Nasal Soft Tissue Triangle Large Composite Graft Take With Postoperative Hyperbaric Oxygen Therapy: A Case Report
© 2023 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Auricular composite grafts hold great potential for reconstructing the nasal soft tissue triangle with desired aesthetic results because there is ample tissue available for sufficient nasal ala projection and the natural curvature of the helical rim matches that of the alar rim. The use of auricular composite grafts also results in positive functional outcomes because of the cartilaginous airway support provided to widen the external nasal valve. Composite graft survival is highly dependent on graft size, as larger sized grafts have a higher metabolic demand.
To improve graft viability and reliability, hyperbaric oxygen therapy can be employed to accommodate the increased metabolic demand seen with larger composite grafts.
Conclusions. This report presents the survival of a large skin and cartilage composite graft for nasal soft tissue triangle reconstruction in conjunction with hyperbaric oxygen therapy to improve graft viability.
Introduction
Successful nasal tip and soft tissue triangle reconstruction proves to be a challenging task due to the complexity of nasal anatomy and its substantial contribution to facial aesthetics. The goals of reconstruction are to restore form and function by reestablishing nasal ala projection, achieving sufficient skin and nasal lining coverage, and obviating airway obstruction.1 There are many different approaches available for nasal reconstruction, each with their own advantages and disadvantages.2 These methods include skin grafts, local flaps, composite grafts, or even alloplastic techniques.1-3 Skin grafts may be considered in patients with superficial defects or significant comorbidities that cannot tolerate more extensive reconstruction. However, the aesthetic outcomes are usually suboptimal due to color mismatch and lack of volume to alleviate contour defects.1 Bilobed flaps can be used for defects less than 1.5 cm, and paramedian forehead flaps can be employed for larger defects greater than 1.5 cm. While both these methods provide adequate skin coverage, the latter often requires multiple staged surgeries.1,2
Composite grafts composed of skin and cartilage provide ample support to restore nasal ala projection and nasal airflow. Harvesting skin and cartilage from the helical apex or root provides a framework with a natural curvature that will not only enhance the aesthetic outcome by mimicking the alar rim but results in minimal donor site morbidity and is completed in one stage.4 Composite grafts are particularly useful for full-thickness defects because the alar skin, cartilage, and nasal lining can be simultaneously replaced.5
Graft survival is highly dependent on graft size. Some studies report the survival of larger grafts between 1.5 and 2 cm,6-8 but a more widely accepted guideline is to use grafts between 1 and 1.5 cm.5 The high metabolic rate of these grafts may explain their high failure rate and critical dependency on size.1
Perioperative interventions can be employed to increase survivability of these grafts and make them a more reliable method for nasal soft tissue triangle reconstruction. Methods being studied to improve graft viability include administration of postoperative systemic corticosteroids, hypothermia to decrease metabolic demand, and hyperbaric oxygen therapy (HBOT). HBOT has been shown to improve tissue survival after ischemic insult and is proposed to enhance flap and graft survival.9,10 This report presents a novel case in which HBOT was used successfully to aid in the vascularization and survival of a larger skin and cartilage composite graft for nasal soft tissue triangle reconstruction.

Methods
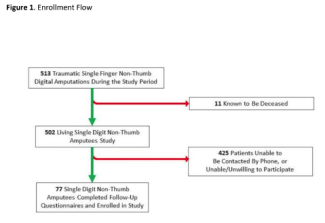
A 49-year-old woman sustained a traumatic dog bite resulting in injury to her right nasal soft tissue triangle and airway. Immediate reconstruction with a skin graft was performed at the time of injury, leaving the patient with right external nasal valve obstruction and soft tissue triangle asymmetries due to loss of approximately 8 mm of cartilaginous support (Figure 1). The patient was unsatisfied with the aesthetic outcome and decided to undergo revision surgery 1 year later.


The patient underwent a right soft triangle and alar reconstruction with composite cutaneous cartilaginous graft measuring 11 × 17 mm. The scar was excised as a triangular defect, and a 9-mm curved defect was noted from the superior portion of the columella medial crura onto the mid lateral crura (Figure 2A). The cartilaginous portion of the composite graft was 11 mm in length (Figure 3). The donor site was closed primarily with permanent sutures. The graft was inset into the nasal defect using parachuting sutures to the mucosa. The anterior graft skin was sutured to the mucosa with absorbable sutures. The cartilage was undermined, placed into its position, and closed anteriorly with permanent sutures. A soft splint was placed, and the incision was dressed in antibiotic ointment and sterile supportive dressings. Beginning the day after surgery, the patient underwent HBOT sessions, each lasting 90 minutes; the patient completed 7 treatment sessions.


Results
In the operating room following graft inset, moderate improvement in overall nasal shape and symmetry was observed (Figure 2B). On postoperative day 7 and after 7 HBOT sessions, composite graft survival was achieved (Figure 2C). Postoperative images were taken 8 weeks out from the date of surgery, and the patient was happy with the result (Figure 4). On follow-up 6.5 months after surgery, there was no evidence of graft contracture (Figure 5).
Discussion
Composite grafts maintain their shape, reducing the postoperative deformity and rate of airway restenosis, and often match the texture and color of the nasal skin.11 A disadvantageous aspect of auricular cartilage grafting is the associated unpredictable survivability. For this reason, this surgical method may be contraindicated in high-risk patients with a history of smoking, diabetes, vascular disease, or prior treatment with radiation therapy.5
A sufficiently large graft must be obtained from the auricular donor site to alleviate the functional and aesthetic concerns of the nasal defect. However, as the size of these grafts increases, the probability of graft failure increases due to the high metabolic demand of the grafted tissue.1 Thus, the size of the composite graft becomes critical as too little tissue volume may be attributed to failure to alleviate the defect whereas too much volume may result in necrosis of the grafted tissue.1
A potentially useful therapy in increasing the likelihood of survival of auricular composite grafts is HBOT. HBOT involves pressure elevation greater than atmospheric pressure while simultaneously delivering 100% oxygen to the patient. Patients will, on average, undergo 3 to 5 treatment sessions, each lasting 60 to 90 minutes.12 The patient in this report underwent 7 treatment sessions.
HBOT may increase the survivability of grafted tissue via hyperoxygenation through implication of Henry's Law. An increase in intrachamber oxygen precipitates an increase in arterial oxygen, which then leads to an increase in oxygen within patient plasma.11 This increase in plasma oxygen accommodates for the increased metabolic demand of the composite graft and thus may aid the survival of the transplanted tissue. The resultant hyperoxia leads to vasoconstriction, which reduces postoperative edema. Hyperoxygenation of tissue also promotes neovascularization and the generation of free radicals, which may act to eliminate bacteria.12 Thus, HBOT may allow for increased reliability for survival in auricular cartilage grafts to the nasal soft tissue triangle; however, its use is associated with significant cost and lack of accessibility.5 Additionally, while HBOT is relatively safe, it can result in such adverse effects as oxygen toxicity or barotrauma to the ears, sinuses, and lungs.13
In this case, the authors present the successful use of HBOT to aid in the survival of a skin and cartilage composite graft for nasal soft tissue triangle and airway reconstruction. The graft provided this patient with an improved aesthetic and functional outcome, and the patient experienced no side effects as a result of therapy. The authors of this paper hope to present HBOT as a useful adjunctive therapy in healing patients following auricular composite grafts to the nasal soft tissue triangle to improve outcomes.
Acknowledgments
Affiliations: 1Division of Plastic and Reconstructive Surgery, Tulane University School of Medicine, New Orleans, Louisiana
Correspondence: David A Jansen, MD; drjansen@jansenplasticsurgery.com
Ethics: Informed consent was obtained to publish the descriptions and photographs relating to this case.
Disclosures: Dr David Jansen is an advisor and an investor in Bongiovi Media and Medical, which has no affiliation to any hospital group. None of the remaining authors have anything to disclose.
References
1. Faris C, Vuyk HD. Reconstruction of nasal tip and columella. Facial Plast Surg Clin North Am. 2011;19(1):25-62. doi:10.1016/j.fsc.2010.10.012
2. Joseph AW, Truesdale C, Baker SR. Reconstruction of the nose. Facial Plast Surg Clin North Am. 2018;27(1):43-54. doi:10.1016/j.fsc.2018.08.006
3. Lee SH, Cho J, Lee JS. Long-term outcomes of secondary nasal tip plasty after degradation of a polycaprolactone (PCL) mesh. Aesthetic Plast Surg. 2022;46(5):2358-2365. doi:10.1007/s00266-022-02839-1
4. Chen C, Patel R, Chi J. Comprehensive algorithm for nasal ala reconstruction: utility of the auricular composite graft. Surgery J (N Y). 2018;4(2):e55-e61. doi:10.1055/s-0038-1639581
5. Harbison JM, Kriet JD, Humphrey CD. Improving outcomes for composite grafts in nasal reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2012;20(4):267-273. doi:10.1097/MOO.0b013e328355b1f2
6. Scheithauer MO, Rotter N, Lindemann J, Schulz M, Rettinger G, Veit JA. The auricle’s cavum conchae composite graft in nasal reconstruction. Am J Rhinol Allergy. 2013;27(2):e53-e57. doi:10.2500/ajra.2013.27.3883
7. Teltzrow T, Arens A, Schwipper V. One-stage reconstruction of nasal defects: evaluation of the use of modified auricular composite grafts. Facial Plast Surg. Jun 2011;27(3):243-248. doi:10.1055/s-0031-1275773
8. Haas AF, Glogau RG. A variation of composite grafting for reconstruction of full thickness nasal alar defects. Arch Dermatol (1960). 1994;130(8):978-980. doi:10.1001/archderm.1994.01690080042004
9. Buras J. Basic mechanisms of hyperbaric oxygen in the treatment of ischemia-reperfusion injury. Int Anesthesiol Clin. 2000;38(1):91-109. doi:10.1097/00004311200001000-00007
10. Kindwall EP, Gottlieb LJ, Larson DL. Hyperbaric oxygen therapy in plastic surgery: a review article. Plast Reconstr Surg. 1991;88(5):898-908. doi:10.1097/00006534199111000-00029
11. Immerman S, White WM, Constantinides M. Cartilage grafting in nasal reconstruction. Facial Plast Surg Clin North Am. 2011;19(1):175-182. doi:10.1016/j.fsc.2010.10.006
12. Bhutani S, Vishwanath G. Hyperbaric oxygen and wound healing. Indian J Plast Surg. 2012;45(2):316-324. doi:10.4103/0970-0358.101309
13. Liao S-C, Mao Y-C, Yang K-J, Wang K-C, Wu L-Y, Yang C-C. Targeting optimal time for hyperbaric oxygen therapy following carbon monoxide poisoning for prevention of delayed neuropsychiatric sequelae: a retrospective study. J Neurol Sci. 2018;396:187-192. doi:10.1016/j.jns.2018.11.025