Negative Pressure Wound Therapy for Complex Surgical Wounds in 59 Patients Across Secondary and Tertiary Care Centers in Turkey
Abstract
Background. Complex wounds are associated with a challenging healing process, prolonged hospitalization, increased treatment cost, and workforce loss. In this case series, negative pressure wound therapy (NPWT) with and without instillation and dwell time (NPWTi-d), closed incision negative pressure therapy (ciNPT), and open abdomen negative pressure therapy (OA-NPT) use in the management of complex wounds were examined.
Methods. Fifty-nine patients (mean age, 55.0 ± 14.8 years) across secondary and tertiary care centers in Turkey were treated. Patients were examined, and a NPWT system was selected based on wound care needs. Dressing changes occurred every 2 to 7 days, depending on therapy type. Wound closure occurred through surgical closure or secondary intention.
Results. Patient wound types consisted of acute wounds (n = 10), chronic wounds (n = 34), postoperative wound dehiscence (n = 9), and tumor resection/flap necrosis (n = 6). Thirty-six patients (61.0%) received NPWT, 16 (27.1%) received NPWTi-d, 5 (8.5%) received ciNPT, and 2 (3.4%) received OA-NPT. Average treatment duration was 19.7 ± 13.7 days. Surgical closure occurred in 45 patients, and secondary closure was observed in 13 patients; the remaining patient showed wound improvement. Wound healing complications were observed in 2 patients (scar formation and partial flap necrosis).
Conclusions. Our findings indicate an association of negative pressure therapy with favorable wound healing outcome in complex wounds. Negative pressure therapy seems to be a useful treatment option to bridge wound care between initial debridement and final reconstruction.
Introduction
Negative pressure wound therapy (NPWT) is based on the topical application of subatmospheric pressure through a vacuum source onto the wound bed filled with a porous dressing, creating a negative pressure environment in the wound.1,2 NPWT has become widely used in the management of complex wounds of various etiologies, such as open abdominal wounds, nonhealing wounds, and chronic wounds along with an expansion of clinical use over the last decade.1-6
NPWT has been available since the early 1990s and has evolved to include a range of devices, allowing the clinician to tailor NPWT to the wound. NPWT in open abdomen management (OA-NPT) and NPWT with instillation and dwell time (NPWTi-d) were introduced in the 2000s, offering a noted improvement in wound management options compared with standard wound care dressings.6-9 At the beginning of 2010, an NPWT system designed specifically for the application of negative pressure therapy on clean, closed incisions (closed incision negative pressure therapy [ciNPT]) became available.2,10,11
The efficacy of NPWT in wound management is associated with the generation of subatmospheric pressure in a closed system that results in increased exudate removal, reduction of edema, and promotion of granulation tissue formation.1,2,12 NPWTi-d cleanses the wound through the instillation of topical wound solutions and prepares the wound for closure.7 ciNPT helps to hold incision edges together, acts as a barrier to external contamination, and removes fluid and infectious materials.13 While OA-NPT provides separation between the abdominal wall and viscera, it also protects the abdominal contents, draws the wound edges together, provides a barrier against the external environment, and removes fluid from the paracolic gutters.14
The utility of negative pressure therapy in the management of complex wounds is considered critical given that these wounds are likely to have a delayed or complicated healing process and prolonged hospitalization, leading to increased treatment costs and considerable workforce loss.15 In this case series, we aimed to provide data on the utility of NPWT, NPWTi-d, ciNPT, and OA-NPT in the management of complex wounds based on the clinical experience of physicians from several disciplines at both secondary and tertiary care centers across Turkey.
Methods and Materials
This study was performed in accordance with the Declaration of Helsinki, and ethics approval was received from the Ethical Committee of Uludağ University (2011-KAEK-26/522). Negative pressure therapy devices used during patient care were selected by the clinician based on goals of therapy and institutional guidelines. Informed consent was obtained from patients for the use of patient data and images for publication purposes.
Patient Selection
The patients included in this retrospective analysis were treated with negative pressure therapy with sufficient care documentations throughout the study period (2015-2018).
NPWT
NPWT (3M V.A.C. Therapy using 3M V.A.C. Granufoam Dressing; 3M) was used to promote granulation tissue formation and prepare the wound for closure. When exposed bone or tendons were present in the wound bed, a nonadherent dressing was used to protect the fragile structures. The NPWT foam dressings were cut to size and placed in the wound bed, followed by application of a drape (3M V.A.C. Drape; 3M) and a negative pressure–sensing pad (3M SensaT.R.A.C. Pad; 3M). The negative pressure–sensing pad was connected to the NPWT device, and NPWT was initiated using continuous pressure between -50 mm Hg and -125 mm Hg. Dressing changes were performed every 24 to 72 hours.
When NPWT was used as a bolster for skin grafts, a polyvinyl alcohol dressing (3M V.A.C. Whitefoam Dressing; 3M) was used with continuous negative pressure at -125 mm Hg. Dressing changes occurred every 3 to 5 days.
NPWTi-d
For wounds in need of cleansing, NPWTi-d (3M Veraflo Therapy with 3M V.A.C. Veraflo Dressing; 3M) was used. When exposed bone or tendons were present in the wound bed, a nonadherent dressing was used to protect the fragile structures. The NPWTi-d dressing was sized to fit the wound, placed in the wound bed, and covered with a drape. The negative pressure and instillation pad was applied, and the tubing was connected to the NPWTi-d device. Normal saline was instilled into the wound bed with dwell times ranging from 5 to 20 minutes, followed by continuous negative pressure (-50 mm Hg to -125 mm Hg) for 1 to 3 hours. Dressing changes were performed every 24 to 72 hours.
ciNPT
ciNPT (3M Prevena Incision Management System) was used over clean, closed incisions to provide a barrier to external contamination, help hold incision edges together, and remove fluid from the incision site. Following incision closure, the dressing (3M Prevena Customizable Dressing; 3M) was cut to size and applied over the incision and connected to the device. Continuous negative pressure was initiated (-50 mm Hg to -125 mm Hg). The dressing was kept in place for 5 to 7 days.
OA-NPT
OA-NPT was used in patients requiring open abdomen management. OA-NPT (3M AbThera Open Abdomen Negative Pressure Therapy using 3M AbThera Perforated Foam; 3M) was applied according to the manufacturer’s instructions. A protective layer (3M AbThera Fenestrated Visceral Protective Layer; 3M) was cut to size and placed inside the abdominal compartment, covering all exposed viscera and tucked between the abdominal wall and the internal organs. The foam dressing was cut to size and placed over the protective layer. A drape (3M V.A.C. Drape; 3M) was applied over the periwound skin and foam dressing. A negative pressure–sensing pad (3M SensaT.R.A.C. Pad; 3M) was attached to the drape and connected to the OA-NPT device. OA-NPT was initiated using continuous negative pressure at -125 mm Hg with dressing changes every 24 to 72 hours.
Oxidized Regenerated Cellulose/Collagen Dressings
Oxidized regenerated cellulose (ORC)/collagen dressings (3M Promogran Collagen Matrix with ORC or 3M Promogran Prisma Collagen Matrix with ORC and silver; 3M) were used in 2 patients when a delay in wound healing was observed after discontinuation of negative pressure therapy. ORC/collagen dressings were utilized to promote granulation tissue formation and assist with wound bed preparation. The ORC/collagen dressing was cut to size and applied to the wound. A secondary dressing (3M Tielle Hydropolymer Adhesive Dressing; 3M) was applied over the ORC/collagen dressing. Dressing changes were not needed for the ORC/collagen dressings due to their ability to be absorbed into the wound bed. The secondary dressing was changed every 5 to 7 days, if needed.
Results

In this case series, 59 patients (mean age, 55.0 ± 14.8 years) with complex wounds requiring hospitalization were assessed. Wounds were characterized as acute (n = 10), chronic (n = 34), postoperative dehiscence (n = 9), and tumor resection/necrosis (n = 6) (Table 1). Thirty-six patients (61.0%) received NPWT, 16 (27.1%) received NPWTi-d, 5 (8.5%) received ciNPT, and 2 (3.4%) received OA-NPT. The average treatment duration was 19.7 ± 13.7 days, with NPWTi-d patients having the longest treatment duration (Table 1).
Wound closure occurred in 58 of 59 patients; the remaining patient showed wound improvement and was transferred to the intensive care unit for further medical care. Sixteen patients (27.6%) underwent wound closure through primary intention, 13 patients (22.4%) underwent wound healing through secondary intention, and the remaining 29 patients (50.0%) received flap or skin graft closure (Table 1). Wound healing complications were observed in 2 patients (scar formation and partial flap necrosis).
Representative Cases
Representative cases showing the use of NPWT, NPWTi-d, ciNPT, or OA-NPT are presented below.
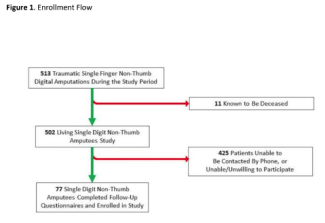
Case 1: Traumatic Leg Wound

A 31-year-old man was admitted to the emergency department following a car accident. Physical examination revealed open tibial fracture, impaired skin circulation, and tissue edema (Figure 1A). No full-thickness skin loss was observed. The patient underwent external fixator application and debridement for skin necrosis (Figure 1B-1C). No bone was exposed after debridement. As a partial skin defect occurred due to tissue edema, the treatment plan of NPWT use followed by skin graft procedure was utilized. To promote granulation tissue development in the wound bed and prepare the wound for skin grafting, NPWT was used. NPWT was applied with continuous negative pressure at -125 mm Hg. Dressing changes occurred every 3 days. After 30 days of NPWT, a split-thickness skin graft (STSG) was applied due to reduction in wound discharge and the achievement of sufficient granulation tissue (Figure 1C).
Case 2: Ischemic Diabetic Foot Wound

A 70-year-old man with diabetes, hypertension, and peripheral artery disease was hospitalized due to a stump wound in the amputated second and third digits of the left foot and an abscess at the sole of the foot (Figure 2A). Evaluation revealed stenosis below the popliteal level, monophasic flow in tibial artery, and an ankle brachial index level of 0.5. Revascularization could not be performed. Following successive debridements and antibiotic therapy regulation, NPWT with reticulated open cell foam with silver (ROCF-S)(3M V.A.C. Granufoam Silver Dressing; 3M) was applied to 11 × 2-cm2 wound area. Intermittent negative pressure at -125 mm Hg using 5 minutes on and 2 minutes off intervals was utilized. Dressing changes occurred every 3 days. Intermittent negative pressure was used due to the patient’s pain tolerance and the presence of wound ischemia. NPWT was utilized to promote the development of granulation tissue in the wound bed. After 3 days of NPWT, necrosis was noted in the wound site and first digit. Amputation of the first digit and a metatarsal head resection were performed (Figure 2B). Following debridement, NPWT with ROCF-S dressing was reapplied using intermittent negative pressure at -50 mm Hg with 4 minutes of negative pressure followed by 2 minutes of no negative pressure. Dressing changes occurred daily. NPWT was gradually increased to -100 mm Hg using intermittent negative pressure (intervals of 5 minutes on/2 minutes off) and dressing changes every 3 days with close ischemia control. Hyperbaric oxygen treatment (HBOT) was also utilized. After 57 days of NPWT, 58 sessions of HBOT, and infection control, the development of granulation tissue and reepithelialization were observed (Figure 2C). The wound underwent closure with an STSG and remained healed without complications 2 months after grafting (Figure 2D).
Case 3: Hidradenitis Suppurutiva

A 52-year-old man was admitted to our clinic with a 21-year history of hidradenitis suppurutiva, extending from the sacrum to the entire gluteal region and left thigh (Figure 3A). Magnetic resonance imaging revealed involvement of the left sacral region and entire perianal area. Initially, a large surgical excision was planned. Intraoperative assessment revealed complete involvement of the anococcygeal ligament, with dissemination around the coccyx (forming hard fibrous tissue on sacrum and channels), an abscess foci extending from the left lateral side of the sacrum to retroperitoneum, and focal involvement of the external anal sphincter muscle. Debridement was performed for bilateral gluteal regions with consideration of resection to the margins and preservation of the external anal sphincter as much as possible (Figure 3B). Afterwards, NPWT was applied (continuous negative pressure at -125 mm Hg) to promote granulation tissue development and prepare the wound for surgical closure and skin grafting. Dressing changes occurred every 3 days (Figure 3C). Primary closure of wound edges was performed to reduce defect size followed by reapplication of NPWT over the remaining open wound every 6 days for 18 days (Figure 3D-3E). After 18 days, the remaining open wound (approximately 8 × 6 × 4 cm3) on the sacrum was closed with STSG derived from the posterior surface of the left thigh (Figure 3F-3G). Overall duration of treatment was 35 days without deviating colostomy creation. After treatment with NPWT was discontinued, pathological findings revealed well-differentiated squamous cell carcinoma arising from hidradenitis suppurutiva. Related chemo/radiotherapy protocols were initiated (Figure 3H). It should be noted that malignancy is contraindicated for NPWT use; in this case, however, malignancy was not identified until after treatment had concluded.
Case 4: Postoperative Wound Dehiscence and Necrosis of Repair Flap

A 70-year-old woman had previously undergone several surgical debridement procedures for postoperative discharge after right total hip prosthesis within the year before presentation at our facility. The wound dehiscence defect was repaired with a gastrocnemius flap, and the patient was discharged. However, the patient was rehospitalized 2 to 3 weeks later due to flap necrosis (Figure 4A). The patient underwent surgical debridement followed by application of NPWT (continuous negative pressure at -125 mm Hg) with ROCF-S dressings (Figure 4B). NPWT was used to promote the development of wound bed granulation tissue and prepare the wound for a skin graft procedure. Dressing changes occurred every 3 days. After 6 days of NPWT, ROCF-S dressings were discontinued and ROCF dressings applied (Figure 4C). After 12 days of NPWT, a STSG procedure was performed (Figure 4D). Fifteen days after grafting, the wound showed signs of healing without complications, and the patient was discharged (Figure 4E-4F).
Case 5: Traumatic Scalp Defect

An 18-year-old man was admitted to emergency department following a motor vehicle accident. Physical examination revealed mandibular deformity and malocclusion as well as a 15 × 8–cm2 right parietotemporal scalp defect with exposed bone (10 × 6 cm2) (Figure 5A). Further assessment revealed presence of double fracture of the mandible, laceration of the spleen, and cervical vertebrate fracture. After control of life-threatening conditions, the patient underwent same-session surgery for mandible fracture repair and scalp defect debridement. A nonadherent dressing was used to protect the exposed skull. NPWTi-d was used to help cleanse the wound and remove debris. NPWTi-d was initiated over the scalp defect, consisting of 50 µL isotonic saline with a 5-minute dwell time, followed by 4 hours of negative pressure at -125 mm Hg (Figure 5B). Dressing changes occurred every 3 days. After 12 days of NPWTi-d, primary closure of the skin was performed (Figure 5C-5D). The patient had no wound complications other than a scar on the scalp observed during a 2-year follow-up visit (Figure 5E).
Case 6: Fournier’s Gangrene

A 57-year-old woman was admitted to the emergency department with signs of Fournier’s gangrene and diabetic ketoacidosis. Physical examination revealed necrosis extending from perianal area to left inguinal and lumbar regions as well as a fluctuating abscess progressing through the entire fascial plane. Systemic antibiotics were initiated. Surgical debridement of fascial planes was followed by application of NPWTi-d (Figure 6A-6B). NPWTi-d was used to cleanse the wound and help remove exudate and infectious materials from the wound bed. Normal saline was instilled into the wound bed with a 5-minute dwell time, followed by -125 mm Hg negative pressure for 2 hours. Dressing changes occurred every 2 days. A fecal management system was used to prevent contamination of the wound bed. After 24 days of NPWTi-d, the patient underwent surgical closure of the wound (Figure 6C). The patient was discharged with a full recovery without the need for a colostomy (Figure 6D).
Case 7: Anterior Thoracic Wall Reconstruction

A 50-year-old man presented for care with an early postoperative local recurrence following resection surgery for an anterior thoracic wall soft tissue sarcoma and reconstruction via local flaps (Figure 7A-7B). Flap reconstruction was performed, followed by application of ciNPT using -75 mm Hg negative pressure (Figure 7C). ciNPT was chosen for use to help hold the incision edges together and provide a barrier to external contamination. Dressing changes occurred every 3 days. After 9 days of ciNPT use, the patient was discharged. The incisions remained intact without complications on postoperative day 60 (Figure 7D).

Case 8: Open Abdominal Wound After Colon Mass Excision
A 67-year-old man underwent colon mass excision surgery with supra- and infra-umbilical median incision and descending colon loop colostomy. The patient was admitted to our clinic due to postoperative infection, full-thickness necrosis of the anterior abdominal wall, colostomy dehiscence, and distension development (Figure 8A). Abdominal compartment syndrome and anterior abdominal wall necrosis were diagnosed. Intraoperatively, intestinal edema and free fluid were noted (Figure 8B). Peritoneal cavity washing, debridement of anterior abdominal wall, and loop colostomy revision were performed. OA-NPT was used to remove fluid and help reduce edema, provide medial tension to help reduce fascial retraction and loss of domain, and to provide a separation between the abdominal wall and viscera. OA-NPT was applied with continuous negative pressure at -125 mm Hg, and dressings were changed every 3 days (Figure 8C). Use of OA-NPT resulted in dramatic reduction in the edema of the intra-abdominal organs and in the abdominal wall defect size (Figure 8D-8E). After 12 days of OA-NPT, a 15 × 10–cm2 defect was closed by partial-thickness skin graft. Full wound healing was observed 21 days after the first debridement surgery (Figure 8F).
Discussion
Complex wounds are associated with a challenging healing process, prolonged hospitalization, increased treatment cost, and considerable workforce loss.15 While many treatment options exist, NPWT has become widely used in the management of complex wounds with various etiologies.1-6 As the use of NPWT has expanded, the strategy has evolved to include several different configurations to allow for treatment tailored to the wound. In this case series of 59 patients, we aimed to provide data on the utility of NPWT, NPWTi-d, ciNPT, and OA-NPT in the management of complex wounds at secondary and tertiary care centers across Turkey. Our findings indicated favorable patient outcomes with the use of negative pressure therapy devices in combination with surgical debridement.
Thirty-six patients received NPWT for management of wounds that included diabetic foot ulcers, necrotizing fasciitis, and surgical dehiscence. All patients experienced wound healing without complications following successful surgical closure or grafting. These results are similar to those seen in previously published studies that examined the use of NPWT for the management of necrotizing fasciitis, head and neck wounds, or surgical dehiscence.16-18 In these studies, successful wound closure without complications was reported. Additionally, a meta-analysis examining the use of NPWT in the management of diabetic foot ulcers reported reduced healing time, wound area, and amputation rates associated with the use of NPWT compared with standard wound care dressings.19
In some of our patients, a lower negative pressure was utilized due to the presence of tissue ischemia. One patient with a diabetic ischemic wound displayed a progression to wound necrosis after NPWT at -125 mm Hg. Wound healing was improved when the pressure was reduced to -50 mm Hg and progressively increased to -100 mm Hg. This emphasizes the potential benefit of starting with low pressures and gradually increasing the negative pressure in the management of ischemic wounds, depending on the patient’s pain tolerance and the response of the wound.1,20
NPWTi-d was chosen for use in 16 patients with wounds ranging from ulcers to Fournier’s gangrene. In these patients, NPWTi-d offered wound cleansing with removal of debris and infectious materials, and the wound bed was prepared for closure. Wound closure was successful with no complications in a majority of patients. These results are similar to those seen in previous studies.9,21,22 In a case series involving 3 patients of Middle Eastern ethnicity, Ben-Nakhi et al used NPWTi-d to cleanse the wound bed and prepare the wounds for closure, resulting in reduced trips to the operating room and development of healthy granulation tissue.9 Similarly, Dieham et al utilized NPWTi-d in 30 patients requiring wound cleansing; this approach resulted in increased granulation tissue development and successful reconstruction in 90% of patients.21 A single case report noted reduction of operating room visits and increased granulation tissue development following use of NPWTi-d in a patient with necrotizing fasciitis.22 A meta-analysis examining the effectiveness of NPWTi-d observed complete healing in 93.65% of patients following use of NPWTi-d.23 Our results and those of the published literature indicate that NPWTi-d can provide positive clinical benefits when used in wounds needing cleansing.
In our study, ciNPT was applied over closed incisions in 5 patients. The use of ciNPT resulted in fully healed, closed incisions without complications in 4 patients. The fifth, patient who had undergone deep inferior epigastric perforator flap reconstruction surgery following mastectomy, developed partial flap necrosis. However, this patient had displayed graft failure complications during treatment, indicating that the flap complication was likely due to an underlying comorbidity. Flap debridement and surgical closure was performed along with application of a nitroglycerine patch and use of ciNPT with a lower negative pressure. This modification resulted in resolution of flap congestion and ultimate healing without further complications. None of the patients developed surgical site infection (SSI), supporting previously published literature reporting the association of ciNPT with reduced rates of SSIs.10,11,24-26 Similarly, the application of ciNPT in 504 patients with lower extremity incisions was reported to be associated with significantly decreased rate of SSIs as compared with standard dressings.27
In our case series, the use of OA-NPT resulted in amelioration of intestinal edema and reduction in abdominal wall defect size in a patient with abdominal compartment syndrome and anterior abdominal wall necrosis after colon mass excision surgery. This result was similar to those previously reported in the literature.8,28,29 In these studies, OA-NPT was utilized in patients with intra-abdominal hypertension or abdominal compartment syndrome. OA-NPT was reported to protect the abdominal contents without further increases in abdominal pressure while removing large amounts of exudate and promoting primary closure of the fascia without repeated laparotomy procedures.8,28,29 These positive results are most likely due to the OA-NPT providing separation between the abdominal wall and the viscera, protecting the abdominal contents from the external environment, actively removing fluid and reducing edema, and providing medial tension to help minimize fascial retraction and loss of domain.14
In patients with more complex wounds, improved wound healing was observed after the combined use of negative pressure therapy approaches. The combined approaches included surgical debridement along with the sequential use of NPWTi-d and NPWT. In patients with multiple therapy treatment plans, wound closure was successful without complication. Here, the negative pressure therapy plan was revised to match the wound bed requirements as the wounds improved. In a small case series from Rupert et al, 4 patients received NPWTi-d followed by NPWT before surgical closure via grafts or flaps.30 NPWTi-d was used to cleanse the wounds, and NPWT was then initiated to promote granulation tissue development.30 This treatment combination resulted in successful surgical closure in all 4 patients without complications, similar to the results observed in our 2 patients who received combination therapy.
Limitations
Limitations exist for this study. The results of this large case series are limited due to the retrospective nature of the study and a lack of a control population. The retrospective nature of the study may introduce patient selection bias. The authors attempted to prevent any bias by selecting all patients with complex wounds who presented for care during the designated time period for inclusion into the study. Additionally, the lack of control patients limits a full assessment of clinical outcomes following treatment. As such, the study results may not be applicable to all patient populations. Large-scale randomized controlled studies are needed to further assess the efficacy of NPWT, NPWTi-d, ciNPT, and OA-NPT in the management of complex wounds.
Conclusions
Our findings support the association of negative pressure therapy use with favorable wound management outcomes in complex wounds. Alongside its potential beneficial effect on reducing the risk of wound site infection and tissue edema, negative pressure therapy, in all forms, seems to be a useful treatment option that can bridge patient care between initial debridement and final reconstruction with grafts and flaps. Our findings emphasize the utility of several wound therapy approaches in combination with negative pressure therapy in the management of more complex wounds, as well as the importance of tailoring the treatment plan to the needs of the patient and wound. Large-scale randomized controlled studies are needed to further assess the efficacy of the various negative pressure therapy configurations in the management of complex wounds.
Acknowledgments
The Turkish Wound Working Group includes: Abdullah Etöz, MD, and Muhammed Eren Şimşek, MD (Acibadem Bakirkoy Hospital, Istanbul); Savaş Serel, MD (Ankara University, Ankara); Hilal Çoban, MD; Ayfer Ekinci, MD; İdris Kurtuluş, MD; Derya Kuyucu, MD; and Nurettin Uzer, MD (Basaksehir State Hospital, Istanbul, and Diskapi Yildirim Beyazit Training and Research Hospital, Ankara); Özkan Balçin, MD (Bursa State Hospital, Bursa); Melih Akıncı, MD; Fatma Aybala Altay, MD; Sultan Ayaz, MD; Şener Balas, MD; Abdurrahman Başpınar, MD; Yenel Bilgetekin, MD; Taner Bostancı, MD; Nurhak Cihangir Çıngıl, MD; Merve Nergis Fidan, MD; Harun Karabacak, MD; İsmail Oskay Kaya, MD; Hatice Mustafayeva, MD; Alper Bilal Özkardeş, MD; Mehmet Saydam, MD; Fatih Sancak, MD; Turgay Sayin, MD; Hakan Sönmez, MD; Faruk Yazıcı, MD; İbrahim Yilmaz, MD; Kerim Bora Yılmaz, MD; and Hikmay Zeynalov, MD (Diskapi Yildirim Beyazit Training and Research Hospital, Ankara); Ali Cem Akpınar, MD; Salih Cem Altunal, MD; Çağla Amutkan Çiçek, MD; Şüheda Çıldır, MD; Bükem Cüce, MD; Recep Demirhan, MD; Gaye Taylan Filinte, MD; Emre Güvercin, MD; Tufan Hiçdönmez, MD; Barış Kanık, MD; Atilla Özdemir, MD; Kadir Burak Özer, MD; Cem Berkay Sınacı, MD; Gökhan Temiz, MD; Tunç Tunçbilek, MD; and Murat Yaman, MD (Dr. Lutfu Kirdar Training and Research Hospital, Istanbul); A. Emre Koçman, MD; Aydan Köse, MD; and Cengiz Çetin, MD (Eskisehir Osmangazi University, Eskisehir); Murat Kendirci, MD, and İbrahim Tayfun Şahiner, MD (Hitit University, Çorum); Halil Alış, MD; Süleyman Büyükaşık, MD; and Burak Kankaya, MD (Istanbul Aydin University, Istanbul); Naciye Çiğdem Arslan, MD, and Yaşar Özdenkaya, MD (Istanbul Medipol University, Istanbul); Şamil Aktaş, MD, and Bengisu Mirasoğlu, MD (Istanbul University, Istanbul); Ersin Akşam, MD (Izmir Katip Celebi University, Izmir); Gürkan Çalışkan, MD; Cemil Ertürk, MD; Sabri Kerem, MD; Adem Şahin, MD; and Ahmet Şahin, MD (Kanuni Sultan Süleyman Training and Research Hospital, Istanbul); Ömer Günal, MD; Nihal Durmuş Kocaaslan, MD; Melekber Cavus Özkan, MD; Evrim Şirin, MD; and Oytun Derya Tunç, MD (Marmara University, Istanbul); Fatih Dikici, MD; Halil Can Gemalmaz, MD; İbrahim Kaya, MD; Kerim Sarıyılmaz, MD; and Mustafa Sungur, MD (Mehmet Ali Aydinlar University, Istanbul); Mehmet Karakayalı, MD (Sultanbeyli Hospital, Istanbul); and Ayhan Sönmez, MD (Unye State Hospital, Ordu).
We extend thanks to Cagla Ayhan, MD and Prof Sule Oktay, MD, PhD, from KAPPA Consultancy Training Research Ltd, Istanbul, who provided editorial support funded by Acelity Turkey. We also thank Julie M Robertson, PhD (3M) for assistance with manuscript editing.
Affiliations: 1Department of Plastic Reconstructive and Aesthetic Surgery, Bursa Uludağ University, Bursa, Turkey;2Members of the Turkish Wound Working Group are listed in the Acknowledgments.
Correspondence: Ramazan Kahveci, MD; kahveci@uludag.edu.tr
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics: Approval for this study was received from the Ethical Committee of Uludağ University (2011-KAEK-26/522).
Disclosures: The authors declare that they have no conflict of interest.
References
1. Apelqvist J, Willy C, Fagerdahl AM, et al. Negative pressure wound therapy - overview, challenges and perspectives. J Wound Care. 2017;26(Suppl. 3):S1-S113. doi:10.12968/jowc.2017.26.Sup3.S1
2. Matusiak D, Wichtowski M, Pieszko K, Kobylarek D, Murawa D. Is negative-pressure wound therapy beneficial in modern-day breast surgery? Contemp Oncol (Pozn). 2019;23(2):69-73. doi:10.5114/wo.2019.85199
3. Bovill E, Banwell PE, Teot L, et al. Topical negative pressure wound therapy: a review of its role and guidelines for its use in the management of acute wounds. Int Wound J. 2008;5(4):511-529. doi:10.1111/j.1742-481X.2008.00437.x
4. Orgill DP, Bayer LR. Update on negative-pressure wound therapy. Plast Reconstr Surg. 2011;127(Suppl 1):105S-115S; discussion 116S. doi:10.1097/PRS.0b013e318200a427
5. Blume PA, Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care. 2008;31(4):631-636. doi:10.2337/dc07-2196
6. Acosta S, Bjarnason T, Petersson U, et al. Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg. 2011;98(5):735-743. doi:10.1002/bjs.7383
7. Kim PJ, Attinger CE, Crist BD, et al. Negative pressure wound therapy with instillation: review of evidence and recommendations. Wounds. 2015;27(12):S2-S19.
8. Fernandez LG, Matthews MR. Clinical observations in patients with open abdomens managed with negative pressure therapy using a perforated foam dressing: a limited case series with brief literature review. Wounds. 2021; doi:10.25270.wnds/082421.02
9. Ben-Nakhi ME, Eltayeb HI. First Middle East experience with novel foam dressing together with negative pressure wound therapy and instillation. Cureus. 2018;10(10):e3415. doi:10.7759/cureus.3415
10. Tyagi V, Kahan J, Huang P, Li D, Gibson D. Negative pressure incisional therapy and postoperative infection after posterior approach primary total hip arthroplasty. Cureus. 2020;12(3):e7394. doi:10.7759/cureus.7394
11. Poehnert D, Hadeler N, Schrem H, Kaltenborn A, Klempnauer J, Winny M. Decreased superficial surgical site infections, shortened hospital stay, and improved quality of life due to incisional negative pressure wound therapy after reversal of double loop ileostomy. Wound Repair Regen. 2017;25(6):994-1001. doi:10.1111/wrr.12606
12. Saxena V, Hwang CW, Huang S, Eichbaum Q, Ingber D, Orgill DP. Vacuum-assisted closure: microdeformations of wounds and cell proliferation. Plast Reconstr Surg. 2004;114(5):1086-1096. doi:10.1097/01.prs.0000135330.51408.97
13. Wilkes RP, Kilpadi DV, Zhao Y, Kazala R, McNulty A. Closed incision management with negative pressure wound therapy (CIM): biomechanics. Surg Innov. 2012;19(1):67-75. doi:10.1177/1553350611414920
14. Atema JJ, Gans SL, Boermeester MA. Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in non-trauma patients. World J Surg. 2015;39(4):912-925. doi:10.1007/s00268-014-2883-6
15. Milcheski DA, Portocarrero ML, Alvarez DM, Mazuca LGMP, Monteiro AA, Jr., Gemperli R. Initial experience with negative-pressure wound therapy with instillation in complex wounds. Revista do Colegio Brasileiro de Cirurgioes. 2017;44(4):348-353. doi:10.1590/0100-69912017004008
16. Zhang N, Yu X, Zhang K, Liu T. A retrospective case series of Fournier’s gangrene: necrotizing fasciitis in perineum and perianal region. BMC Surg. 2020;20(1):259. doi:10.1186/s12893-020-00916-3
17. Satteson ES, Crantford JC, Wood J, David LR. Outcomes of vacuum-assisted therapy in the treatment of head and neck wounds. J Craniofac Surg. 2015;26(7):e599-e602. doi:10.1097/SCS.0000000000002047
18. Seidel D, Diedrich S, Herrle F, et al. Negative pressure wound therapy vs conventional wound treatment in subcutaneous abdominal wound healing impairment: the SAWHI randomized clinical trial. JAMA Surg. 2020;155(6):469-478. doi:10.1001/jamasurg.2020.0414
19. Liu S, He CZ, Cai YT, et al. Evaluation of negative-pressure wound therapy for patients with diabetic foot ulcers: systematic review and meta-analysis. Ther Clin Risk Manag. 2017;13:533-544. doi:10.2147/tcrm.S131193
20. Wackenfors A, Gustafsson R, Sjogren J, Algotsson L, Ingemansson R, Malmsjo M. Blood flow responses in the peristernal thoracic wall during vacuum-assisted closure therapy. Ann Thorac Surg. 2005;79(5):1724-1731. doi:10.1016/j.athoracsur.2004.10.053
21. Diehm YF, Loew J, Will PA, et al. Negative pressure wound therapy with instillation and dwell time (NPWTi-d) with V.A.C. VeraFlo in traumatic, surgical, and chronic wounds-A helpful tool for decontamination and to prepare successful reconstruction. Int Wound J. 2020;17(6):1740-1749. doi:10.1111/iwj.13462
22. Reider K, McElroy E, Lemay S. The use of negative pressure with instillation and dwell for the treatment of necrotizing fasciitis. Cureus. 2018;10(10):e3515. doi:10.7759/cureus.3515
23. Kanapathy M, Mantelakis A, Khan N, Younis I, Mosahebi A. Clinical application and efficacy of negative pressure wound therapy with instillation and dwell time (NPWTi-d): A systematic review and meta-analysis. Int Wound J. 2020;17(6):1948-1959. doi:10.1111/iwj.13487
24. Cantero R, Rubio-Perez I, Leon M, et al. Negative-pressure therapy to reduce the risk of wound infection following diverting loop ileostomy reversal: an initial study. Adv Skin Wound Care. 2016;29(3):114-118. doi:10.1097/01.ASW.0000480458.60005.34
25. Grauhan O, Navasardyan A, Tutkun B, et al. Effect of surgical incision management on wound infections in a poststernotomy patient population. Int Wound J. 2014;11(Suppl 1):6-9. doi:10.1111/iwj.12294
26. Gabriel A, Sigalove S, Sigalove N, et al. The impact of closed incision negative pressure therapy on postoperative breast reconstruction outcomes. Plast Reconstr Surg Glob Open. 2018;6(8):e1880. doi:10.1097/GOX.0000000000001880
27. Benrashid E, Youngwirth LM, Guest K, Cox MW, Shortell CK, Dillavou ED. Negative pressure wound therapy reduces surgical site infections. J Vasc Surg. 2020;71(3):896-904. doi:10.1016/j.jvs.2019.05.066
28. Fitzgerald JE, Gupta S, Masterson S, Sigurdsson HH. Laparostomy management using the ABThera open abdomen negative pressure therapy system in a grade IV open abdomen secondary to acute pancreatitis. Int Wound J. 2013;10(2):138-144. doi:10.1111/j.1742-481X.2012.00953.x
29. Plaudis H, Rudzats A, Melberga L, Kazaka I, Suba O, Pupelis G. Abdominal negative-pressure therapy: a new method in countering abdominal compartment and peritonitis – prospective study and critical review of literature. Ann Intensive Care. 2012;2(Suppl 1):S23. doi:10.1186/2110-5820-2-S1-S23
30. Rupert P, Ochoa RA, Punch L, Van Epps J, Gordon-Burroughs S, Martinez S. The use of NPWT-i technology in complex surgical wounds. Cureus. 2016;8(12):e920. doi:10.7759/cureus.920