Addressing Myths And Misconceptions About Hallux Rigidus
 Citing emerging insights from the literature, this author raises questions about the pathomechanics of hallux rigidus, challenges perceptions about the involvement of metatarsus primus elevatus and first ray hypermobility, and says pain reduction may be the ultimate goal in facilitating optimal, long-term outcomes.
Citing emerging insights from the literature, this author raises questions about the pathomechanics of hallux rigidus, challenges perceptions about the involvement of metatarsus primus elevatus and first ray hypermobility, and says pain reduction may be the ultimate goal in facilitating optimal, long-term outcomes.
The management of hallux rigidus remains a daunting and elusive challenge for the podiatric physician. While conservative management of this disorder may minimize symptoms, it will not slow down progression of the pathology. At the same time, surgical options for hallux rigidus have among the poorest prognoses for long-term success in comparison to all other elective foot surgeries. This quandary puts the treating podiatric physician in a position of choosing the least of all evils among available treatment options.
Almost from the day that hallux rigidus was first described, a number of myths and misconceptions have emerged regarding the etiology of the disorder. At the top of the list are the notions of hypermobility of the first ray and metatarsus primus elevatus. These two clinical findings often lead surgeons to make important decisions about how they will treat patients with hallux rigidus. However, recent research has questioned whether first ray mobility or position has any relevance in the etiology or treatment of hallux rigidus.
Accordingly, let us take a closer look at the recent research and expose some myths about the etiology and treatment of hallux rigidus. Newer insights may give us better options for decision making by the podiatric surgeon.
Redefining Hallux Rigidus
Cotterill first used the term hallux rigidus in 1888 to describe stiffness of the great toe joint.1 Later, hallux rigidus became associated with degenerative arthritis of the first metatarsophalangeal joint (MPJ).2 This condition is often inappropriately labeled hallux limitus, which refers only to a functional limitation of first MPJ motion in the absence of degenerative arthritis.3
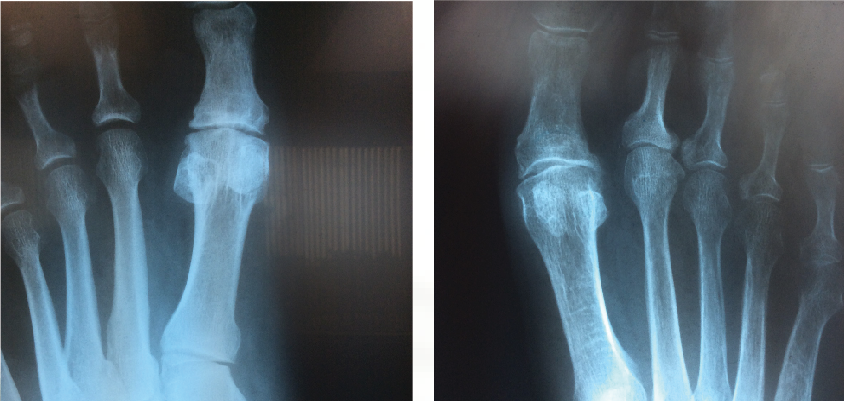 The symptoms of hallux rigidus include pain with range of motion of the first MPJ, swelling around this joint and pain with irritation from footwear.4 Physical examination reveals bone enlargement and restricted motion of the first MPJ.5 Radiographic findings of hallux rigidus include joint space narrowing of the first MPJ, osteophyte formation, subchondral sclerosis, flattening of the first metatarsal head, trumpeting of the base of the proximal phalanx and loose bodies.6,7
The symptoms of hallux rigidus include pain with range of motion of the first MPJ, swelling around this joint and pain with irritation from footwear.4 Physical examination reveals bone enlargement and restricted motion of the first MPJ.5 Radiographic findings of hallux rigidus include joint space narrowing of the first MPJ, osteophyte formation, subchondral sclerosis, flattening of the first metatarsal head, trumpeting of the base of the proximal phalanx and loose bodies.6,7
Many different authors have described staging the severity of hallux rigidus. Beeson and coauthors identified 18 classification systems for hallux rigidus and concluded there is a need for more objective criteria based upon sound scientific research.8 This is evidenced by the fact that the most commonly used classification systems rely on terms such as “mild or moderate pain” or “mild or moderate” restriction of joint range of motion to describe hallux rigidus. Clinicians would disagree in their assessment of “minor” or “moderate” joint space narrowing of the first MPJ.
In terms of “normal” parameters of first MPJ range of motion, we now know our long held theory of 65 degrees dorsiflexion or extension being a minimal requirement is incorrect. Nawoczenski has determined that healthy people only require about 40 degrees of dorsiflexion of the hallux at the first MPJ during normal walking gait.9 We would already consider this to be an early stage of hallux rigidus according to previous classification systems.10,11 Nawoczenski also demonstrated that the current standard measurement of first MPJ joint range of motion with the patient seated non-weightbearing is not an accurate predictor of the actual motion the same patient uses in walking gait. Instead, having the patient stand and actively extend the hallux demonstrates the true range of motion that the patient uses during walking.9
Controversies In The Pathomechanics Of Hallux Rigidus
Other than plantar heel pain syndrome, no other condition affecting the human foot has more misunderstanding about its etiology than hallux rigidus. While many clinicians have learned that abnormal foot mechanics and variations of foot skeletal alignment are key contributing factors, a closer look at scientific evidence will reveal conflicting information.
Two oft quoted etiologic factors for hallux rigidus include hypermobility of the first ray as well as metatarsus primus elevatus. While both factors deserve closer scrutiny, one must first realize that they are two very different entities that we often erroneously combine together as the same clinical condition.
Morton first proposed the term “hypermobility” of the first ray of the human foot in 1926.12 However, this condition in theory contributed to metatarsalgia and arch instability with no mention made about first MPJ mechanics. Jack was the first to describe a jamming mechanism of the great toe joint when the first ray was dorsiflexed or pushed abnormally into extension.13 Later, Roukis and coworkers demonstrated that an elevation of the first metatarsal by only 4 mm would decrease dorsal range of motion of the first MPJ by almost 20 percent.14 However, confusion has arisen regarding the assumption that a so-called “hypermobile” first ray, measured off–weightbearing, would dorsiflex inappropriately during the gait cycle and lead to jamming of the first MPJ. The fact is that this phenomenon of first ray hypermobility and jamming of the first MPJ in gait has never had testing, measurement or validation.
The term metatarsus primus elevatus, which describes when the first metatarsal is elevated relative to the remaining metatarsals, originated with Lambrinudi in 1938.15 He was the first to describe this deformity, which was considered a hereditary causative force in the development of hallux rigidus. Subsequently, Bonney and Macnab observed metatarsus primus elevatus in two-thirds of all patients with hallux rigidus but could not determine if the finding was the cause rather than the result of the painful condition.16 Notwithstanding, the literature describes at least 10 different surgical procedures and surgeons continue to utilize them to correct the static deformity known as metatarsus primus elevatus.17
Do Metatarsus Primus Elevatus And First Ray Hypermobility Cause Hallux Rigidus?
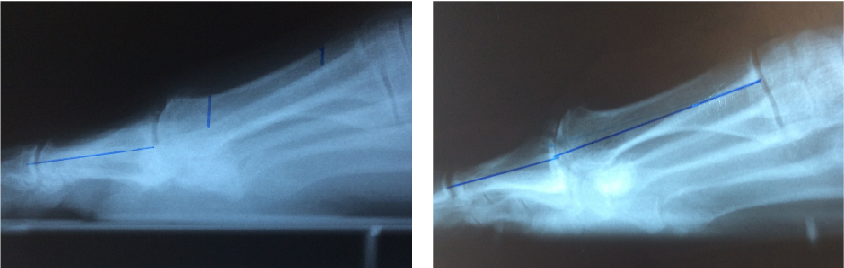
Metatarsu s primus elevatus is basically a radiographic finding that theoretically depicts the position of the first metatarsal relative to the lesser metatarsals at the midstance phase of the gait cycle.18 In metatarsus primus elevatus, the first metatarsal is elevated to an abnormal position. However, there is no agreement as to the degree that this elevation is truly “abnormal” or pathologic. Some authors have noted that metatarsus primus elevatus can be present in normal, healthy feet with no evidence of hallux rigidus.19
s primus elevatus is basically a radiographic finding that theoretically depicts the position of the first metatarsal relative to the lesser metatarsals at the midstance phase of the gait cycle.18 In metatarsus primus elevatus, the first metatarsal is elevated to an abnormal position. However, there is no agreement as to the degree that this elevation is truly “abnormal” or pathologic. Some authors have noted that metatarsus primus elevatus can be present in normal, healthy feet with no evidence of hallux rigidus.19
Many authors have connected metatarsus primus elevatus as a causative factor for hallux rigidus. Meyer reviewed radiographs of 120 patients and found that hallux rigidus findings did correlate with the presence of metatarsus primus elevatus.20 Roukis determined the mean first to second metatarsal elevation to be 5.8 mm in a hallux rigidus group, which was higher than in patients with other foot pathologies.21 Bouaicha and coworkers attempted to standardize techniques to measure alignment of the first metatarsal on lateral radiographs and found that elevation of the first metatarsal greater than 5 mm was predictive of hallux rigidus.17
The fact that hallux rigidus and metatarsus primus elevatus seem to go together when looking at lateral radiographs reaffirmed the long held notion that hypermobility and elevation of the first ray must be a primary cause of hallux rigidus. However, two studies have raised the question about whether such a cause-effect relationship really exists. Horton and coworkers studied radiographs of patients with and without hallux rigidus, and found no difference in alignment of the first ray between the two groups.18 In cases of severe hallux rigidus, the metatarsus primus elevatus increased significantly, suggesting to the authors that elevation of the first metatarsal occurs as a result of hallux rigidus and not vice versa.
Coughlin and Shurmas studied 110 patients with hallux rigidus and found metatarsus primus elevatus in only 10 cases.22 They also concluded that elevation of the first metatarsal is the result of and not the cause of hallux rigidus. Previously, Coughlin had made a similar observation of the intermetatarsal angle deformity, which increases as hallux abducto valgus deformity increases.23
What The Literature Reveals About Hypermobility And Hallux Rigidus
Over the years, many authorities have attributed a hypermobile first ray as a primary etiology of hallux rigidus.4,11,13,24,25 However, none of these reports provided any specific measurements to confirm their findings. Notwithstanding, numerous authors have proposed surgical procedures that would reduce the perceived hypermobility.26,27
We should now appreciate that static radiographic measures of first ray alignment are not reliable in determining the presence or severity of hallux rigidus. Often, we use the terms metatarsus primus elevatus and first ray “hypermobility” interchangeably, but they are actually different. Metatarsus primus elevatus describes the static position of the first metatarsal head in a weightbearing position of the foot, which somewhat duplicates the midstance phase of gait.
One often assesses hypermobility in the clinical setting by moving the first metatarsal through the sagittal plane and determining the overall range of motion. Greisberg has termed this “translation” of the first ray and points out that this is different than the “elevation” of the first ray, which one determines radiographically.28 However, in his study of metatarsalgia, Greisberg found that the two entities were often linked together.
Root and colleagues have described hypermobility as “any motion occurring at a joint in response to forces which are interacting at a joint at a time when the joint should be stable under such forces.”29 Furthermore, Root states that, “hypermobility of the first ray is a state of abnormal first ray instability that occurs while the forefoot is bearing weight.” Root described a clinical assessment technique to measure excursion of the first ray. This static measurement advocated by Root and coworkers is one that most podiatric physicians employ.29 In this case, the physician holds the plane of metatarsals two through five level and then moves the first metatarsal dorsal and plantar, measuring the range of motion above and below the plane of the lesser metatarsals.
We have determined that such a measurement technique has numerous problems with standardization and reproducibility. Coughlin and coworkers showed that a simple change in ankle position will affect stiffness of the first ray with static measurement off-weightbearing.29
 Due to these shortcomings, several devices have emerged to provide better quantitative measurement of first ray range of motion in the clinical setting. The Glasoe and Klaue devices enable one to measure first ray motion in the sagittal plane while maintaining a stable position of the lesser metatarsals.30,31Researchers have found both devices to be far more accurate in measuring first ray motion and authors have studied the role of dorsal mobility of the first metatarsal and various foot pathologies.32
Due to these shortcomings, several devices have emerged to provide better quantitative measurement of first ray range of motion in the clinical setting. The Glasoe and Klaue devices enable one to measure first ray motion in the sagittal plane while maintaining a stable position of the lesser metatarsals.30,31Researchers have found both devices to be far more accurate in measuring first ray motion and authors have studied the role of dorsal mobility of the first metatarsal and various foot pathologies.32
Coughlin and Shurmas used the Klaue device to measure dorsal mobility of the first metatarsal in 110 patients with hallux rigidus.22 The dorsal excursion of the first metatarsal was 5.8 mm, which was far below the previous 8 mm threshold for hypermobility.31 This is the only study to date to actually measure first ray mobility in patients with hallux rigidus and no correlation existed between hypermobility and this condition.
What Is The Role Of Soft Tissue Constraints In Hallux Rigidus?
If metatarsus primus elevatus is perhaps the result of painful hallux rigidus, what causes the first metatarsal to elevate relative to the lesser metatarsals as is commonly visible on lateral radiographs of patients in later stages of this condition? Recent evidence has suggested an important role of several dynamic soft tissue constraints around the first MPJ.
Bouaicha and coworkers further studied the role of metatarsus primus elevatus and hallux rigidus.17 They observed that some of the conflicting results of previous studies of metatarsus primus elevatus were due to unreliable measurement techniques of radiographs taken of patients with hallux rigidus. Bouaicha and colleagues described a new measurement technique to measure elevation of the first metatarsal relative to the second metatarsal. With this technique, a correlation between metatarsus primus elevatus and hallux rigidus was present, but the authors could not determine the cause-effect relationship.
However, a more interesting finding was reported in the Bouaicha study regarding the position of the hallux relative to the first metatarsal.17 This angular relationship in the sagittal plane, described as the first metatarsal dorsiflexion angle, showed a significant reduction (i.e. plantarflexion) in patients with hallux rigidus. Furthermore, there was a significant correlation with plantarflexion of the hallux and elevation of the first metatarsal in patients with hallux rigidus. The authors speculated that tensioning of the flexor hallucis longus tendon could be responsible for retrograde metatarsus primus elevatus.
Other investigators have proposed the role of the flexor hallucis longus tendon and the pathogenesis of hallux rigidus. In a cadaveric study, Kirane and coworkers showed that reduced excursion of the flexor hallucis longus tendon would significantly alter mechanics of dorsiflexion of the first MPJ.38 They recommended evaluating the flexor hallucis longus for fibrosis or impingement as far proximal as the myotendinous junction in patients with hallux rigidus.
Researchers have long implicated plantar aponeurosis as a contributor to reduced dorsiflexion of the first MPJ.26,29 Phillips and coauthors suggested that pronation of the rearfoot leading to instability of the medial column increases tension in the plantar fascia with subsequent limitation of dorsiflexion of the hallux.34
 While studies showing how improvement of foot alignment can improve first MPJ function are lacking, a very simple demonstration of the role of the plantar fascia in hallux rigidus offers some interesting insight. Harton and coworkers measured a 10 degree increase in passive dorsiflexion of the first MPJ in patients who had plantar fasciotomy for heel pain syndrome.35 While nobody would recommend this procedure as a primary intervention for hallux rigidus, it is interesting to see the role of the plantar fascia on the mechanics of the first MPJ.
While studies showing how improvement of foot alignment can improve first MPJ function are lacking, a very simple demonstration of the role of the plantar fascia in hallux rigidus offers some interesting insight. Harton and coworkers measured a 10 degree increase in passive dorsiflexion of the first MPJ in patients who had plantar fasciotomy for heel pain syndrome.35 While nobody would recommend this procedure as a primary intervention for hallux rigidus, it is interesting to see the role of the plantar fascia on the mechanics of the first MPJ.
Allen and coworkers further elucidated the role of the dynamic soft tissue structures affecting alignment of the first ray during gait with an important gait study on 15 healthy people.36 These researchers theorized that people with higher dorsal mobility of the first metatarsal measured off-weightbearing in a static state would also demonstrate increased dorsal mobility of that segment during walking gait. However, in this study, static measurement of first ray motion did not in any way predict position of the first ray during walking gait. The researchers point out that during walking, numerous dynamic influences from soft tissue structures occur that can reduce hypermobility of the first metatarsal measured in the static, non-weightbearing condition.
During supination of the rearfoot in terminal stance, the peroneus longus plantarflexes and everts the first ray.37 The plantar fascia stabilizes and plantarflexes the first metatarsal via the windlass mechanism.38 Allen and coworkers warned that making conclusions about hypermobility or dorsal excursion of the first ray based upon static measurements would be misleading.36
Emerging Insights On Treatment Goals For Hallux Rigidus
If we have dispelled previous notions about metatarsus primus elevatus and first ray hypermobility, why should surgeons continue to perform plantarflexion osteotomies of the first metatarsal to treat hallux rigidus? If one looks at the literature, outcomes with such procedures are quite favorable.39-41 However, further scrutiny of these articles reveal that the surgeons consistently report that the plantarflexion procedures “decompress” the first MPJ and this may account for some, if not all, of the relief of symptoms. Given the more recent insights about the role of soft tissue structures limiting motion of the first MPJ, it appears that procedures that effectively “lengthen” the soft tissue may help restore normal mechanics.
At the same time, systematic reviews of the medical literature evaluating the efficacy of surgical procedures for treatment of hallux rigidus have consistently shown the same conclusions. Some procedures such as cheilectomy and arthrodesis are primarily designed to relieve pain. Other procedures such as plantarflexion osteotomy of the first metatarsal, interpositional arthroplasty and implant arthroplasty are designed to restore range of motion. The procedures that have the best outcome and long-term benefit in the treatment of hallux rigidus are those that limit pain, not those that are designed to improve joint range of motion.42-44
Gait studies have shown significant abnormalities in patients with hallux rigidus.45-47 However, one cannot conclude that the abnormal gait pattern is solely due to restricted range of motion of the first MPJ. When patients get relief of pain with surgical procedures for hallux rigidus, these same studies show gait patterns improve and almost return to normal. Interestingly, two studies showing such improvements after surgery for hallux rigidus occurred on patients undergoing arthrodesis of the first MPJ, which clearly eliminates motion rather than restoring motion.48-49 This has led some researchers to suggest that limiting pain, rather than restoring range of motion at the first MPJ, may be the more important goal when treating hallux rigidus.50
Concluding Treatment Recommendations
1. Research has implicated metatarsus primus elevatus and first ray hypermobility as causative factors for hallux rigidus, but recent research has called into question whether any such cause/effect relationship actually exists.18,20-22
2. Static measurements and range of motion of first ray position and laxity do not predict actual performance of this segment during dynamic gait.
3. Dynamic loading of soft tissue structures including the peroneus longus, the flexor hallucis longus and the plantar fascia are probably more important than static alignment of the first ray in the pathomechanics of hallux rigidus.
4. Surgeons should favor treatments that diminish pain around the first MPJ over those intending only to improve joint range of motion.
Dr. Richie is a Clinical Associate Professor at the Western University of Health Sciences. He is a Fellow and Past President of the American Academy of Podiatric Sports Medicine. Dr. Richie is a Fellow of the American College of Foot and Ankle Surgeons. He is in private practice in Seal Beach, Calif. Dr. Richie writes a monthly blog for Podiatry Today. One can access his blog at www.podiatrytoday.com/blogs/301 .
References
- Cotterill J. Stiffness of the great toe in adolescents. Br Med J. 1887; 1(1378):1158.
- Bingold A, Collins D. Hallux rigidus. J Bone Joint Surg. 1950; 32-B(2):214 – 222.
- Laird PO. Functional hallux limitus. Illinois Podiatr. 1972; 9(1):4.
- Camasta C. Hallux limitus and rigidus. Clinical examination, radiographic findings, and natural history. Clin Podiatr Med Surg. 1996; 13(3):423–448.
- Nilsonne H. Hallux rigidus and its treatment. Acta Orthop Scand. 1930; 1:295–303.
- Roukis TS, Jacobs PM, Dawson DM, et al. A prospective comparison of clinical, radiographic and intraoperative features of hallux rigidus. J Foot Ankle Surg. 2002; 41(2):76-95.
- Schweitzer M, Maheshwari S, Shabshin N. Hallux valgus and hallux rigidus: MRI findings. Clin Imag. 1999; 23(6):397–402.
- Beeson P, Phillips C, Corr S, et al. Classification systems for hallux rigidus: A review of the literature. Foot Ankle Int. 2008; 29(4):407-14.
- Nawoczenski DA, Baumhauer JF, Umberger BR. Relationship between clinical measurements and motion of the first metatarsophangeal joint during gait. J Bone Joint Surg. 1999; 81(3):370-6.
- Regnauld B. Disorders of the great toe. In Elson R (ed.) The Foot: Pathology, Aetiology, Seminology, Clinical Investigation And Treatment. Springer-Verlag, New York, 1986, pp. 269–281, 344–349.
- Hattrup SJ, Johnson KA. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop. 1988; 226:182–191.
- Morton D. Hypermobility of the first metatarsal bone: the interlinking factor between metatarsalgia and longitudinal arch strains. J Bone Joint Surg. 1928; 10:187–196.
- Jack EA. The aetiology of hallux rigidus. Br J Surg. 1940; 27(107):492- 497.
- Roukis TS, Scherer PR, Anderson CF. Position of the first ray and motion of the first metatarsophalangeal joint. J Am Podiatr Med Assoc. 1996; 86(11):538-46.
- Lambrinudi C. Metatarsus primus elevatus. Proc R Soc Med. 1938; 31(11):1273.
- Bonney G, Macnab T. Hallux valgus and hallux rigidus: a critical survey of operative results. J Bone Joint Surg Br. 1952; 34(3):366-385.
- Bouaicha S, Ehrmann C, Moor BK, et al. Radiographic analysis of metatarsus privus elevatus and hallux rigidus. Foot Ankle Int. 2010; 31(9):807-14.
- Horton GA, Park YW, Myerson MS. Role of metatarsus primus elevatus in the pathogenesis of hallux rigidus. Foot Ankle Int. 1999; 20(12):777–780.
- Bryant A, Tinley P, Singer K. A comparison of radiographic measurements in normal, hallux valgus and hallux limitus feet. J Foot Ankle Surg. 2000; 39(1):39–43.
- Meyer JO, Nishon LR, Weiss L, Docks G. Metatarsus primus elevatus and the etiology of hallux rigidus. J Foot Surg. 1987; 26(3):237-241.
- Roukis TS. Metatarsus primus elevatus in hallux rigidus: fact or fiction? J Am Podiatr Med Assoc. 2005; 95(3):221-8.
- Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003; 24(10):731-743.
- Coughlin JJ, Jones CP. Hallux valgus and first ray mobility. A prospective study. J Bone Joint Surg. 2007; 89-A(9):1887-98.
- Kurtz D, Harrill J, Kaczander B, Solomon M. The Valenti procedure for hallux limitus: a long-term follow-up and analysis. J Foot Ankle Surg. 1999; 38(2):123–130.
- Gould N. Hallux rigidus: cheilectomy or implant? Foot Ankle. 1981; 1(6):315–320.
- McMaster MJ. The pathogenesis of hallux rigidus. J Bone Joint Surg Br. 60(1):82–87.
- Baravarian B, Briskin GB, Burns P. Lapidus bunionectomy: arthrodesis of the first metatarsocunieform joint. Clin Podiatr Med Surg. 21(1):97–111, vi.
- Greisberg J, Sperber L, Prince D. First ray mobility is increased in patients with metatarsalgia. Foot Ankle Int. 2010; 31(11):954–8.
- Root ML, Orien WP, Weed JH. Normal and Abnormal Function of the Foot. Clinical Biomechanics Corp, Los Angeles, 1977.
- Glasoe WM, Yack HJ, Saltzman CL. Measuring first ray mobility with a new device. Arch Phys Med Rehabil. 1999; 80(1):122–124.
- Klaue K, Hansen ST, Masquelet AC. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 1994; 15(1):9–13.
- Glasoe W, Allen M, Saltzman C, Ludewig P, Sublett S. Comparison of two methods used to assess first-ray mobility. Foot Ankle Int. 2002; 23(3):248–252.
- Kirane YM, Michelson JD, Sharkey NA. Contribution of the flexor hallucis longus to loading of the first metatarsal and first metatarsophalangeal joint. Foot Ankle Int. 2008; 29(4):367–77.
- Phillips RD, Law EA, Ward ED. Functional motion of the medial column joints of the foot during propulsion. J Am Podiatr Med Assoc. 1996; 86(10):474–486.
- Harton FM, Weiskopf SA, Goecker RM. Sectioning the plantar fascia. Effect on first metatarsophalangeal joint motion. J Am Podiatr Med Assoc. 2002;92(10):532-6.
- Allen MK, Cuddeford TJ, Glasoe WM, et al. Relationship between static mobility of the first ray and first ray, midfoot and hindfoot motion during gait. Foot Ankle Int. 2004; 25(6):391-6.
- Johnson CH, Christensen JC. Biomechanics of the first ray. Part 1: The effects of peroneus longus function: a three- dimensional kinematic study on a cadaver model. J Foot Ankle Surg. 1999; 38(3):313–321.
- Hicks JH. The mechanics of the foot. II: The plantar aponeurosis and the arch. J Anat. 1954; 88(1):25–30.
- Malerba F, Milani R, Sartorelli E, Haddo O. Distal oblique first metatarsal osteotomy in grade 3 hallux rigidus: a long-term followup. Foot Ankle Int. 2008; 29(7):677–682.
- Ronconi P, Monachino P, Baleanu PM, Favilli G. Distal oblique osteotomy of the first metatarsal for the correction of hallux limitus and rigidus deformity. J Foot Ankle Surg. 2000; 39(3):154–160.
- Derner R, Goss K, Postowski HN, Parsley N. A plantar-flexor- shortening osteotomy for hallux rigidus: a retrospective analysis. J Foot Ankle Surg. 2005; 44(5):377–389.
- Yee G, Lau J. Current concepts review: hallux rigidus. Foot Ankle Int. 2008; 29(6):637-646.
- Brewster M. Does total joint replacement or arthrodesis of the first metatarsophalangeal joint yield better functional results? A systematic review of the literature. J Foot Ankle Surg. 2010; 49(6):546-52.
- McNeil DS, Baumhauer JF, Glazebrook. Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int. 2013; 34(1):15-32.
- VanGheluwe B, Dananberg HJ, Hagman F, Vanstaen K. Effects of hallux limitus on plantar foot pressure and kinematics during walking. J Am Podiatr Med Assoc. 2006; 96(5):428–436.
- Mulier T, Steenwerckx A, Thienpont E, et al. Results after cheilectomy in athletes with hallux rigidus. Foot Ankle. 1999; 20(4):232–237.
- Nawoczenski DA. Nonoperative and operative intervention for hallux rigidus. J Orthop Sports Phys Ther. 1999; 29(12):727–735.
- Brodsky JW, Baum BS, Pollo FE, Mehta H. Prospective gait analysis in patients with first metatarophalangeal joint arthrodesis for hallux rigidus. Foot Ankle Int. 2007; 28(2):162–165.
- DeFrino PF, Brodsky JW, Pollo FE, Crenshaw SJ, Beischer AD, et al. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int. 2002; 23(6):496-502.
- Maher AJ, Metcalfe SA. First MTP joint arthrodesis for the treatment of hallux rigidus: Results of 29 consecutive cases using the foot health status questionnaire validated measurement tool. Foot. 2008; 18(3):123-130.











