The Lawnmower and the Pediatric Lower Extremity: A Catastrophic Combination
© 2024 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Lower extremity (LE) trauma within the pediatric population may be debilitating and have different implications and etiologies than in adults. Specifically, lawnmower injuries can cause catastrophic sequelae to the lower extremities, often requiring complex reconstruction or resulting in amputation. This study aims to present our experience with pediatric LE lawnmower injuries at one of the busiest level 1 trauma centers in the United States.
Methods. An IRB-approved retrospective analysis was performed studying pediatric patients (age <18 years) who experienced LE trauma due to a lawnmower injury over a 5-year period (2012-2017). Patient demographics, perioperative data, and types of reconstruction were reviewed. Univariate analysis of the data was performed to examine trends in exposure and management of pediatric LE lawnmower injuries.
Results. Twenty-three patients were identified with pediatric LE lawnmower injuries, of whom 82.6% were male. The patients had a median age of 6 years and a median Injury Severity Score (ISS) of 4. Over one-third (34.8%) of this cohort required immediate amputation. Additionally, 26.1% and 8.7% required local and free flap reconstruction, respectively. In comparison, only 3.6% and 2.3% of all traumatic pediatric LE injuries from the same time frame required local and free flaps, respectively.
Conclusions. Lawnmower injuries to the LE can be devastating, causing long-term physical, emotional, and psychosocial consequences for pediatric patients and their families. The data in this study suggest that pediatric LE injuries from lawnmowers more often require complex reconstruction than other traumatic LE injuries. Rapid and effective decision-making by experienced surgeons is necessary to optimize the potential for limb salvage in pediatric LE lawnmower injuries. An algorithm of recommendations on when to transfer these types of injuries to more experienced tertiary centers is provided. Additional resources should be dedicated toward improving public awareness and industrial safety features to help prevent lawnmower injuries in pediatric patients.
Introduction
Pediatric lower extremity (LE) trauma can be devastating and is derived from a wider variety of etiologies than in the adult population. While adult LE injuries often occur at work, a recent study by Fallah et al demonstrated that pediatric LE injuries frequently occur during recreational activities, such as while riding all-terrain vehicles.1
Lawnmower-related injuries are the third leading cause of traumatic amputations in children, with riding rather than push mowers being of particular concern.2,3 Though easily preventable, according to the United States Consumer Product Safety Commission’s National Electronic Injury Surveillance System (NEISS) database, over 9000 lawnmower-related injuries occur annually in people younger than 18 years of age.4 Over the last 3 decades, this incidence has remained relatively unchanged, suggesting a failure in public health and prevention strategies.5,6
One study examining the National Trauma Data Bank between 2007 and 2011 found that lawnmowers were responsible for 12.1% of pediatric amputations.2 Furthermore, Lee et al found that 2 predictors of prolonged hospital stay and increased number of procedures in pediatric LE injuries are younger age and riding lawnmowers.8 Additionally, over half of patients injured by a lawnmower require at least 1 surgical amputation (foot, leg, arm, or hand) during their hospital stay.9 Many patients ultimately require complex reconstruction, including local or free flaps.
Pediatric LE lawnmower injuries have complex injury patterns and are resource-intensive, requiring multidisciplinary collaboration. We aim to identify trends in management of pediatric LE lawnmower injuries, improve public education about lawnmower safety, and streamline health care referrals to tertiary care centers.
Methods and Materials
Following institutional review board approval (IRB No. HSC-MS-19-0038), a retrospective study was conducted to review the records of all pediatric patients (<18 years old) who presented over a 5-year period (2012-2017) with LE trauma due to a lawnmower injury. Patients were identified with the following diagnosis codes: ICD9 E920.0 and ICD10 W28.XXA. Relevant demographics, perioperative data, and operative interventions were recorded. Demographic information of interest included age, sex, race, and mode of arrival. The timing of presentation from injury to arrival at our facility was inconsistently documented, so this information was not included in this study. Otherwise, perioperative information included relevant patient histories, surgical trauma team activation, Injury Severity Score (ISS), wound size, time to reconstruction, number of irrigation and/or debridement procedures before reconstruction, and total number of procedures, including all irrigation and/or debridement procedures and the final reconstruction procedure.10 Types of reconstruction were categorized as simple reconstruction, defined as primary or delayed primary closure, skin grafting, local flap, free flap, or amputation. For this study, amputation refers to immediate amputation and does not account for patients who underwent another type of reconstruction such as free flap before ultimately requiring an amputation. All data were collected and stored in a secured database, and univariate analysis was performed using Microsoft Excel.
Results
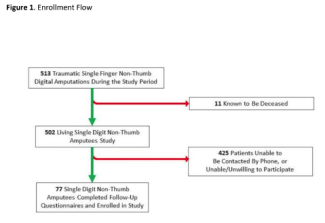
Within the specified study period, there were 1821 pediatric patients at our institution who presented with LE trauma. Among these patients, 23 patients presented specifically with a lawnmower injury to at least one LE (Figure 1). Of these, 82.6% and 17.4% were male and female, respectively. The median age was 6 years (interquartile range [IQR], 4-13.75 years). Eleven (47.8%) of the 23 patients were Caucasian, 7 (30.4%) Hispanic, 4 (17.4%) African American, and 1 (4.3%) Asian. Patient demographics are summarized in Table 1.


Twelve (52.2%) of the patients were brought in by emergency air ambulance and 7 (30.4%) were transferred in from other lower-acuity hospitals. The surgical trauma team was activated for 13 (56.5%) patients. The median ISS and wound size were 4 (IQR, 4-5) and 100 cm2 (IQR, 79.75-242 cm2), respectively. The median number of days to reconstruction was 2 days (IQR, 0.5-9.5 days). Most of the patients required at least 1 irrigation and/or debridement procedure before definitive reconstruction. The mean number of procedures performed prior to reconstruction was 3.1 (standard deviation [SD] 2.6). The mean number of total procedures performed was 3.7 (SD 3.2); this includes all irrigation and/or debridement procedures and definitive reconstruction. All perioperative and surgical data are summarized in Table 2.

Six (26.1%) patients ultimately received a simple reconstruction (ie, primary closure), 1 (4.3%) underwent a skin graft, 6 (26.1%) underwent a local flap, 2 (8.7%) had a free flap, and 8 (34.8%) required immediate amputation. Examples of the lawnmower injuries encountered and the subsequent reconstructions they received can be seen in Figures 2 through 4.



Discussion
By volume and emergency room visits, our institution is one of the busiest level 1 trauma centers in the nation, located in one of the most diverse cities in the country and serving a socioeconomically varied population. In our cohort, more than one-third of patients required immediate amputation after suffering a LE lawnmower injury. A recent analysis of pediatric traumatic amputations reinforces lawnmowers as a major source of amputations, particularly in children aged 0 to 5 years old.5 While some pediatric amputees regain good mobility and function with lower limb prostheses, it is important to acknowledge the potentially damaging long-term physical, mental, emotional, and psychosocial effects of amputation at an early age. In addition, these injuries are frequently, unwittingly inflicted by close family members and caretakers, creating prolonged feelings of guilt, clinical depression, and anxiety.
For pediatric patients fortunate enough to avoid an immediate amputation, the road to full recovery can still be long and arduous as these patients need adequate debridement prior to definitive reconstruction, close postoperative monitoring to ensure adequate graft or flap survival, and prolonged rehabilitation. As expected, many of the patients from our study required at least 1 debridement before definitive reconstruction. Once the wound was ready for reconstruction, one-third of patients ultimately required complex reconstruction in the form of a local or free flap. Interestingly, when comparing injuries in our current study to all pediatric LE traumatic injuries encountered at our institution during the same time frame as previously reported by Fallah et al,1 26.1% and 8.7% of patients from our study required a local flap or free flap compared with 3.6% and 2.3%, respectively. In addition, the median age in our cohort was 6 years compared with 10 years as previously reported by Fallah et al.1 This suggests that younger patients may be particularly vulnerable to lawnmower injuries.
For pediatric patients with lawnmower injuries to the LE, rapid and effective decision-making by experienced surgeons is needed to optimize the potential for limb salvage. Due to the immediately available resources, high-volume experience, and refined surgeon expertise observed at tertiary institutions, we believe that high-volume level 1 trauma centers are best equipped to handle complex LE lawnmower injuries. This setting allows for plastic surgeons to collaborate directly with orthopedic surgeons, vascular surgeons, and pediatric trauma surgeons to explore all available options for timely reconstruction. In a recent study of over 700 pediatric patients with traumatic vascular injuries to the upper or lower limbs, Prieto et al demonstrated significantly lower amputation and mortality rates in pediatric trauma patients treated at American College of Surgeons (ACS)–verified trauma centers compared with centers without ACS verification.11 Other important resources that may not be readily available at institutions with low-volume pediatric trauma include pediatric psychosocial support such as pediatric care teams and psychiatrists, as well as pediatric rehabilitation therapists. The senior authors (PN and WC) have, therefore, compiled a list of recommendations based on their experience at our high-volume trauma center to guide providers at lower acuity institutions in determining when to transfer these patients to a larger trauma center (Figure 5).

In addition to the previously discussed physical and mental/psychosocial effects, the financial impact of lawnmower injuries can also be significant. Factors observed in our study that can contribute to high health care costs include transportation, such as emergency air ambulance, need for multiple procedures, prolonged hospitalization, and need for complex reconstruction, which often requires expensive specialized equipment and long operative times. After discharge from the hospital, rehabilitation and prosthetic needs can contribute further to overall health care cost. Therefore, it is important to dedicate adequate resources toward educating parents and caregivers on the risk of lawnmower injuries in order to prevent the long-term consequences associated with these injuries in pediatric patients.
Public awareness and education about safety features are crucial and may help reduce the incidence of pediatric lawnmower injuries. Despite existing literature on the significant effects of lawnmower injuries on morbidity and mortality, their incidence did not decline between 1990 and 2013,5,6,12 and increased efforts are needed to promote injury prevention and public awareness.3,5 Important safety recommendations include wearing sturdy, closed-toed shoes around lawnmowers and not allowing children to ride as passengers, as previously summarized by Kansa et al (Table 3).7 We believe that increased awareness of these safety recommendations may help lower the incidence of pediatric lawnmower injuries. Table 3 is a summary list of existing recommendations for lawnmower industrial standards to ensure uniform operating conditions in the United States, adapted from a prior publication by Khansa et al.7

In addition to increased public awareness of safety features and regulations, local and national legislation should be passed to mandate and enforce safety features from a manufacturing standpoint. Currently, public safety recommendations regarding lawnmowers are voluntary and not federally mandated. For example, the American National Standards Institute’s and Outdoor Power Equipment Institute’s standards were updated in 2003 to include a feature that does not allow mowers to reverse, but unfortunately this feature can be temporarily disabled.13-15 As a result, lawnmowers can be steered backwards with the blades still engaged. To codify these safety standards, physicians and community members must work together to engage lawmakers and the public through a mix of public education, legislation advocacy, media, and retail promotion.
Limitations
There are limitations to this study that warrant recognition. The study was limited to a single institution with a small sample size, which brings into question the generalizability of our results. In the same respect, this is a retrospective study, and it is difficult to account for differences in individual physician practice or other potential unmeasured confounders. Additionally, this study only includes patients who were managed at our level 1 trauma center. Therefore, patients inflicted with minor wounds who did not require transfer for a higher level of care were not included in this study. This leaves potential for selection bias as our patient group may be skewed toward greater injury severity than would otherwise be observed. Furthermore, the trauma database we used for patient identification may have inadvertently omitted patients by error or because of coding issues. It is impossible for us to know if patients who were inadvertently omitted from the database would have been significantly different from our present cohort.
Conclusions
Lawnmower injuries pose a severe threat to limb viability and render a variety of damaging long-term consequences to pediatric patients and their families. Adequate resources should be dedicated toward improving public awareness and industrial safety regulations.
Acknowledgments
Affiliations: 1Division of Plastic and Reconstructive Surgery, Department of Surgery, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, Texas; 2Division of Plastic Surgery, Department of Surgery, Indiana University School of Medicine, Indianapolis, Indiana; 3Division of Plastic Surgery, Department of Surgery, University of Colorado School of Medicine, Aurora, Colorado; 4Department of Pediatric Plastic Surgery, Children’s Hospital Colorado, Aurora, Colorado
Correspondence: Phuong D. Nguyen, MD, FACS, FAAP; phuong.nguyen@childrenscolorado.org
Ethics: IRB number HSC-MS-19-0038
Disclosures: The authors declare that we have no relevant disclosures.
References
- Fallah KN, Konty LA, Anderson BJ, et al. Forecasting the flap: predictors for pediatric lower extremity trauma reconstruction. Arch Plast Surg. 2022;49(1):91-98. doi:10.5999/aps.2021.00675
- Borne A, Porter A, Recicar J, Maxson T, Montgomery C. Pediatric traumatic amputations in the United States: a 5-year review. J Pediatr Orthop. 2017;37(2):e104-e107. doi:10.1097/BPO.0000000000000693
- Loder RT. Demographics of traumatic amputations in children. Implications for prevention strategies. J Bone Joint Surg Am. 2004;86(5):923-928. doi:10.2106/00004623-200405000-00006
- NEISS – National Electronic Injury Surveillance System: Coding Manual. U.S. Consumer Product Safety Commission: Division of Hazard and Injury Data Systems. Published 2019. Accessed April 15, 2020. https://www.cpsc.gov/s3fs-public/2019_NEISS_Coding_Manual.pdf
- Bachier M, Feliz A. Epidemiology of lawnmower-related injuries in children: A 10-year review. Am J Surg. 2016;211(4):727-732. doi:10.1016/j.amjsurg.2015.11.025
- Vollman D, Smith GA. Epidemiology of lawn-mower-related injuries to children in the United States, 1990-2004. Pediatrics. 2006;118(2):e273-e278. doi:10.1542/peds.2006-0056
- Khansa I, Pearson GD, Bjorklund K, Fogolin A, Kirschner RE. Pediatric lawnmower injuries: a 25-year review. JPRAS Open. 2021;29:135-143. doi:10.1016/j.jpra.2021.05.001
- Lee TS, Luhmann JD, Luhmann SJ, Quayle KS. Pediatric Lawnmower Injuries. Pediatr Emerg Care. 2017;33(12):784-786. doi:10.1097/PEC.0000000000001109
- Garay M, Hennrikus WL, Hess J, Lehman EB, Armstrong DG. Lawnmowers versus children: the devastation continues. Clin Orthop Relat Res. 2017;475(4):950-956. doi:10.1007/s11999-016-5132-5
- Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187-196.
- Prieto JM, Van Gent JM, Calvo RY, et al. Pediatric extremity vascular trauma: it matters where it is treated. J Trauma Acute Care Surg. 2020;88(4):469-476. doi:10.1097/TA.0000000000002595
- Hottinger DG, Nasr I, Canner JK, Kattail D, Koka R, Schwengel D. Incidence, distribution, and cost of lawn-mower injuries in the United States, 2006-2013. Public Health Rep. 2018;133(5):570-577. doi:10.1177/0033354918785909
- CPSC. CPSC Fact Sheet: Riding Lawnmowers. Bethesda, MD: United States of America Consumer Product Safety Commission. Published 2007. Accessed September 2022. http://www.cpsc.gov//PageFiles/122050/588%20Riding%20Lawnmower%20Fact%20Sheet.pdf
- Troybilt. Support.troybilt.com. https://support.troybilt.com/s/article/182-1. Published 2022. Accessed June 13, 2022.
- Riding Mower Safety. Mtdproducts.com. https://www.mtdproducts.com/en_US/safety-riding-mowers/. Published 2022. Accessed June 13, 2022.