Nitinol Compression Staple Versus Headless Compression Screw Fixation for Scaphoid Waist Fractures
© 2024 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. There are a variety of ways to surgically manage patients with scaphoid waist fractures. The purpose of this study is to compare the rate of union achieved with a nitinol compression staple versus that of a headless compression screw in the treatment of scaphoid waist fractures.
Methods. We performed a retrospective review of patients with middle-third scaphoid fractures treated surgically. Patients were stratified into 2 groups based on fixation device: a nitinol compression staple or headless compression screw (HCS). Primary outcome was radiographic union. Secondary outcomes included time from surgery to union, development of avascular necrosis (AVN), complication rate, and need for revision.
Results. Forty-one patients were included in the final analysis. The median follow-up time was 5.7 months. Twenty patients were treated with staples, 21 with HCS. Thirty-seven patients achieved union. All who failed to unite were treated with HCS. Eight patients had postoperative complications, including postoperative AVN, all of whom were in the HCS cohort. This treatment group had a higher rate of revision surgery as well. Staples required less time to achieve union and fewer weeks of immobilization. Postoperative scapholunate angles were similar between the groups.
Conclusions. Fixation of scaphoid waist fracture with nitinol compression staples is at least as likely to achieve union as fixation with HCS in patients without prior surgical intervention. This treatment also demonstrated equivalent or better secondary outcomes, including postoperative AVN, complication and revision rates, time to union, and weeks immobilized.
Introduction
Scaphoid fractures account for 60% of carpal fractures and 2.4% of wrist fractures. Between 66% and 82% occur in males with peak incidence occurring in the second and third decades of life.1,2 Nondisplaced fractures have a 5% to 10% incidence of nonunion and 55% chance of nonunion if they are displaced more than 1 mm.3,4 If untreated, persistent nonunion may lead to degenerative radiocarpal osteoarthritis with persistent pain and impaired functionality.5 Scaphoid nonunions are often treated with headless compression screws, achieving union in greater than 80% of cases.6,7 However, the use of headless compression screws may result in complications related to its application, such as penetration of the screw into the intra-articular space.8 There has been recent evidence, however, demonstrating similar rates of union and fewer complications with use of nitinol staples compared with headless compression screws in the treatment of scaphoid delayed union and nonunion.9-13 Both in independent and comparative head-to-head studies, nitinol alloy staples provided greater and more durable compression at physiologic temperatures than do other staple constructs or compression screws.14-20 By comparing these 2 treatment modalities, we hypothesize patients treated with nitinol compression staples will have a greater incidence of union and have fewer complications compared with those treated with headless compression screws.
Methods and Materials
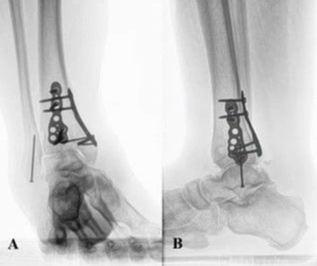
Following Institutional Review Board approval, all patients who underwent a repair of the scaphoid with open reduction and external fixation by 1 of 4 board-certified hand surgeons between 2010 and 2020 were identified by Current Procedural Terminology (CPT) codes 25440 and 25628. Subsequent chart review was performed to determine fracture location, union status, and surgical fixation technique. Patients who had surgical fixation of a scaphoid waist fracture with either a single nitinol compression staple via a volar approach (Figure 1) or a single headless compression screw were included (Figure 2). They were then stratified into 2 groups by fixation device that was based on surgeon preference. Patients with a staple were required to have undergone a volar approach as described by Congiusta et al.21 Exclusion criteria included prior intervention, pathologic fracture, less than 12 weeks follow-up, and less than 4 weeks between injury and surgery. Once identified, a full chart review was performed to collect data for statistical analysis.

Figure 1. Fixation with a single nitinol compression staple via a volar approach.

Figure 2. Fixation with a single headless compression screw.
Union, as determined radiographically in conjunction with snuffbox tenderness, was the primary outcome. If uncertainty persisted with regard to fracture healing following x-ray and physical exam, computed tomography scan was obtained at the discretion of the operating surgeon. Secondary outcomes included time to union, revision and complication rates, loss of alignment, postoperative avascular necrosis (AVN), postoperative resolution of preoperative AVN, weeks immobilized in nonremovable splint or cast, and postoperative scapholunate angle. AVN was diagnosed radiographically as sclerotic and bony changes consistent with avascular bone. Complications were defined as persistent nonunion, new or persistent AVN (AVN on presentation that does not resolve following surgical intervention) following surgical fixation, loss of alignment following fixation, infection, cellulitis, or hardware complications. Initial follow up was performed at 2 weeks and subsequently at monthly intervals; however, not all patients were strictly adherent to this schedule.
Categorical variables were compared using chi-squared or Fisher exact-tests where appropriate with Haldane-Anscombe22,23 adjustments of 0.5 applied to correct for incidences of 0. Continuous variables were analyzed using independent samples t tests for parametric data, whereas, in cases of nonparametric distributions, medians with associated interquartile ranges were reported and Mann-Whitney U tests were used for comparison. Statistical significance was set at P < .05. Analysis was conducted using SAS Enterprise Guide, Version 7.1 of the SAS System for Windows (SAS Institute).
Results
In total, 46 patients with scaphoid waist nonunion were identified. Of these, 5 (11%) were excluded due to insufficient follow-up. Thirty-four of the remaining 41 patients were male (83%). The median age was 22 years. Most injuries were right-sided (58%). The most frequent mechanism of injury was a fall, followed by motor vehicle collisions and motorcycle collisions. Characteristic data was not different between the 2 treatment groups. All patients presented with pain as their primary complaint, while nine (22%) also complained of decreased range of motion. Fifteen (37%) patients presented with proximal pole AVN. There was no difference in median follow-up time between the 2 groups (Table 1).

A total of 20 (49%) patients were treated with a single nitinol compression staple and 21 (51%) with a headless compression screw, which was similar to the sample sizes of other studies.9-11,13 Thirty-seven (90%) patients achieved union postoperatively. The 4 patients who failed to unite were treated with headless compression screws (19%). Median time to union was 2.7 months in those patients treated with a staple and 4.2 months in those treated with screws, a difference of 1.5 months. Patients treated with compression screws were at a greater risk for persistent or postoperative AVN, both of which were exclusive to this group. There were 8 complications, 4 persistent nonunion and 4 new or persistent AVN postoperatively, all occurring in the screw cohort, which was statistically significant. There was no loss of alignment, postoperative infection, cellulitis, or hardware complications in either group. Five patients required revision surgery, all of whom were in the group treated with screws (23%). This bordered statistical significance. On average, the staple group was immobilized in a cast or nonremovable splint for significantly fewer weeks compared with those treated with screws. The scapholunate angles of the 2 treatment groups were also assessed and were not significantly different. Outcome data is shown in Table 2.

Analysis of covariates showed no difference between the treatment groups with regard to age, time from injury to surgery, preoperative scapholunate angle, AVN on presentation, type of graft, and bone stimulator use. Further multivariate analysis showed no confounding effect of these variables on primary or secondary outcomes. Post-hoc bivariate analysis revealed that iliac crest graft, utilized in 10 patients in the overall cohort (24%) and 3 of those treated with headless compression screws (14%), was independently associated with persistent nonunion.
Discussion
This non-inferiority study demonstrates the comparable effectiveness of nitinol compression staples in the treatment of scaphoid waist fractures as compared with headless compression screws. Patients treated with a single nitinol compression staple from a volar approach were at least as likely as those treated with a single headless compression screw to achieve union. Secondary outcomes evidenced improvement with the use of a nitinol staple over a headless compression screw. Stapling resulted in fewer revisions, complications, and new or persistent AVN. These patients also achieved union faster and were immobilized for fewer weeks than those with headless compression screw fixation. Our study further supports union rates found in the literature for both fixation methods, albeit with a slightly higher rate than what has been thus far reported with compression staples,9-13,24-36 which is likely attributable to our use of the nitinol alloy staple as well as variations in fracture location, surgical technique, and bone grafting, while demonstrating a similar time to union9,12,13,28,36 and complication rate.37-41 While numerous studies have found success treating acute, delayed, and nonunion scaphoid waist fractures with compression staples,9-13,24-27 this technique remains underutilized.
Limitations
There are multiple limitations to this study. Although initial follow up was performed at 2 weeks with subsequent follow-up being scheduled at 1-month intervals at least until union was achieved, patients were not universally adherent to this schedule, which may affect the time at which union was identified. Further research is necessary to evaluate outcomes over a longer follow-up period as a median follow-up of 5.6 months is relatively short. However, it should be noted that those patients who did not achieve union following surgical intervention had a median follow up of 15.7 months with a range of 7.5 to 27.2 months. Additionally, functional data such as grip strength; range of motion; disabilities of the arm, shoulder, and hand (DASH) scores; and time to return to work were not universally collected. Analysis of these factors could provide essential insight into the clinical relevance of this head-to-head fixation comparison, and prospective investigation to evaluate these functional outcomes is a necessary next step in the assessment of these 2 techniques. Furthermore, a comparison of surgical time would be clinically relevant; however, this has not yet been established in the case of nitinol compression staples.
Conclusions
In the experience of the authors, treatment of scaphoid waist fractures with a nitinol compression staple versus a headless compression screw require similar amounts of time; however, they have found staple fixation to be the overall more efficient technique and may prevent graft extrusion owing to a buttressing effect of the staple. Staple fixation also offers technical advantages in that the scaphotrapezial joint is avoided (retrograde screw fixation) as is the proximal cartilage (anterograde screw fixation), and impingement of the distal radius is avoided utilizing techniques similar to those employed in other scaphoid plating and is described more thoroughly in Congiusta et al.21 With a mind to cost-conscious care, neither device provides benefit over the other as the price of the constructs are similar.
Acknowledgments
Authors: Adam M. Kurland, BA1; Dominick V. Congiusta, MD, MPH1; Ashley Ignatiuk, MD2; Abram E. Kirschenbaum, MD1; Michael M. Vosbikian, MD1; Irfan H. Ahmed, MD1
Affiliations: 1Department of Orthopaedic Surgery, Rutgers New Jersey Medical School, Newark, New Jersey; 2Department of Surgery, Plastic & Reconstructive Surgery Division, Rutgers New Jersey Medical School, Newark, New Jersey
Correspondence: Dominick V. Congiusta, MPH; dvc33@njms.rutgers.edu
Ethics: IRB study ID: Pro20170000549, "Orthopaedic Hand Surgery Outcomes and Complications: Retrospective Review."
Disclosures: The authors disclose no potential conflicts of interest in the information and production of this manuscript.
References
1. Van Tassel DC, Owens BD, Wolf JM. Incidence estimates and demographics of scaphoid fracture in the U.S. population. J Hand Surg Am. 2010;35(8):1242-1245. doi:10.1016/j.jhsa.2010.05.017
2. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999;33(4):423-426. doi:10.1080/02844319950159145
3. Osterman AL, Mikulics M. Scaphoid nonunion. Hand Clin. 1988;4(3):437-455.
4. Szabo RM, Manske D. Displaced fractures of the scaphoid. Clin Orthop Relat Res. 1988;230:30-38.
5. Lindström G, Nyström A. Natural history of scaphoid non-union, with special reference to "asymptomatic" cases. J Hand Surg Br. 1992;17(6):697-700. doi:10.1016/0266-7681(92)90204-f
6. Merrell GA, Wolfe SW, Slade JF 3rd. Treatment of scaphoid nonunions: quantitative meta-analysis of the literature. J Hand Surg Am. 2002;27(4):685-691. doi:10.1053/jhsu.2002.34372
7. Munk B, Larsen CF. Bone grafting the scaphoid nonunion: A systematic review of 147 publications including 5 246 cases of scaphoid nonunion. Acta orthopaedica Scandinavica. 2004;75(5):618-629. doi:10.1080/00016470410001529
8. Bushnell BD, McWilliams AD, Messer TM. Complications in dorsal percutaneous cannulated screw fixation of nondisplaced scaphoid waist fractures. J Hand Surg Am. 2007;32(6):827-833. doi:10.1016/j.jhsa.2007.04.003
9. Antti-Poika I, Korkala O, Bakalim G. Treatment of delayed union and non-union of the carpal scaphoid with a compression staple and cancellous bone grafting—new method and preliminary results. Ann Chir Gynaecol. 1987;76:266-268.
10. Carpentier E, Sartorius C, Roth H. Scaphoid nonunion: treatment by open reduction, bone graft, and staple fixation. J Hand Surg Am. 1995;20:235-240.
11. Dunn J, Kusnezov N, Fares A, et al. The scaphoid staple: a systematic review. Hand (N Y). 2017;12:236-241.
12. Korkala OL, Antti-Poika IU. Late treatment of scaphoid fractures by bone grafting and compression staple osteosynthesis. J Hand Surg Am. 1989;14:491-495.
13. Korkala OL, Kuokkanen HO, Eerola MS. Compression-staple fixation for fractures, non-unions, and delayed unions of the carpal scaphoid. J Bone Joint Surg Am. 1992;74:423-426.
14. Pelton, AR, DiCello, J, Miyazaki S. Optimization of processing and properties of medical grade mitinol wire. Min Invas Ther Allied Technol. 2000;9(1):107-118.
15. Chang TJ, Overley BD., An In Vitro Comparative Study of Screw and Nitinol Staple Compression: A Model Showing Active ‘Dynamic’ Compression. Presented at the American College of Foot & Ankle Surgeons 65th Annual Scientific Conference, Orlando, Florida, March 2007.
16. Farr D, Karim A, Lutz M, Calder J. A biomechanical comparison of shape memory compression staples and mechanical compression staples: compression or distraction?. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):212-217. doi:10.1007/s00167-009-0887-9
17. Shibuya N, Manning SN, Meszaros A, Budny AM, Malay DS, Yu GV. A compression force comparison study among three staple fixation systems. J Foot Ankle Surg. 2007;46(1):7-15. doi:10.1053/j.jfas.2006.09.008
18. McKnight RR, Lee SK, Gaston RG. Biomechanical properties of nitinol staples: effects of troughing, effective leg length, and 2-staple constructs. J Hand Surg Am. 2018; S0363-5023:31905-31906.
19. Hoon QJ, Pelletier MH, Christou C, Johnson KA, Walsh WR. Biomechanical evaluation of shape-memory alloy staples for internal fixation – an in vitro study. J Exp Orthop. 2016;3(1):19. doi:10.1186/s40634-016-0055-3
20. Hart A, Harvey EJ, Rabiei R, Barthelat F, Martineau PA. Fixation strength of four headless compression screws. Med Eng Phys. 2016;38(10):1037-1043. doi:10.1016/j.medengphy.2016.06.025
21. Congiusta DV, Basyuk Y, Vosbikian MM, Ahmed IH, Kirschenbaum A. The use of nitinol compression staple fixation and bone graft for scaphoid waist fractures and nonunion: a surgical technique. Tech Hand Up Extrem Surg. 2020;25(1):35-40. doi:10.1097/BTH.0000000000000303
22. Haldane, JBS. The mean and variance of the moments of chi-squared when used as a test of homogeneity, when expectations are small. Biometrika. 1940;29:133-134.
23. Anscombe, FJ. On estimating binomial response relations. Biometrika, 1956;43:461-464.
24. Zhou PY, Jiang LQ, Xia DM, Wu JH, Ye Y, Xu SG. Nickel-titanium arched shape-memory alloy connector combined with bone grafting in the treatment of scaphoid nonunion. Eur J Med Res. 2019;24(1):27. doi:10.1186/s40001-019-0380-y
25. Winkel R, Schlageter M. Formgedächtnisklammer aus NITINOL ("memory staple") zur Osteosynthese des Skaphoids [NITINOL shape memory staple for osteosynthesis of the scaphoid]. Oper Orthop Traumatol. 2009;21(4-5):361-372. doi:10.1007/s00064-009-1910-5
26. Song M, He X, Li C, Xu Y. [Nitinol memory alloy two foot fixator with autologous cancellous bone grafting for old scaphoid fracture and nonunion]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(6):676-682. doi:10.7507/1002-1892.201910078
27. Rocchi L, Merendi G, Cazzato G, et al. Scaphoid waist fractures fixation with staple. Retrospective study of a not widespread procedure. Injury. 2020;51:S2-S8. doi:10.1016/j.injury.2019.12.020
28. Hegazy G, Seddik M, Abd-Elghany T, et al. Treatment of unstable scaphoid waist nonunion with cancellous bone grafts and cannulated screw or Kirschner wire fixation. J Plast Surg Hand Surg. 2021 Jun;55(3):167-172. doi:10.1080/2000656X.2020.1856674
29. Daly K, Gill P, Magnussen PA, Simonis RB. Established nonunion of the scaphoid treated by volar wedge grafting and Herbert screw fixation. J Bone Joint Surg Br. 1996;78(4):530-534.
30. Radford PJ, Matthewson MH, Meggitt BF. The Herbert screw for delayed and non-union of scaphoid fractures: a review of fifty cases. J Hand Surg Br. 1990;15(4):455-459. doi:10.1016/0266-7681(90)90089-m
31. Rajagopalan BM, Squire DS, Samuels LO. Results of Herbert-screw fixation with bone-grafting for the treatment of nonunion of the scaphoid. J Bone Joint Surg Am. 1999;81(1):48-52. doi:10.2106/00004623-199901000-00007
32. Reigstad O, Grimsgaard C, Thorkildsen R, Reigstad A, Rokkum M. Long-term results of scaphoid nonunion surgery: 50 patients reviewed after 8 to 18 years. J Orthop Trauma. 2012;26(4):241-245. doi:10.1097/BOT.0b013e31821f940a
33. Wu J, Tay SC, Shin AY. The effect of screw design on union rates in scaphoid nonunions. Hand Surg. 2015;20(2):273-279. doi:10.1142/S0218810415500239
34. Trumble TE, Clarke T, Kreder HJ. Non-union of the scaphoid. Treatment with cannulated screws compared with treatment with Herbert screws. J Bone Joint Surg Am. 1996;78(12):1829-1837. doi:10.2106/00004623-199612000-00005
35. Tsuyuguchi Y, Murase T, Hidaka N, Ohno H, Kawai H. Anterior wedge-shaped bone graft for old scaphoid fractures or non-unions. An analysis of relevant carpal alignment. J Hand Surg Br. 1995;20(2):194-200. doi:10.1016/s0266-7681(05)80049-x
36. Pinder RM, Brkljac M, Rix L, Muir L, Brewster M. Treatment of scaphoid nonunion: a systematic review of the existing evidence. J Hand Surg Am. 2015;40(9):1797-1805.e3. doi:10.1016/j.jhsa.2015.05.003
37. Wozasek GE, Moser KD. Percutaneous screw fixation for fractures of the scaphoid (published correction appears in J Bone Joint Surg [Br] 1991 May;73(3):524). J Bone Joint Surg Br. 1991;73(1):138-142. doi:10.1302/0301-620X.73B1.1670499
38. Bond CD, Shin AY, McBride MT, Dao KD. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83(4):483-488. doi:10.2106/00004623-200104000-00001
39. Slade JF 3rd, Grauer JN, Mahoney JD. Arthroscopic reduction and percutaneous fixation of scaphoid fractures with a novel dorsal technique. Orthop Clin North Am. 2001;32(2):247-261. doi:10.1016/s0030-5898(05)70247-9
40. Dias JJ, Wildin CJ, Bhowal B, Thompson JR. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005;87(10):2160-2168. doi:10.2106/JBJS.D.02305
41. Arora R, Gschwentner M, Krappinger D, Lutz M, Blauth M, Gabl M. Fixation of nondisplaced scaphoid fractures: making treatment cost effective. Prospective controlled trial. Arch Orthop Trauma Surg. 2007;127(1):39-46. doi:10.1007/s00402-006-0229-z
42. Hegazy G. Percutaneous screw fixation of scaphoid waist fracture non-union without bone grafting. J Hand Microsurg. 2015;7(2):250-255. doi:10.1007/s12593-015-0194-2
43. Capo JT, Shamian B, Rizzo M. Percutaneous screw fixation without bone grafting of scaphoid non-union. Isr Med Assoc J. 2012;14(12):729-732.