Can A Hybrid Imaging Technology Be Beneficial In Diagnosing And Monitoring Diabetic Foot Osteomyelitis?
The global prevalence of diabetes mellitus is rising with a global estimate of 366 million people diagnosed with the disease in 2011 and expert predictions that 552 million individuals will be diagnosed with diabetes worldwide by 2030.1
 Epidemiological data has previously shown that 40 to 60 percent of all non-traumatic lower extremity amputations are in patients with diabetes and foot ulcers precede 85 percent of these amputations.1 The economic and social impact of having an ulcer is not negligible as foot problems account for the largest number of hospital bed days for patients with diabetes as well as considerable morbidity.1 This translates into poor functional outcomes. Researchers estimate that 77 percent of patients older than 75 undergoing amputation in the United States do not return to independent living.2
Epidemiological data has previously shown that 40 to 60 percent of all non-traumatic lower extremity amputations are in patients with diabetes and foot ulcers precede 85 percent of these amputations.1 The economic and social impact of having an ulcer is not negligible as foot problems account for the largest number of hospital bed days for patients with diabetes as well as considerable morbidity.1 This translates into poor functional outcomes. Researchers estimate that 77 percent of patients older than 75 undergoing amputation in the United States do not return to independent living.2
The pathophysiology of the diabetic foot has previously been well elucidated with researchers identifying neuropathy and microvascular complications as factors leading to destruction of the fat pad.2 This process increases the risk of ulceration, which may then lead to infection of the underlying bone.
The management of patients with diabetic foot osteomyelitis remains a challenge for the clinician as there is little evidence-based data guiding care in our current practice. The Infectious Diseases Society of America (IDSA) guidelines recommend obtaining bone or deep tissue specimens for pathology and microbiology studies, allowing the physician to tailor antimicrobial therapy to pathogens recovered from cultures.3 Assessing the response to therapy remains difficult and clinicians rely largely on physical exam findings and trends in erythrocyte sedimentation rate/C-reactive protein (ESR/CRP), which are non-specific markers of inflammation.
After establishing the diagnosis of bone infection with X-ray or magnetic resonance imaging (MRI), my patients receive a minimum of six weeks of intravenous and/or oral antimicrobial therapy in addition to surgical debridement. This is based largely on anecdotal experience. One can also use highly bioavailable oral antibiotics in some cases of diabetic foot osteomyelitis. At least four to six weeks of therapy is required and probably longer if infected bone remains.3
Over the last 15 years, cross-sectional imaging modalities such as computed tomography (CT) and MRI have become popular diagnostic methods in part because of their high anatomical resolution.
One can use MRI to evaluate non-specific edema. It has modest cortex resolution and remains positive for long periods of time so serial measures to evaluate the resolution of infections are not possible. There is a concern that MRIs can lead to overdiagnosis of diabetic foot osteomyelitis because of prolonged bone marrow edema in patients with foot surgery, trauma or Charcot arthropathy.4-6 In the diabetic foot, Charcot joint (5 percent) and previous surgery (40 percent) are common, rendering MRI with questionable diagnostic value. The sensitivity of MRI is consistently high but the specificity and positive predictive values are variable.7 In some studies, the specificity and positive predictive value of MRI are about the same as flipping a coin.8-12
There are several common shortcomings in the “MRI osteomyelitis” literature. Most published papers consist of small cohorts (less than 40 osteomyelitis cases). Few studies report long-term clinical follow-up or confounding variables such as peripheral perfusion, recent surgery, Charcot arthropathy, antibiotic treatment history or comorbidities.
Investigating The Potential Of SPECT-CT Imaging
In our hospital, we have been increasingly using nuclear medicine with high-specificity single photon emission computed tomography (SPECT-CT) of 99mTc labeled white blood cells to establish the diagnosis of diabetic foot osteomyelitis due to the technology’s improved sensitivity and specificity in comparison to MRI.13 Despite appropriate antimicrobial therapy, radiologic and MRI changes can worsen for several weeks and “lag” behind clinical signs and symptoms that may be consistent with overall improvement. The SPECT-CT imaging may be the imaging technique of choice to monitor the response of therapy for diabetic foot osteomyelitis. The SPECT-CT is a new hybrid imaging technology that combines radiolabeled white blood cells and high resolution X-ray CT.
The advantages of SPECT-CT include:
1. Superior anatomic and spatial resolution
2. Few false positives from trauma, fracture or previous surgery
3. Provides an infection severity score to predict clinical outcomes
4. Ability to monitor response to therapy and determine when osteomyelitis treatment has been successful
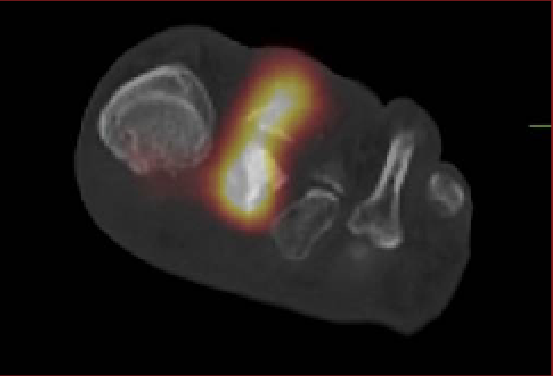
The SPECT-CT combines nuclear medicine tagged white blood cells (WBC) with the three-dimensional imaging of CT so the clinician can see subtle differences in the magnitude and penetration of tagged WBC in soft tissue and bone.
In our preliminary study, we assessed the accuracy of hybrid image 99mTc labeled WBC SPECT/CT for diagnosing diabetic foot osteomyelitis as determined by bone biopsy results in comparison to MRI. We retrospectively reviewed 166 patients who received a bone biopsy from 2010 to 2013. The study excluded patients whose scan(s) were not within a clinically relevant timeframe of biopsy, which we determined to be eight weeks. Patients who received both MRI and SPECT/CT within a clinically relevant timeframe were included in both groups.
Our data suggested that SPECT-CT is not inferior to MRI in the diagnosis of diabetic foot osteomyelitis. Furthermore, SPECT-CT results correlate well with the bone biopsy results.
Case Study: When SPECT-CT Can Help Direct Antibiotic Therapy
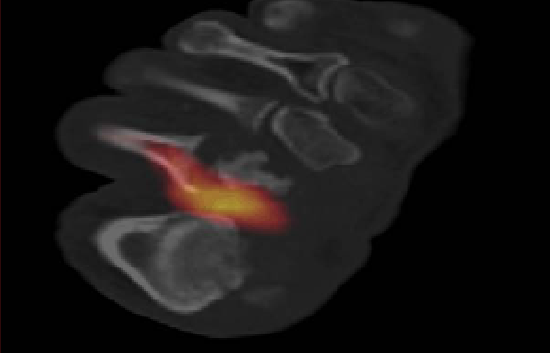 This case represents an example in how this hybrid technique may be useful monitoring response to therapy. A 46-year-old male with diabetes presented to our clinic with the diagnosis of diabetic foot osteomyelitis.
This case represents an example in how this hybrid technique may be useful monitoring response to therapy. A 46-year-old male with diabetes presented to our clinic with the diagnosis of diabetic foot osteomyelitis.
He had refused surgery since the time of presentation. An infectious disease physician was involved to evaluate the patient for a long-term antibiotic regimen.
Initial Tc-99m WBC SPECT/CT demonstrated osteomyelitis of the second metatarsal head with additional involvement of the second proximal phalanx. Sequential SPECT/CT scans at two-month clinical intervals showed improvement of osteomyelitis followed by the resolution of infection after prolonged antibiotic therapy. This allowed physicians to determine when it was the proper time to stop antibiotic therapy.
In Conclusion
Diagnostic imaging has long played a major role in the investigation of suspected osteomyelitis. When interpreting the literature on performance characteristics of different radiographic tests, it is important to remember that osteomyelitis is a heterogeneous condition. It is also important to be clear on what clinical entity (e.g., acute or chronic osteomyelitis, presence or absence of neuropathic changes) you are assessing with the particular modality. It is critical to interpret any individual patient’s imaging results in light of the clinical situation, considering what patient-specific features may interfere with the test’s reported sensitivity and specificity. Given the less than perfect performance characteristics, one should view the role of diagnostic imaging as confirming the presumed clinical diagnosis and providing information regarding the exact site and extent of infection.14
As with most tests, no technique can absolutely confirm or exclude the diagnosis. All results need careful interpretation in light of the clinical findings. Imaging studies provide information that supports or refutes the clinical suspicion with variable certainty.
Dr. La Fontaine is the Associate Professor of the Department of Plastic Surgery at the University of Texas Southwestern Medical Center in Dallas. He is a Fellow of the American College of Foot and Ankle Surgeons, and the American Society of Podiatric Surgeons.
References
1. Bakker K, Schaper NC. The development of global consensus guidelines on the management and prevention of the diabetic foot 2011. Diabetes Metab Res Rev. 2012;28(Suppl 1):116-8
2. Ramsey SD, Newton K, Blough D, et al. Incidence, outcomes and cost of foot ulcers in patients with diabetes. Diabetes Care. 1999;22(3):382-387
3. Lipsky BA, Berendt RA, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):132-173
4. Baker JC, Demertzis JL, Rhodes NG, et al. Diabetic musculoskeletal complications and their imaging mimics. Radiographics. 2012; 32(7):1959-74.
5. Chatha DS, Cunningham PM, Schweitzer ME. MR imaging of the diabetic foot: diagnostic challenges. Radiol Clin North Am. 2005; 43(4):747-59, ix.
6. Ledermann HP, Morrison WB. Differential diagnosis of pedal osteomyelitis and diabetic neuroarthropathy: MR imaging. Semin Musculoskelet Radiol. 2005; 9(3):272-83.
7. Lavery LA, Armstrong DG, Wunderlich RP, et al. Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care. 2003; 26(5):1435-8.
8. Newman LG, Waller J, Palestro CJ, et al. Leukocyte scanning with 111In is superior to magnetic resonance imaging in diagnosis of clinically unsuspected osteomyelitis in diabetic foot ulcers. Diabetes Care. 1992; 15(11):1527-30.
9. Seabold JE, Flickinger FW, Kao SC, et al. Indium-111-leukocyte/technetium-99m-MDP bone and magnetic resonance imaging: difficulty of diagnosing osteomyelitis in patients with neuropathic osteoarthropathy. J Nucl Med. 1990; 31(5):549-56.
10. Craig JG, Amin MB, Wu K, et al. Osteomyelitis of the diabetic foot: MR imaging-pathologic correlation. Radiology. 1997; 203(3):849-55.
11. Nawaz A, Torigian DA, Siegelman DS, et al. Diagnostic performance of FDG-PET, MRI, and plain film radiography (PFR) for the diagnosis of osteomyelitis in the diabetic foot. Mol Imaging Biol. 2010; 12(3):335-42.
12. Ertugrul MB, Baktiroglu S, Salman S, et al. The diagnosis of osteomyelitis of the foot in diabetes: microbiological examination vs. magnetic resonance imaging and labelled leucocyte scanning. Diabet Med. 2006; 23(6):649-53.
13. Lew DP, Waldvogel FA. Osteomyelitis. N Engl J Med. 1997; 336(14):999–1007.
14. Mader JT, Shirtliff M, Calhoun JH. Staging and staging application in osteomyelitis. Clin Infect Dis. 1997;25(6):1303–9.
For an enhanced experience, check out Podiatry Today on your iPad or Android tablet.











