Postoperative Complications Following Reduction Mammaplasty in Relation to Patient Body Mass Index
© 2024 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Reduction mammaplasty is a common procedure that is performed for both aesthetic reasons and quality-of-life improvement. It is performed largely to help the patient achieve a proportionate breast size for their individual body type, with the goal of restoring anatomical proportionality and psychological wellness while reducing chronic neck, back, and shoulder pain. The common risks of breast reduction include bleeding, scarring, infection, poor wound healing, fat necrosis, nipple necrosis, and/or seroma. This study is designed to show that patients with a body mass index (BMI) of >30.0 kg/m2 are at higher risks for all complications.
Methods. This retrospective study analyzed medical records of 236 patients who underwent breast reduction mammaplasty from January 2015 to February 2022 by a single surgeon at a single institution. Patients were divided into 2 groups based on their BMI: the non-obese group with a BMI ≤29.9 kg/m2 and the obese group with a BMI ≥30.0 kg/m2 and above. This study compares postsurgical outcomes and complications in relation to patient BMI.
Results. Of 236 total patients, 104 (44%) had complications specified by predetermined criteria. Of those 104 patients with complications, 94 (90.38%) had a BMI ≥30.0 kg/m2. Predetermined complications were as follows: 24 patients (23.08%) experienced wound dehiscence, 23 of whom had a BMI ≥30.0 kg/m2; 9 patients (8.65%) experienced hematomas, all of whom had a BMI ≥30.0 kg/m2; 37 patients (35.58%) were found to have superficial wounds, 32 of whom had a BMI ≥30.0 kg/m2; 39 (37.5%) were found to have a seroma, 35 of whom patients were found to have a BMI ≥30.0 kg/m2; 25 patients (24.04%) experienced fat necrosis, 24 of whom had a BMI ≥30.0 kg/m2; 3 patients (2.88%) experienced nipple necrosis, all of whom had a BMI ≥30.0 kg/m2; 20 patients (19.23%) experienced infection, 19 of whom had a BMI ≥30.0 kg/m2.
Conclusions. On the basis of data gathered and the statistics performed, patients with a BMI ≥30.0 kg/m2 were 4.86 times more likely to have postsurgical complications than those with a BMI <30.0 kg/m2.
Introduction
The reduction mammaplasty procedure was first recorded and performed in the early 1900s by surgeons who were concerned mostly with size reduction versus aesthetics.1 Today, a reduction mammaplasty procedure is performed not only with the goal of reducing such common complaints as back pain, neck pain, uncomfortable and expensive bras, and inframammary fungal infections but also achieving proportionate breast size and repositioning the nipple on the breast to give an aesthetic appearance once healed. According to the American Society of Plastic Surgeons, reduction mammaplasty was performed 33,574 times in 2020 for cosmetic reasons alone, and 63,746 times for reconstructive patients. The psychosocial factors of a patient who seeks a reduction mammaplasty include back and/or shoulder pain, skin irritation and/or infections, feeling uncomfortable with their bodies, insecurities about uneven breast sizes, and the inability to exercise and find properly fitting clothing. The goal of this study was to determine if there was a relationship between obesity and negative postoperative outcomes for a common elective procedure, such as reduction mammaplasty.2 Higher body mass index (BMI) has already been linked to higher chances of postoperative wound infection, longer operative times, and poorer outcomes compared with patients who have a normal BMI.3 Obesity in general is a risk factor for perioperative morbidity, and morbid obesity is a known risk factor to raise mortality.4
Methods and Materials
This study consisted of a retrospective chart review of patients who underwent a reduction mammaplasty procedure from January 2015 to February 2022. All procedures were performed by J.S. at a rural hospital in southern Ohio. A total of 236 patients and 464 breasts were studied. Of the 464 breasts undergoing reduction mammaplasty, 234 procedures were performed on the right breast and 230 performed on the left breast. Patients were chosen based on the criteria that they were patients of J.S. and underwent a reduction mammaplasty procedure performed by J.S. Patient information that was reviewed and recorded was BMI, age, and any associated chronic health problems or behaviors, such as diabetes, hypothyroidism, smoking, and any other known conditions that would contribute to poor wound healing. In addition to this information, any postoperative complications were also recorded. Complications that were studied included: superficial or deep surgical site infection, wound dehiscence, seroma, hematoma, hypertrophic scarring, superficial wounds, and areola/nipple necrosis.
Patients were stratified by demographic data, and postsurgical complication rates were analyzed. All patients who met the specified criteria were split into 2 groups based on their BMI: non-obese with a BMI ≤29.9 kg/m2 or obese with a BMI ≥30.0 kg/m2. There were no excluding criteria. All patients with a BMI ≤29.9 kg/m2 were placed into group A and all patients with a BMI ≥30.0 kg/m2 were placed into group B. From there, each group was analyzed separately and categorized according to those who had complications and those who did not. Those with complications were grouped by specific type of postoperative complication.
Patients in each postoperative complication category were then assessed for chronic health problems or negative health behaviors that promoted poor wound healing, such as current or former smoking, hypertension, and diabetes. Infection was defined as symptomatic superficial or deep infection that required extra postoperative care, such as topical antibiotic with dressing changes or oral antibiotic treatments. Seroma and hematoma were defined as a symptomatic collection of fluid that was required to be drained based on patient comfort and surgeon discretion. Superficial wounds were defined as dehiscence requiring topical antibiotic ointment. Wound dehiscence was defined as partial or total separation of once-approximated wound edges.5 Areola necrosis was defined as total or partial loss of once-viable areolar tissue. Superficial or deep surgical site infection was defined as those infections occurring within 30 days of the surgery and affecting either the incision or deep tissue of the procedure site.6
Statistical analysis of demographic data versus postsurgical outcomes was performed using SigmaPlot v15 software (Grafiti LLC). The mean, standard deviation, and P value of each individual group and subset thereof were calculated and compared. An α = .05 was used to determine statistical significance. Data were reported as a percentage for both groups A and B (>30 kg/m2 or <29.9 kg/m2, respectively). Due to the nature of the data being reported in a categorical variable, an odds ratio was used to compare each group and compute the significance. A P value of .05 or less and a population size of at least 194 patients were used to calculate a statistically significant outcome.
Results
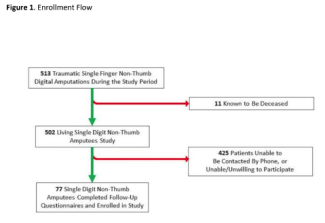
A total of 236 patients were studied using a retrospective chart review. These patients underwent the same reduction mammaplasty procedure for a total of 464 breasts. Each patient underwent a reduction mammaplasty with a wise pattern and superior medial pedicle; mean pedicle length was 10 cm and never measured more than 20 cm. The breasts were closed with 3-0 Vicryl nonabsorbable suture (Ethicon Inc) in the deep dermal layer and 4-0 antibacterial spiral Monocryl monofilament (Ethicon Inc) around the nipple/areola complex and vertical limb, covered with Prineo glue tape (Ethicon Inc) and wrapped in an elastic bandage. No drains were used, and compression was applied for 6 weeks postoperatively. Of note, this surgeon required patients to be nonsmokers or test negative for nicotine before surgery if they admitted to smoking or vaping. The patients experiencing complications totaled 104 (44%) of the 236 patients. The complication types are displayed in Figure 1.

Figure 1. Total complications of patients undergoing reduction mammaplasty.
These 104 patients had a total of 157 complications as specified by predetermined criteria. Of those 104 patients, 94 (90.28%) had a BMI ≥30.0 kg/m2. The complications were broken down further into the 5 classes of BMI values, as shown in Table 1.

The amount of tissue removed per breast was also calculated in grams according to each patient’s individual body surface area. The average amount of tissue removed from patients in each BMI range is displayed in Table 2.

Wound dehiscence was defined as a partial or total separation of previously approximated wound edges. Of 104 patients with complications, 24 (23.08%) experienced wound dehiscence, 23 of whom had a BMI ≥30 kg/m2. Hematoma was defined as a symptomatic collection of blood that was drained based on surgeon discretion; 9 patients (8.65%) of 104 with complications were found to have hematomas, and all 9 had a BMI ≥30 kg/m2. Superficial wounds, defined as an area requiring topical antibiotic ointment, were reported in 37 patients (35.58%); of those, 32 had a BMI ≥30 kg/m2. Seroma was previously defined as a symptomatic collection of fluid that occurred where breast tissue was excised and was drained by aspiration based on surgeon discretion. A total of 39 patients (37.5%) of the 104 with complications were found to have a seroma, 35 of whom had a BMI ≥30 kg/m2. Fat necrosis was defined as a hard lump felt underneath the skin that was believed to be caused by decreased blood supply to the fat during the reduction mammaplasty procedure. Of the 104 patients with complications, 25 (24.04%) experienced fat necrosis and nearly all of these (n = 24) had a BMI ≥30 kg/m2. Nipple necrosis, defined as partial or total loss of previously viable areolar tissue, affected 3 (2.88%) of 104 patients, and all 3 of these patients had a BMI ≥30 kg/m2 or greater. Infection was defined as a symptomatic invasion of bacteria, either superficially or deep, that was treated by surgeon discretion. A total of 20 patients (19.23%) were found to have had either a superficial or deep infection of surgical incisions, 19 of whom had a BMI ≥30 kg/m2.
All data listed included likelihoods of complications with associated confidence intervals (CI) with any interval going through or including the value 1 not statistically significant.
Figure 2 demonstrates the likelihood of each complication and the associated CI.

Figure 2. Complication likelihoods and associated CIs. CI, confidence interval.
Based on patient data gathered and the number of complications, a simple odds ratio with a 95% CI showed that patients with a BMI ≥30 kg/m2 were 4.86 times more likely to have complications than those patients whose BMI was <30 kg/m2. Patients with a BMI ≥30 kg/m2 were 7.86 times more likely to experience wound dehiscence, 6.11 times more likely to experience hematomas, 2.15 times more likely to experience superficial wounds, 3.06 times more likely to experience seromas, 8.25 times more likely to experience fat necrosis, 2.18 times more likely to experience nipple necrosis, and 6.33 times more likely to experience infection.
During the calculations of odds ratios for hematomas and seromas, the Haldane-Anscombe correction was applied with a value of 0.5 to the 2 × 2 contingency table to correct for the value of infinity due to no patients with a BMI <30 kg/m2 experiencing these complications throughout the study period. Of all the complications analyzed, the increased incidence of wound dehiscence, seroma, and fat necrosis in obese patients was found to be statistically significant based on the corresponding CI. Overall, the patients with a BMI ≥30 kg/m2 were more likely to experienced complications (P < .0001).
Discussion
Breast mammaplasty is a common surgical procedure that is used to modify the size, shape, and contour of the breasts. While there have been advances in surgical techniques, complications still arise. Risks of these complications can be higher secondary to patient characteristics as described in this study. Using a retrospective method, we analyzed data that identified the most common postoperative complications of breast mammaplasty associated with a BMI of ≥30 kg/m2. By knowing the most common complications, health care professionals can develop effective strategies to minimize the risk of complications in this patient population. Through the results of this study and the patients enlisted, we found that patients having a BMI ≥30 kg/m2 were at a higher risk for such complications as wound dehiscence, fat necrosis, hematomas, and poor wound healing. The specific complications addressed in this study can lead to additional surgeries, prolonged recovery times, and increased health care costs. Therefore, it is essential to consider a patient’s BMI before performing breast mammaplasty and to educate patients about the potential risks associated with this procedure. Because of the outcomes of this study, J.S. has now implemented a policy requiring patients have a BMI of <40 kg/m2 to be a candidate for reduction mammaplasty in her practice.
Limitations
Certain limitations within the study exist. First, all results may not be generalizable due to all patients undergoing surgery in a single hospital within a rural area, which limits comparisons to patients in a more urban population setting. More studies with different patient populations would be needed to generalize these findings to a broader population of patients. Furthermore, this study cannot account for the difference in surgical techniques as every surgery was done by a single surgeon at a single institution.
In addition, patients were classified according to age. A review of the data showed that 4 of the 9 hematomas were in patients older than 50 years of age. Although hematoma could be associated with menopause, this paper was focused on the correlation of BMI and complications.
Lastly, patients within this rural area could have had limited access to in-depth postsurgical care following reduction mammaplasty, which may have affected the complication rates seen within the study.
Conclusions
Based on the collected data, obesity is a risk factor for increased common postoperative complications after reduction mammaplasty. As these complications are a risk to all patients undergoing a reduction mammaplasty procedure, obesity should not be a complete contraindication for reduction mammaplasty but should warrant honest and open communication with patients whose BMI is ≥30 kg/m2 regarding their increased risk.
Acknowledgments
Authors: Jessica Suber, MD1; Grace Berry, BS, OMS-IV2; Philip Janszen, BS, OMS-IV2; Rachel Haddad, DO1; Steven Janszen, BS, OMS-IV2
Affiliations: 1Southern Ohio Medical Center, Portsmouth, Ohio; 2 Ohio University Heritage College of Osteopathic Medicine, Athens, Ohio
Correspondence: Jessica Suber, MD; jessicasuber@gmail.com
Ethics: Institutional review board approval was obtained for this study (IRB number 00002622, FWA00002833).
Disclosures: The authors disclose no relevant conflict of interest or financial disclosures for this study.
References
1. Purohit S. Reduction mammoplasty. Indian J Plast Surg. 2008 Oct;41(Suppl):S64-79.
2. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016 Dec 9;11(12):e0167746. doi:10.1371/journal.pone.0167746
3. Al-Mulhim AS, Al-Hussaini HA, Al-Jalal BA, Al-Moagal RO, Al-Najjar SA. Obesity disease and surgery. Int J Chronic Dis. 2014;2014:652341. doi:10.1155/2014/652341
4. Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg. 2007;31(3):556–560. doi:10.1007/s00268-006-0305-0
5. Rosen RD, Manna B. Wound dehiscence. In: StatPearls. StatPearls Publishing; 2022. Accessed February 17, 2024. https://www.ncbi.nlm.nih.gov/books/NBK551712/
6. Owens CD, Stoessel K. Surgical site infections: epidemiology, microbiology and prevention. J Hosp Infect. 2008 Nov;70 Suppl 2:3-10. doi:10.1016/S0195-6701(08)60017-1
7. Banuelos J, Abu-Ghname A, Vyas K, et al. Should obesity be considered a contraindication for prepectoral breast reconstruction? Plast Reconstr Surg. 2020 Mar;145(3):619-627. doi:10.1097/PRS.0000000000006540
8. Borenstein A, Friedman O. Multilevel breast reduction: a retrospective study of 338 breast reduction surgeries. Plast Reconstr Surg Glob Open. 2019 Aug 30;7(8):e2427. doi:10.1097/GOX.0000000000002427
9. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women. Plast Reconstr Surg. 2019 Sep;144(3):572-581. doi:10.1097/PRS.0000000000005907
10. Ri M, Aikou S, Seto Y. Obesity as a surgical risk factor. Ann Gastroenterol Surg. 2017 Oct 28;2(1):13-21. doi:10.1002/ags3.12049
11. Myung Y, Heo CY. Relationship between obesity and surgical complications after reduction mammaplasty: A systematic literature review and meta-analysis. Aesthet Surg J. 2017;37(3):308-315. doi:10.1093/asj/sjw189