Conservative Care Recommendations For The Stages Of Hallux Limitus/Rigidus
Classification systems can be invaluable for directing treatment for hallux limitus/rigidus. Accordingly, these authors recommend a modified classification system that integrates treatment methods and goals with an emphasis on conservative care.
 Despite their perception as two separate entities, hallux limitus and hallux rigidus actually signify different phases of the same pathological process.
Despite their perception as two separate entities, hallux limitus and hallux rigidus actually signify different phases of the same pathological process.
We can clinically define hallux limitus as a biomechanical or structural decrease in the available dorsiflexion of the first metatarsophalangeal joint (MPJ). When there is a longstanding biomechanical limitation of hallux dorsiflexion, the first MPJ responds by slowly developing a progressive osteoarthritis of the joint. This manifests as a loss of dorsal articular cartilage and a hypertrophy of the dorsal aspect of the first metatarsal head.
If this condition continues for several years, hallux rigidus will result. The pathologic process that occurs with hallux limitus is responsible for a reduction in motion and, eventually, pain the patient experiences during the propulsive phase of gait.
There are two phases of hallux limitus that we can clinically differentiate. The earliest stage of first MPJ osteoarthritis is functional hallux limitus, which is characterized by a lack of dorsiflexion during gait. When we examine the joint unloaded, range of motion (ROM) appears normal but a distinct dorsiflexion restriction pattern can be visible via instrumented gait analysis. Vallotton postulated that this occurs when overpronation of the hindfoot leads to excess medial loading, which puts tension on the flexor hallucis longus tendon.1 The flexor hallucis longus tendon passes through a groove in the posterior aspect of the talus, sometimes referred to as the retrotalar pulley. Tension on the tendon during pronation causes it to become functionally shortened, restricting the amount of dorsiflexion available at the first MPJ.
Another theory focuses on dorsiflexion of the medial column.2 If the patient has a flexible medial column that allows for excess dorsiflexion of the first ray during midstance and propulsion, jamming of the first MPJ occurs as the hallux tries to dorsiflex on an elevating first metatarsal head. As the base of the phalanx rides up on the metatarsal head, binding or tightening of the joint occurs. The first metatarsal head has a ginglymus shape similar to the knee and in order for dorsiflexion motion to be unhindered, the metatarsal head must be free to plantarflex as the hallux rises. Early in the development of the condition, the joint is asymptomatic and the patient presents with normal ROM. As the disease progresses, motion decreases and pain develops with each step.
Structural hallux limitus is different from the functional form due to the onset of joint stiffness and a progressive loss of dorsiflexion ROM from bony and joint capsule adaptations at the first MPJ. The degree of adaptation will worsen over time to the point where no motion is available to the joint and hallux rigidus occurs.3 This often occurs bilaterally and is more common in women.4 Other etiologies include trauma, extrinsic biomechanical factors and a genetic predisposition. The most commonly reported trauma is turf toe, where osteochondral injury leads to arthritic joint changes.5 Hallux limitus/rigidus is the second most common condition affecting the big toe after hallux valgus.6 Further, it is the most common arthritic condition of the foot.7
What To Look For When Patients Present With Hallux Limitus/Rigidus
Sufficient dorsiflexion at the first MPJ is essential for normal ambulation.2 In a normal individual, the appropriate motion at the first MPJ should be 65 to 75 degrees of dorsiflexion with respect to the weightbearing surface during the propulsive phase of gait.8 There is a broad spectrum of clinical symptoms and radiographic findings that depend upon the degree of osteoarthritic changes that occur with this condition.
 In the early stages, hallux limitus presents as a reduction in dorsiflexion at the first MPJ during gait only. However, as the available dorsiflexion at the MPJ decreases, the joint begins to jam during propulsion. The patient then experiences pain and joint stiffness, which may lead to further decreases in motion since the patient begins to compensate during gait to relieve the stress on the painful area. The patient may describe the pain as aching, which generally worsens with activity and generally dissipates with rest.9 The motion at the first MPJ continues to decrease as the osteoarthritis progresses, which leads to further osteophyte formation dorsally, medially and laterally as well as significant joint space narrowing.
In the early stages, hallux limitus presents as a reduction in dorsiflexion at the first MPJ during gait only. However, as the available dorsiflexion at the MPJ decreases, the joint begins to jam during propulsion. The patient then experiences pain and joint stiffness, which may lead to further decreases in motion since the patient begins to compensate during gait to relieve the stress on the painful area. The patient may describe the pain as aching, which generally worsens with activity and generally dissipates with rest.9 The motion at the first MPJ continues to decrease as the osteoarthritis progresses, which leads to further osteophyte formation dorsally, medially and laterally as well as significant joint space narrowing.
Patients with symptomatic hallux limitus or rigidus can be severely restricted in ambulation due to pain at the first MPJ. This may cause them to attempt to walk in a supinated position (low gear push off), shorten their stride and avoid propulsion, externally rotate their hip to push off the medial aspect of the joint, or even avoid performing daily activities of living, decreasing their quality of life.7 Treatment options, therefore, should focus on decreasing pain and improving quality of life.
While there are a vast number of surgical options for hallux limitus/rigidus, there are also many conservative measures that can alleviate pain and prevent further joint destruction. Conservative treatment options include shoe modifications, foot orthoses, physical therapy, oral non-steroidal anti-inflammatory drugs (NSAIDs) and intra-articular steroid injections.
In one study by Grady and colleagues, over half of patients with symptomatic hallux limitus had successful treatment with conservative measures, and 47 percent had successful treatment with foot orthoses alone.10 Further, the invasiveness of surgical procedures presents increased risks (e.g. infection, delayed union or non-union, weight transfer to second toe leading to further pathology) and extended recovery times for the patient, which one can avoid by the use of conservative treatments. Therefore, one should consider surgical measures only in cases of recalcitrant hallux rigidus.
Adding Recommended Treatment Options To The Staging Of The Coughlin And Shurnas Classification System
The exact type of treatment that is appropriate for a patient with hallux limitus or rigidus depends greatly on the stage of joint destruction as determined by the clinical and radiographic findings. Similarly, the treatment goals for each stage vary. There are many classification systems for hallux limitus/rigidus but to date, there is no agreed upon gold standard.8 Furthermore, none of these systems incorporate intervention options, conservative or otherwise, into the staging.
We believe the most comprehensive and useful of the classification systems is the one developed by Coughlin and Shurnas.11 This system distinguishes between available ROM at the first MPJ, clinical symptoms and radiographic findings. In one study by Beeson and coworkers, the authors speculated that the Coughlin and Shurnas system had the greatest potential to be a gold standard for classification of hallux rigidus.12 However, this system, like all of the others for hallux limitus/rigidus, does not include an appropriate treatment plan for each stage of disease.
Due to the complex and variable nature of the presentation of first MPJ osteoarthritis, we believe that the inclusion of treatment plans and goals into a classification system, such as the Coughlin and Shurnas system, would give the patient’s healthcare team a simplified and standardized method to provide conservative intervention.11
 The use of some conservative approaches, such as physical therapy and NSAIDs, are generally appropriate regardless of the hallux limitus/rigidus staging, and are therefore not mentioned in the following proposed classification system. However, shoe modifications and orthotic devices will vary with staging, and are therefore included in the tailored treatment plan for each stage (see the table “A Closer Look At A Modified Classification System For Hallux Limitus/Rigidus” on page 51).
The use of some conservative approaches, such as physical therapy and NSAIDs, are generally appropriate regardless of the hallux limitus/rigidus staging, and are therefore not mentioned in the following proposed classification system. However, shoe modifications and orthotic devices will vary with staging, and are therefore included in the tailored treatment plan for each stage (see the table “A Closer Look At A Modified Classification System For Hallux Limitus/Rigidus” on page 51).
The treatment plans that follow are by no means the only treatments that one can use as the clinical picture of each patient will be different. However, it provides a guideline upon which to base the patient’s overall therapy.
Addressing Stage 0 Hallux Limitus
Stage 0. In this stage, there is no radiographic evidence of joint destruction and the patient does not experience pain during full ROM.11 However, there is some joint stiffness present and only 40 to 60 degrees of dorsiflexion is evident upon examination. This stage most closely represents functional hallux limitus.
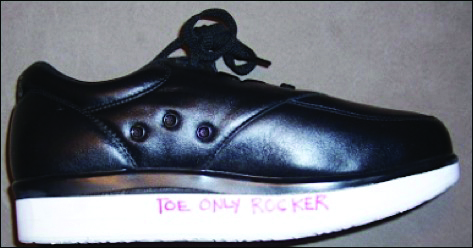
Our goal for patients in this stage is to increase the motion at the first MPJ and attempt to return the individual to his or her full potential ROM. In order to do this, we would suggest the use of a neutral position foot orthosis with a first ray cutout to allow for normal plantarflexion of the first metatarsal during propulsion. It is imperative to facilitate utilization of all of the cartilage covering the metatarsal head. When the proximal phalanx begins to lose articulation with the dorsal metatarsal head, it can lead to cartilage atrophy and faster progression of the deformity. Patients can utilize standard footwear in this stage but rocker style sole designs may provide additional relief.
Keys To Treating Stage 1 Hallux Limitus
Stage 1. In stage 1 of the classification system, only 30 to 40 degrees of dorsiflexion is available for the hallux to dorsiflex passively.11 Furthermore, we begin to see dorsal spurring radiographically with minimal narrowing of the joint space. The patient consequently begins to experience slight pain but usually only at the end range of motion and not consistently. These clinical and radiographic findings correspond to early structural hallux limitus.
The goal of treatment should be to increase motion at the great toe joint before shifting our focus to pain reduction. With less than half of the motion lost at the joint, a first ray cutout will once again be useful to attempt to allow for full ROM at the first MPJ. Shoe gear for this patient would include a shoe with a high toe box, which will also prevent direct contact between the dorsal osteophyte and the shoe, and a stiff, commercial rocker style sole, particularly if the first ray cutout increases pain at the joint.
Footwear And Orthotic Recommendations For Stage 2 Hallux Limitus
Stage 2. In stage 2, there is a more dramatic loss in dorsiflexion at the first MPJ (10 to 30 degrees of dorsiflexion remaining), which can make ambulation both difficult and painful.11 On radiographs, we again see dorsal osteophytes but they will be more extensive than in stage 1, and there will be a further decrease in joint space. While this stage still represents a structural hallux limitus, the severity of joint destruction at this point in the progression of the disorder necessitates a different approach to treatment than the previous stages. Instead of attempting to increase motion, which would continue to cause the patient pain, we would like to limit the remaining motion available at the joint.
The goal of this intervention is to control pain. In order to do this, we recommend implementing a neutral position orthotic device with a rigid shank shoe and a rocker sole. For the orthotic, the clinician can incorporate a modification of the Morton’s extension, which one would use for a structurally elevated first metatarsal. A rigid continuation of the medial shell of the orthotic that extends to the distal hallux can restrict motion and can be a substitute for adding a rigid shank to the shoe.13 This rigid beam decreases the motion available at the arthritic hallux joint and reduces the pain that is experienced with motion. This orthotic modification can allow the patient to ambulate comfortably without pain or compensation.
 Reviewing The Options For Stage 3 And Stage 4 Hallux Rigidus
Reviewing The Options For Stage 3 And Stage 4 Hallux Rigidus
Stage 3. In stage 3, the patient has lost nearly all motion in the first MPJ (less than 10 degrees of dorsiflexion remaining) and movement of the joint to end range causes the patient significant pain.11 Joint space narrowing is substantial and the sesamoids may be affected. This stage would correspond to a hallux rigidus by definition.
The most effective conservative treatment at this point is to reduce all motion at the osteoarthritic joint and completely immobilize the first MPJ. One can accomplish this with a rigid shank shoe with a custom-made rocker sole to match the patient’s angle and speed of ambulation. The apex of the rocker sole should be just proximal to the metatarsal heads in order to mimic the normal characteristics of the foot’s movement. Depending on the stride length, the angle of the rocker may require the addition of a thicker sole on both shoes. Even if pathology is only on one side, it is often helpful to add rockers to both shoes to even out the patient’s gait and prevent symptoms from developing on the asymptomatic side.
Due to the severity of joint destruction at this stage, surgical solutions may become attractive choices. Surgically, one may fuse the joint to decrease all motion and therefore eliminate pain, or use an implant to essentially replace the joint.14
Stage 4. This stage is similar to the previous stage, except that any motion at the first MPJ causes the patient pain.11 In this situation, total immobility or replacement of the joint is warranted. One can place this individual in a rigid, rocker-soled shoe as we described above to aid in keeping this joint immobile. Conservative treatment at this stage is most likely going to be more of a temporary fix as the joint autofuses, has surgical fusion or one replaces it with an implant.
The decision to perform surgery, however, should be based on the patient’s age, activity level and overall goals of recovery. If the patient refuses surgery or is not a good surgical candidate, limiting forward excursion of the tibia with the use of a molded ankle foot orthosis may help in restoring a comfortable ambulatory state for the patient.
In Conclusion
Due to the prevalence of hallux limitus/rigidus among our patient population, it is crucial to have a simple, standardized method of classifying, diagnosing and treating the various stages of hallux limitus and rigidus. While there are many systems, there is currently no classification system for this deformity that integrates conservative treatment goals and plans with clinical and radiographic findings.
By proposing an integrated classification system, we hope to achieve better outcomes with conservative treatment prior to considering surgical options. As physicians, we owe our patients the highest standard of care, which involves exhausting conservative approaches before bringing a patient into the operating room. Implementing these shoe modifications and foot orthosis prescriptions at each stage of hallux limitus/rigidus will give our patients the best chance to maintain their quality of life.
Ms. Miner is a fourth-year student at the Temple University School of Podiatric Medicine.
Dr. Foote is a first-year resident at University of Florida Health in Jacksonville, Fla.
Dr. Cheskis is a first-year resident at NYU Langone Hospital in Brooklyn, NY.
Dr. McGuire is a Clinical Associate Professor in the Departments of Podiatric Medicine and Podiatric Biomechanics at the Temple University School of Podiatric Medicine. He is the Director of the Leonard S. Abrams Center for Advanced Wound Healing in Philadelphia.
References
- Vallotton J, Echeverri S, Dobbelaere-Nicolas V. Functional hallux limitus or rigidus caused by a tenodesis effect at the retrotalar pulley. J Am Podiatr Med Assoc. 2010; 100(3):220-229.
- Hild GA, McKee PJ. Evaluation and biomechanics of the first ray in the patient with limited motion. Clin Podiatr Med Surg. 2011; 28(2):245-267.
- Clough JG. Functional hallux limitus and lesser-metatarsal overload. J Am Podiatr Med Assoc. 2005; 95(6):593-601.
- Shurnas PS. Hallux rigidus: etiology, biomechanics, and nonoperative treatment. Foot Ankle Clin. 2009; 14(1):1–8.
- Kunnasegaran R, Thevendran G. Hallux rigidus. Foot Ankle Clin. 2015; 20(3):401-412.
- Moberg E. A simple operation for hallux rigidus. Clin Orthop. 1979; 142:55-56.
- Veillette C. Hallux rigidus. OrthopaedicsOne. Available at https://www.orthopaedicsone.com/x/EgCSAg . Published June 6, 2010.
- Botek G, Anderson MA. Etiology, pathophysiology, and staging of hallux rigidus. Clin Podiatr Med Surg. 2011; 28(2):229-243.
- Julien, PH and Dowling LB. Non-surgical and surgical management of hallux limitus in the athlete. In The Podiatry Institute Update Chapters. Podiatry Institute, Tucker, GA. Chapter 9, 2012.
- Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc. 2002; 92(2):102–108.
- Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003; 85-A(11):2072-2088.
- Beeson P, Phillips C, Corr S, Ribbans W. Classification systems for hallux rigidus: a review of the literature. Foot Ankle Int. 2008; 29(4):407–414.
- Rosenbloom KB. Pathology-designed custom molded foot orthoses. Clin Podiatr Med Surg. 2011; 28(1):171-187.
- Esway JE, Conti SF. Joint replacement in the hallux metatarsophalangeal joint. Foot Ankle Clin. 2005; 10(1):97-115.











