Osteocutaneous Fibular Flap for Reconstruction of Composite Metacarpal Defects Due to Gunshot Wounds
© 2023 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Gunshot wounds of the hand are challenging, as these injuries include bones, tendons neurovascular structures, and soft tissue. The osteocutaneous fibula flap has shown to be an excellent option for treating the composite defects, including bone and soft tissue. In this study, reconstructions of gunshot injuries of the metacarpal bones with a fibular flap are presented.
Methods. Six patients with gunshot injuries to the hand were treated with free fibula flap. All patients had composite defects reconstructed with osteocutaneous fibula flap. Because of the size mismatch between fibula and metacarpal bone, a longitudinally split fibula was used in 2 patients. In 1 patient, the flap was used in a double-barrel fashion to reconstruct 2 metacarpal bone losses. Tendon repairs were performed either primarily or with tendon graft. All patients received hand rehabilitation. Hand function of the patients was evaluated by grip and pinch strength tests and Jebsen hand function test.
Results. All flaps survived with no major postoperative complications. The mean follow-up period was 18 months. Web releasing and an arthrodesis procedure was performed in 1 patient, and tenolysis was performed in 2 others. All flaps adapted well to the recipient area. With respect to routine daily activities, overall hand function measured by grip and pinch strength tests and Jebsen hand function test was considered satisfactory in all patients.
Conclusions. The fibular flap is a good alternative for reconstruction of the injured hand with composite defects, including metacarpal bone and soft tissue. It can be used longitudinally or transversely. Osteotomies can be performed to obtain split fibular flap or double-barrel fibular flap according to the bone defect.
Introduction
A gunshot wound results from the absorption of kinetic energy imparted by a missile when it strikes and penetrates the tissue. The amount of energy transfer will depend on the velocity, size, shape, and construction of the missile and the characteristics of the penetrated tissues. High-density tissues, such as bone, will absorb more of the missile’s kinetic energy and will consequently suffer greater damage.1 Gunshot wounds of the hand pose a challenge to the reconstructive surgeon because these injuries include bones, tendons, neurovascular structures, and soft tissue. High-velocity gunshot injuries, including those involving metacarpal bones, almost always result in metacarpal defects with accompanying tendon and skin defects.1-4 Two major problems arise in these complex situations: first, an osseous defect with potentially colonized or infected avascular residual bone; second, a defect of surrounding soft-tissue envelope with contamination and insufficient blood supply.4 Staged soft tissue reconstruction with local, distant, or free tissue transfer followed by nonvascularized bone grafts produces unsatisfactory results because of the risk of infection and bone resorption.5 The transfer of vascularized composite osteocutaneous flap may be advantageous because of the flap’s ability to survive in a hypovascular, potentially infected environment. In addition, these flaps react to physiological and physical strains in a "normal” way.6
The free fibular osteocutaneous flap is the workhorse of the vascularized bone tissue reconstruction and has been used for composite defects of long bones and the mandible.7-10 It is a reliable flap and has minimal donor site morbidity.11,12 In the literature, only a handful of articles have been published about the use of fibular flap in metacarpal defects.13-18 In this article, we present our experience as well as the long-term functional outcomes of patients with metacarpal injuries due to gunshot wounds who underwent reconstruction using composite free osteocutaneous fibular flap.



Methods
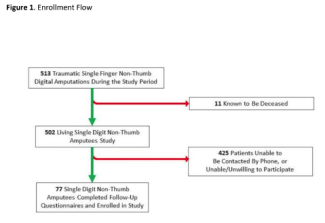
Six patients with gunshot injuries of the hand, resulting in composite metacarpal loss, were treated with free vascularized fibular flap. All patients were male with a mean age of 23 years. The patients underwent a careful clinical and radiologic evaluation, and all injuries were clarified before surgery. The deep and superficial palmar arc of the injured hand was assessed with Doppler ultrasound. The bony defects consisted of 1 metacarpal bone in 4 patients, 2 metacarpal bones in 1 patient, and 3 metacarpal bones in 1 patient. The patient who lost 2 metacarpal bones received a double-barrel osteocutaneous fibular flap. In 2 patients, the fibular bone segment was split longitudinally for size adjustment to the native metacarpal bones. In the last patient, the defect involved the second, third, and fourth metacarpal shafts, and the fibular flap was used transversely to reconstruct the bony defect (Figures 1, 2, and 3). Soft tissue defects were observed at the dorsum of the hand in 5 patients and at the thenar region in 1 patient. All patients had various degrees of extensor and/or flexor tendon injuries. The characteristics of the patients’ injuries are seen in Table 1.


Surgical Technique
The bony landmarks of the fibula were outlined, and Doppler ultrasound was used to locate the perforators to the skin paddle. The skin island was planned according to the soft tissue loss at the recipient site. The osteocutaneous fibula flap was harvested in the routine fashion as previously described.19
All patients were referred to our department from other hospitals after an initial intervention that included stabilization, initial debridement, and bone fracture stabilization with K wires or external fixators. Following admission to our department, additional debridement and definitive reconstruction were performed within 2 days. The fibular bone was osteotomized to replace the single or adjacent missing bone segments. During the treatment of the second and third patients, the fibular bone could hardly be inserted to the defects because of the size mismatch. Therefore, in the fourth and fifth patients, the fibular bone was split longitudinally to reduce the size, which enabled better adjustment to the defect (Figure 4). To split the fibula following the harvest of the flap, the fibular cortex (which does not carry the fibular pedicle or septocutaneous perforators) was excised via longitudinal osteotomy. By this way, we obtained a narrower fibular bone segment. The fibula segment was fixed to the bone remnants with K wires. The flexor tendons were repaired primarily. The extensor tendons were repaired either primarily or with tendon grafts. K wires were removed at 6 weeks postoperatively.

Rehabilitation
Rehabilitation consisted of early mobilization, range of motion exercises, and occupational therapy focusing on all digits and hand. After 3 weeks of therapy, the patients were given a home exercise program and instructed to follow up regularly with the plastic surgery and physical rehabilitation teams (Figure 5). Preoperative evaluation was not possible as all patients were in the acute period of the gunshot injury. The follow-up period of 6 patients ranged from 12 to 26 months with an average of 18 months.
Postoperative evaluation of the hand function was performed at 6 months following reconstruction. Only 3 patients accepted and gave consent to attend the evaluation tests. Grip strength and pinch strength were measured using a Jamar dynamometer and pinchmeter, respectively. Jebsen hand function test, one of the most frequently employed tests for determining hand function in daily activities,20-22 was also administered at this evaluation. The Jebsen test involves 7 assessments: (1) turning over cards; (2) picking up small objects and placing them in a can; (3) simulated eating; (4) stacking checkers; (5) moving large light cans; (6) moving heavy cans; and (7) writing; however, the writing portion of the Jebsen test was excluded from our assessment since writing ability strongly correlates with hand dominance.21 The time taken to complete each test item was recorded in seconds.
Results
All flaps survived with no major postoperative complications requiring surgical intervention. Venous congestion was observed in the skin islands of the second and third cases, which were treated by using medical leeches. We thought that size discrepancy might contribute to the venous congestion in the skin island by causing compression of the perforators. Therefore, in the following 2 patients (fourth and fifth cases), the fibular bone segment was split longitudinally for size match and better adjustment during inset of the flap (Table 1). We have not observed any vascular problems in patients with split fibular flap reconstruction. The mean follow-up period of the 6 patients was 18 months (range, 12-26 months). Clinical and radiological union was established in all cases after an average of 2 months. No delayed bone resorption or migration was observed.


Regarding the routine daily activities, overall hand function was considered satisfactory in all patients (Figure 6). All but 1 patient had an intact first ray, and these 5 patients had sufficient prehensile opposition. The patient with first ray reconstruction had mild opposition. The results of grip and pinch strength and Jebsen hand function tests are presented in Table 2. Both the grip and pinch strengths were close to normal values, showing the overall function and stabilization of the hand. Jebsen hand function test, a standardized and reliable tool for evaluating hand function, also showed near-normal results in our cases. These results indicate acceptable hand function, speed and accuracy of hand movements, and overall quality of life. No significant impairment was noted in the specific areas (subtests) of the Jebsen hand function test.
The remaining 3 patients who did not agree to undergo the functional evaluation, stated that they were happy with their overall hand function and were able to perform all their daily activities. Cosmetic results were acceptable, and no significant donor site morbidity was noted.
Discussion
Gunshot wounds of the hand almost always result with composite defects and present both functional and aesthetic reconstructive challenges. These wounds are frequently contaminated and are associated with impaired perfusion of bony and soft tissue structures. Moreover, gunshot wounds cause large composite bone and soft tissue defects, and they often require a free osteocutaneous flap to achieve satisfactory bone union.4,6 Various composite flaps, such as serratus anterior muscle-rib osteomyocutaneous flap, iliac osteocutaneous flap, osteocutaneous scapular flap, dorsalis pedis osteocutaneous flap, deep circumflex iliac artery flap, ulnar osteocutaneous flap, medial femoral condyle osteocutaneous flap, lateral arm flap, and radial forearm osteocutaneous free flap have been successfully used for reconstruction of the injured hand.14,19,23-25 However, all have limited use due to several disadvantages, such as donor site morbidity, soft tissue bulk, and an associated inability to perform osteotomies to the bone.4,13,14,24 The free fibula flap, on the other hand, has been the workhorse for reconstruction of large bone defects ever since it was first described by Hidalgo.7 Although commonly used in reconstruction for weight-bearing long bones and mandibular and midface reconstruction, it has not been used frequently for metacarpal reconstruction.13-16,19,22
The free fibula flap has distinct advantages in long bone reconstruction. The peroneal artery and vein run along the entire length of the fibula and permit its use as a flow-through flap for anticipated hand revascularization and segmental osteotomies.9,19,23,26 Multiple osteotomies can be performed safely, providing several struts for reconstruction of adjacent or alternating metacarpal defects. As seen in our third case, a double-barrel–shaped fibular flap enables reconstruction of more than 1 metacarpal bone.18
Another useful modification may involve placing the fibular bone in trapezoidal fashion with 2 osteotomies, as reported by Addosooki et al.17 Lee et al reported on 2 cases of composite metacarpal defects reconstructed with fibular flaps, although the authors questioned the reliability of septocutaneous perforators to the fibular flap.13 We, however, think the septocutaneous perforators are very reliable, especially if marked preoperatively and harvested from the lower half of the fibular segment. The presence of multiple septocutaneous perforators enable harvesting chimeric flaps and reconstruction of 2 separate soft tissue defect areas.27
Lin et al and Lee et al reported that the size of the fibular bone is comparable to that of the metacarpal bones.13,14 However, according to our experiences, the fibular bone is much thicker than the metacarpal bones, and it is hard to inset the fibular bone to the metacarpal gap, especially if the defect is at the third and fourth metacarpals. Shen et al also agreed that the fibular segment is still thicker than metacarpal bone and advocated using a split fibular segment.27 When the first, second, and fifth metacarpal bones are reconstructed, the size discrepancy would not cause a serious problem because these bones are either at the radial or the ulnar border of the hand. The size mismatch becomes more important for the third and fourth rays. Due to the rich periosteal blood supply of the free fibular flap, osteotomies can be performed to achieve a bone of desired shape without impairing its perfusion.15 In our series, we used a longitudinally split fibular flap and did not observe any impairment with the circulation of the flap. Consequently, especially for reconstruction of the third and fourth metacarpal bones, we recommend a longitudinal split of the fibula flap. However, special attention is needed to place the raw surface of the fibular bone away from the dorsum of the hand to prevent adhesions with the extensor mechanism.
Adequate bone stabilization is desired for bone healing during composite reconstructions. Although bone grafts covered with well-vascularized flaps seems to be an option, bone grafts may undergo resorption and cause infection.5 In the literature, immediate bone grafting is advocated for bone losses up to 2 cm.28,29 All our patients had bone defects longer than 2 cm in addition to contamination secondary to the gunshot wounds. Thus, we believe bone grafting is not a good option in such cases due to secondary resorption and infection. Alternatively, vascularized bone flaps offer transfer of viable osteocytes and osteoblasts that do not undergo resorption.30 Theoretically, compared with conventional corticocancellous bone grafting, this composite vascularized bone graft to metacarpal defects will have faster bone healing and less tissue adhesion.16
Reports in the literature describe the osteocutaneous radial forearm flap being used successfully for severe hand trauma.31 However, bone stock in a radial forearm flap is not comparable to that of a fibular flap as it provides more robust bone. Additionally, a radial forearm flap needs scarification of a major upper extremity artery and causes inacceptable donor site appearance. Plate and screws or K wire may be used for fixation of the bone. To protect periosteal blood supply, we used K wires and removed them 6 weeks after the operation. We observed adequate radiological bone healing at 3 months without any complication in all patients. Our experience with composite metacarpal reconstruction confirmed, once again, the consistency of the fibula osteoseptocutaneous free flap. In our series, all but 1 patient had intercalated defects, and their carpometacarpal and metacarpophalangeal joints were intact. We believe that intact joints contributed to the good functional outcome. When reconstruction includes the metacarpophalangeal joint or carpometacarpal joint, vascularized joint transfers and arthroplasties can be performed.32
Silicone implant arthroplasty is also a valid option for providing additional range of motion to the affected joints.33 However, our patients had all sustained gunshot wounds that became contaminated; thus, we chose not to perform silicone implant arthroplasty during the definitive reconstruction. During the follow-up period, all patients were satisfied with the function and did not want silicone implant arthroplasty.
Microsurgical free-tissue transfer has progressed from simply addressing wound coverage to offering a higher level of functioning and aesthetic restoration. Acute reconstruction of injured hands to the preinjury state is ideal for optimal functional and cosmetic results. In all our patients, the fibula free flap provided satisfactory aesthetic and functional results. The resulting grip and lateral pinch strength was comparable with normal.34 However, the literature recommends that when using power grip and lateral pinch strength measurements to evaluate the progress and outcome of a patient, the occupation and the preinjury strength of the patient must be taken into consideration, even when the uninjured hand is used for comparison.35 All our patients were active duty miliary personnel with very high preinjury physical capacity. Thus, we believe that this also has a positive impact on the final outcome.
Although grip and pinch strength are used frequently to evaluate hand strength for disability ratings and to assess responses to various forms of therapy, they tend to fluctuate significantly on a day-to-day basis, and a patient’s progress or the effectiveness of therapy may be misjudged.36 Therefore, other modes of assessment should always be considered.35 Thus, we decided to use another test, the Jebsen hand function test, with the aim of evaluating precision and velocity of the movements rather than the strength of the hand, which was already measured by grip and pinch strength test. This test is designed to assess impairments related to hand function, including fine motor skills and overall hand coordination, by evaluating such tasks as writing, picking up small objects, and manipulating cards. The test can help identify specific areas of impairment and provide a baseline for tracking progress over time.37,38 Sharma et al demonstrated that all components of the Jebsen test, except for the writing assessment, correlated with patients’ abilities to perform activities of daily living.21 For the patients in our study, the Jebsen hand function test revealed good hand function that was adequate for performing daily activities. Other hand function evaluations can also be performed, such as the Michigan Hand Outcomes Questionnaire.39. However, this questionnaire is lengthy, has limited scope, and, most importantly, has ceiling and floor effects; as a result, this tool may not be able to accurately assess individuals who have very severe or very mild hand or upper extremity impairments.40 Thus, we prefer the Jebsen hand function test for evaluating function after severe hand injuries, such as gunshot wounds.
The fibular flap offers greater versatility for manipulating 3-dimensional defects of the hand when compared with the other osteocutaneous flaps. Some of the major advantages of fibular flap are as follows: (1) the close relationship of the peroneal artery with the fibula allows different designs of osteotomy; (2) the excellent bone vascularity induces rapid bone graft union; and (3) it can be taken with muscle, such as the flexor hallucis longus, to allow functional muscle transfer.11,12,14,19 In our series, we did not need any functional muscle segment; however, bone reconstruction with a functional muscle transfer offers a unique advantage and must be kept in mind for selected cases.
Limitations
There are 2 main limitations of our study. First and foremost, the small number of patients limits the generalizability of our findings. Larger series would give more information about functional results of our technique. Second, we encountered difficulty in maintaining follow-up of the patients and performing the optimal functional evaluation method. Finally, the decision-making process in selection of the best flap alternative for a particular patient requires a high level of expertise. While the fibular flap may be a good option for high-velocity military grade injuries, other bone reconstructive alternatives with less donor site morbidity (ie, iliac crest or medial femoral condyle) might be sufficient. Besides these limitations, our series offers the fibular osteocutaneous flap as an important option for composite hand defects.
Conclusions
The fibular flap is a good alternative for reconstruction of the injured hand with composite defects, including those injuries involving metacarpal bone and soft tissue. The flap can be used longitudinally or transversely. Osteotomies can be performed to obtain a split fibular flap or double-barrel fibular flap according to the bone defect.
Acknowledgments
Affiliations: 1Indiana University, School of Medicine, Indianapolis, Indiana; 2Gulhane Military Medical Academy, Department of Plastic and Reconstructive Surgery, Ankara, Turkey; 3Wake Forest School of Medicine, Winston Salem, North Carolina; 4Gulhane Military Medical Academy, Department of Hand Surgery, Ankara, Turkey
Correspondence: Fatih Zor, MD; fzor@iu.edu
Disclosures: The authors disclose no financial or other conflicts of interest.
References
1. Dzepina I, Stanec Z, Skrbić S, et al. One-stage reconstruction of war wounds with free osteocutaneous flaps. Brit J Plast Surg. 1997;50(2):81-87. doi:10.1016/s0007-1226(97)91318-7
2. Gonzalez MH, McKay W, Hall RF. Low-velocity gunshot wounds of the metacarpal: treatment by early stable fixation and bone grafting. J Hand Surg. 1993;18(2):267-270. doi:10.1016/0363-5023(93)90359-B
3. Kömürcü M, Alemdaroğlu B, Kürklü M, Ozkan H, Basbozkurt M. Handgun injuries with metacarpal and proximal phalangeal fractures: early definitive treatment. Int Orthop. 2008;32(2):257-262. doi:10.1007/s00264-006-0312-7
4. Kremer T, Bickert B, Germann Gn, Heitmann C, Sauerbier M. Outcome assessment after reconstruction of complex defects of the forearm and hand with osteocutaneous free flaps. Plast Reconstr Surg. 2006;118(2):443-454. doi:10.1097/01.prs.0000227742.66799.74
5. Kiehn MW, Mitra A, Gutowski KA. Fracture management of civilian gunshot wounds to the hand. Plast Reconstr Surg. 2005;115(2):478-481. doi:10.1097/01.prs.0000149537.88804.17
6. Gerwin M, Weiland AJ. Vascularized bone grafts to the upper extremity. Hand Clinics. 1992;8(3):509-523.
7. Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989;84(1):71-79.
8. Lee KS, Chung HK, Kim KH. Vascularised osteocutaneous fibular transfer to the tibia. Int Orthop. 1991;15(3):199-203. doi: 10.1007/BF00192294
9. Yajima H, Tamai S, Ono H, Kizaki K, Yamauchi T. Free vascularized fibula grafts in surgery of the upper limb. J Reconstr Microsurg. 1999;15(07):515-521. doi:10.1055/s-2007-1000131
10. Noaman HH. Management of upper limb bone defects using free vascularized osteoseptocutaneous fibular bone graft. Ann Plast Surg. 2013;71(5):503-509. doi:10.1097/SAP.0b013e3182a1aff0
11. Jones NF, Monstrey S, Gambier BA. Reliability of the fibular osteocutaneous flap for mandibular reconstruction: anatomical and surgical confirmation. Plast Reconstr Surg. 1996;97(4):707-716. doi:10.1097/00006534-199604000-00003
12. Tang CL, Mahoney JL, McKee MD, et al. Donor site morbidity following vascularized fibular grafting. Microsurgery. 1998;18(6):383-386. doi:10.1097/00006534-199604000-00003
13. Lee H-B, Tark K-C, Kang S-Y, Kim S-W, Chung Y-K. Reconstruction of composite metacarpal defects using a fibula free flap. Plast Reconstr Surg. 2000;105(4):1448-1452. doi:10.1097/00006534-200004040-00029
14. Lin C-H, Wei F-C, Rodriguez ED, Lin Y-T, Chen C-T. Functional reconstruction of traumatic composite metacarpal defects with fibular osteoseptocutaneous free flap. Plast Reconstr Surg. 2005;116(2):605-612. doi:10.1097/01.prs.0000173554.46455.5a
15. Momeni A, Stark GB. The free fibular flap: a useful flap for reconstruction following composite hand injuries. J Hand Surg. 2006;31(3):304-305. doi:10.1016/j.jhsb.2006.02.003
16. Simsek T, Engin MS, Demir A, Tayfur V, Eroglu L. Reconstruction of hand injuries with multiple metacarpal defects using free fibular osteoseptocutaneous flap. Microsurgery. 2012;32(7):520-526. doi: 10.1002/micr.21977
17. Addosooki A, Said E, Kenawey M, Yousef MA. Reconstruction of complex hand defects using trapezoidal osteocutaneous free fibular flap. Microsurgery. 2020;40(3):306-314. doi:10.1002/micr.30520
18. Masaki F, Takehiro D, Ryuuichi M, Kumi M. Late reconstruction of two total metacarpal bone defects using lengthening devices and a double-barrel osteocutaneous free parascapular flap. Plast Reconstr Surg. 2000;106(1):102-106. doi:10.1097/00006534-200007000-00019
19. Wei F-C, Chen H-C, Chuang C-C, Noordhoff MS. Fibular osteoseptocutaneous flap: anatomic study and clinical application. Plast Reconstr Surg. 1986;78(2):191-199. doi:10.1097/00006534-198608000-00008
20. Jain A, Ball C, Freidin AJ, Nanchahal J. Effects of extensor synovectomy and excision of the distal ulna in rheumatoid arthritis on long-term function. J Hand Surg Am. 2010;35(9):1442-1448. doi:10.1016/j.jhsa.2010.04.034
21. Sharma S, Schumacher HR, McLellan AT. Evaluation of the Jebson hand function test for use in patients with rheumatoid arthritis. Arthritis Care Res. 1994;7(1):16-19. doi:10.1002/art.1790070
22. Rider B, Linden C. Comparison of standardized and non-standardized administration of the Jebsen hand function test. J Hand Therapy. 1988;1(3):121-123. doi:10.1016/S0894-1130(88)80036-X
23. Boyd JB, Rosen I, Rotstein L, et al. The iliac crest and the radial forearm flap in vascularized oromandibular reconstruction. Am J Surg. 1990;159(3):301-308. doi:10.1016/s0002-9610(05)81223-1
24. Hsu CC, Tseng J, Lin YT. Chimeric medial femoral condyle osteocutaneous flap for reconstruction of multiple metacarpal defects. J Hand Surg Am. 2018;43(8):781.e781-781.e789. doi:10.1016/j.jhsa.2018.03.025
25. Ulusal BG, Lin YT, Ulusal AE, Lin CH. Free lateral arm flap for 1-stage reconstruction of soft tissue and composite defects of the hand: a retrospective analysis of 118 cases. Ann Plast Surg. 2007;58(2):173-178. doi:10.1097/01.sap.0000232832.18894.2b
26. Lin C-H, Wei F-C, Chen H-C, Chuang DCC. Outcome comparison in traumatic lower-extremity reconstruction by using various composite vascularized bone transplantation. Plast Reconstr Surg. 1999;104(4):984-992. doi:10.1097/00006534-199909040-00013
27. Shen H, Shen XQ, Lv Y, Lu H, Xu JH, Wu SC. Three-dimensional virtual planning in precise chimeric fibula free flap for metacarpal defects: a case report. Medicine (Baltimore). 2017;96(31):e7364. doi:10.1097/MD.0000000000007364
28. Saint-Cyr M, Miranda D, Gonzalez R, Gupta A. Immediate corticocancellous bone autografting in segmental bone defects of the hand. J Hand Surg. 2006;31(2):168-177. doi:10.1016/j.jhsb.2004.10.020
29. Stahl S, Lerner A, Kaufman T. Immediate autografting of bone in open fractures with bone loss of the hand: a preliminary report. Scand J Plast Reconstr Surg Hand Surg. 1999;33(1):117-122. doi:10.1080/02844319950159721
30. Pederson WC, Person DW. Long bone reconstruction with vascularized bone grafts. Orthop Clin North Am. 2007;38(1):23-35. doi:10.1016/j.ocl.2006.10.006.
31. Yajima H, Kobata Y, Kawamura K, Shigematsu K, Kawate K, Tamai S. Radial forearm flaps for reconstruction in hand surgery. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):112-117. doi:10.1080/02844310310014847
32. Malizos KN, Dailiana ZH, Innocenti M, Mathoulin CL, Mattar R Jr, Sauerbier M. Vascularized bone grafts for upper limb reconstruction: defects at the distal radius, wrist, and hand. J Hand Surg Am. 2010;35(10):1710-1718. doi:10.1016/j.jhsa.2010.08.006
33. Jones NF, Dickinson BP, Hansen SL. Reconstruction of an entire metacarpal and metacarpophalangeal joint using a fibular osteocutaneous free flap and silicone arthroplasty. J Hand Surg Am. 2012;37(2):310-315. doi:10.1016/j.jhsa.2011.10.031
34. Anakwe RE, Huntley JS, McEachan JE. Grip strength and forearm circumference in a healthy population. J Hand Surg Eur Vol. 2007;32(2):203-209. doi:10.1016/J.JHSB.2006.11.003
35. Lau VW-S, Ip W-Y. Comparison of power grip and lateral pinch strengths between the dominant and non-dominant hands for normal Chinese male subjects of different occupational demand. Hong Kong Physiother J. 2006;24(1):16-22. doi:10.1016/s1013-7025(07)70004-0
36. Young VL, Pin P, Kraemer BA, Gould RB, Nemergut L, Pellowski M. Fluctuation in grip and pinch strength among normal subjects. J Hand Surg. 1989;14(1):125-129. doi:10.1016/0363-5023(89)90071-3
37. Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50(6):311-319.
38. Sığırtmaç İ C, Öksüz Ç. Investigation of reliability, validity, and cutoff value of the Jebsen-Taylor Hand Function Test. J Hand Ther. 2021;34(3):396-403. doi:10.1016/j.jht.2020.01.004
39. Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23(4):575-587. doi:10.1016/S0363-5023(98)80042-7
40. Kroon FPB, Boersma A, Boonen A, et al. Performance of the Michigan Hand Outcomes Questionnaire in hand osteoarthritis. Osteoarthritis Cartilage. 2018;26(12):1627-1635. doi:10.1016/j.joca.2018.07.018