Are Uterine Fibroids A Risk Factor For Plantar Fibroma Recurrence?
Offering insights from an intriguing retrospective review, these authors examine a potential correlation between uterine fibroids and plantar fibromatosis.
Plantar fibromatosis is not uncommon in the lower extremity. It is a benign fibrous disorder of unknown etiology, most commonly involving the medial and central bands of the plantar aponeurosis.1,2 First described by Ledderhose in 1897, plantar fibromatosis can be associated with Ledderhose disease along with other disorders such as Peyronie’s disease or Dupuytren’s contracture.2,3
The primary treatment for plantar fibromas is surgical resection. However, there is a high recurrence rate, reportedly ranging between 30 to 80 percent, and this is the most common complication associated with the procedure.3 However, De Bree and colleagues note that wide resection decreases the likelihood of developing new plantar fibromas.3
Fibromatosis in general is a proliferative disorder, which can present in various areas of the body such as the abdominal wall, genitalia, the hand and the lower extremities.4 In our practice, we observed that plantar fibromas tend to affect women with uterine fibroids more frequently, especially in patients with recurring plantar fibromas. Therefore, the purpose of this study is to identify whether uterine fibroids are a risk factor for the recurrence of plantar fibromas after surgical resection. The authors of this study hypothesize that the presence of uterine fibroids increases the likelihood of a patient also having recurrent plantar fibromas.
What Our Retrospective Study Revealed
We performed a retrospective review of patients from multiple foot and ankle surgeons at a large teaching institution using ICD-9 and ICD-10 codes for plantar fibromas (728.71 and M72.2 respectively) from January 2007 to July 2017. We reviewed outpatient charts, inpatient charts, hospital operative records and pathology reports to confirm the diagnosis of plantar fibromatosis. We also reviewed each chart to identify whether the patient had a recurrence of plantar fibroma following surgical excision.
During the data collection, we made a special notation for each female patient who had a known diagnosis of uterine fibroids. We excluded patients from the study if they did not have an outpatient chart associated with the primary institution in order to eliminate those who received health care from two different institutions. Out of the patients who had surgery for plantar fibromas, a total of 24 patients with plantar fibromatosis met the study inclusion criteria. We also gathered patient demographic information including gender, age, history of tobacco usage and history of diabetes mellitus. Eleven of the 24 patients had uterine fibroids.
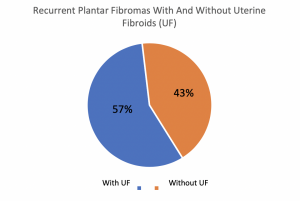
Within the plantar fibroma group, 79 percent (19/24) of patients were African-American, 17 percent (4/24) were Caucasian, and 4 percent (1/24) were Hispanic. All 24 patients were female with a mean age of 56 years and with plantar fibroma diagnosis confirmed via postoperative pathology report. Eleven (46 percent) of the 24 plantar fibroma patients had a diagnosis of uterine fibroids. Likewise, seven (19 percent) out of the 24 patients with plantar fibromas had a recurrence after surgical excision. Four (57 percent) out of those seven patients had a concurrent diagnosis of uterine fibroids whereas three (43 percent) of the seven patients did not have uterine fibroids.

What Conclusions Can We Draw From This Data?
Similar to plantar fibromatosis, little is known about the etiology of uterine fibroids. Reports estimate the incidence and prevalence of uterine fibroids to be higher in African-American women of all ages.5 Family history and genetics are key players in underlying systemic fibromatosis. We were particularly curious about the link between the two disorders given the findings at our institution.
The data generated in this study demonstrates that patients who had uterine fibroids were more likely to have plantar fibroma recurrence after excisional debridement than those without uterine fibroids. In our study, 46 percent of patients with a plantar fibroma also had uterine fibroids but this number increased to 57 percent for patients who had uterine fibroids and plantar fibroma recurrence.
A limitation of this study is that we identified our population utilizing ICD-9 and ICD-10 codes that could indicate either plantar fasciitis or plantar fibromatosis. This could artificially elevate the overlap between the two diagnoses. However, this is why we chose to investigate the recurrence of plantar fibromatosis with uterine fibroids. If we were able to look at the two populations separately, we could form a true association.
Our study attempted to determine whether there is an association between plantar fibromatosis and uterine fibroids. This data may also be beneficial in providing foot and ankle surgeons with expectations regarding the likelihood of plantar fibroma reoccurrence after surgical excision and may provide further clarity on both plantar fibromas and uterine fibroids. As with any scientific investigation, we encourage critical readers to review the study design and results, and reach their own conclusions. As scientists, we never consider data to be definitive but do think that these results are worthy of attention and future investigation.
Final Thoughts
In addition, these results suggest that uterine fibroids possibly increase the likelihood of developing a plantar fibroma. It is our hope that the results of this investigation add to the body of knowledge regarding this subject and lead to future investigations into the progression, evaluation and treatment of plantar fibromatosis.
Dr. Magodia is a third-year resident at the Temple University Hospital Podiatric Surgical Residency Program in Philadelphia.
Dr. Hasenstein is in private practice in Columbus, Ind. and is a recent graduate of the Temple University Hospital Podiatric Surgical Residency Program.
Dr. Pontious is a Clinical Associate Professor in the Department of Podiatric Surgery at Temple University School of Podiatric Medicine in Philadelphia. She is a Fellow of the American College of Foot and Ankle Surgeons.
1. Hafner S, Han N, Pressman MN, Wallace C. Proximal plantar fibroma as an etiology of recalcitrant plantar heel pain. J Foot Ankle Surg. 2011;50(2):153-157.
2. Carrol P, Henshaw R, Garwood C, Raspovic K, Kumar D. Plantar fibromatosis: pathophysiology, surgical and nonsurgical therapies. An evidence-based review. Foot Ankle Spec. 2018;11(2):168-175.
3. De Bree E, Zeotmulder FAN, Keus R, Peterse H, Coevorden F. Incidence and treatment of recurrent plantar fibromatosis by surgery and postoperative radiotherapy. Am J Surg. 2004;187(1):33-38.
4. Zgonis T, Jolly G, Polyzois V, Kanuck D, Stamatis E. Plantar fibromatosis. Clin Podiatr Med Surg. 2005;22(1):11-18.
5. Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35(6):474-480.
Additional References
6. Fuiani M, Mosca M, Caravelli S, et al. Current concepts about treatment options of plantar fibromatosis: A systematic review of the literature. Foot Ankle Surg. 2018;25(5):559-564.
7. Aluisio FV, Mair SE, Hall RL. Plantar fibromatosis: treatment of primary and recurrent lesions and factors associated with recurrence. Foot Ankle Int. 1996;17(11):672-678.


















