A Case of Digital Pseudoaneurysm Following Sharp Injury to a Digit
Abstract
Background. A 74-year-old woman presented to the plastic surgery hand trauma clinic with painful, pulsatile swelling in her left index finger following a sharp incision injury to the digit. A diagnosis of digital artery pseudoaneurysm was made. Digital aneurysmal formations are uncommon, and in the upper limb such aneurysms are often secondary to trauma, including iatrogenic injuries. Surgery is usually indicated for symptom relief; if there are signs of compromised perfusion, either direct arterial repair or reconstruction with a vein graft may be required following excision of the aneurysmal sac.
Introduction
Both true and pseudoaneurysms in the upper limb are relatively uncommon and usually occur following trauma, but such aneurysms could also occur secondary to medical intervention, such as vascular access and anastomotic failure.1-3 The patient in this case report was a 74-year-old woman who was referred to the plastic surgery hand trauma clinic because of a painful, swollen left index finger. She sustained a sharp incision injury to the volar aspect of the finger from a kitchen knife 2 weeks before presentation. Following the injury, she developed a painful mass at the base of her index finger with associated numbness in the ulnar digital nerve distribution.
The patient’s medical history was significant for ovarian cancer, which was treated surgically. She had no drug allergies, and her medications included doxazosin, oramorph, and tramadol.
On examination, the patient had pulsatile swelling on the volar aspect of her left index finger adjacent to the scar from her injury. She had reduced sensation in the ulnar digital nerve distribution (subjective score of 3 out of 10). The swelling was nonmobile, pulsatile but not expansile. The overlying skin was erythematous and warm to touch. There was no bony tenderness. Her range of movement was limited by pain, with clinically intact flexor tendons. Distally, capillary refill time was within normal limits. Differential diagnoses included abscess or possible infected hematoma.
Methods
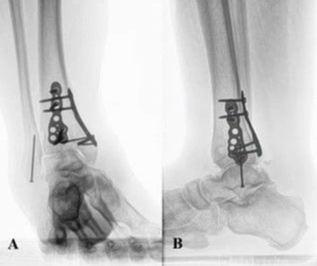
Plain radiographs were taken of the injured finger, which showed no evidence of any foreign bodies or bony injuries, although a soft tissue mass was seen in the lateral view (Figure 1). No other investigations were arranged as the patient was due to have same-day exploratory surgery of the finger, and a request for ultrasound or other imaging modalities could have caused delays.

The patient underwent surgery under regional nerve block for exploration of the swelling and to assess the digital nerves due to her altered sensation. An aneurysmal sac was found on the ulnar digital artery (Figures 2 through 5), which was ligated and excised and sent for histological analysis. No arterial reconstruction was required as distal perfusion was adequate. Both digital nerves were intact, and there was no evidence of any active infection. The wound was flushed with 0.9% normal saline and closed with nonabsorbable monofilament sutures. The patient remained in the hospital for 24 hours for prophylactic antibiotics, hand elevation, and hand physiotherapy before being discharged home.




Results
Histological analysis showed that the excised arterial segment contained an organized hematoma within the vessel lumen, suggestive of a pseudoaneurysm. The patient returned to the plastic surgery dressing clinic for follow-up evaluation, and satisfactory wound healing was noted at 2 weeks post operation. On assessment by a hand physiotherapist at this time, the patient’s range of movement was found to have returned to normal.
Discussion
Digital artery aneurysms are rare. There are few case reports published, and most cases reported are pseudoaneurysms, often caused by penetrating trauma.4 True aneurysms are more commonly caused by blunt trauma. It has been suggested that due to the small caliber of the digital vessels, much higher force is required to cause vessel distention and the vessels are more likely to thrombose following trauma.4
Patients usually present with a painful swelling of the finger following some form of trauma, with or without symptoms of arterial insufficiency (eg, cold intolerance or paresthesia).1 Physical examination should focus on the location of the swelling of the finger, its proximity to any nearby wounds, and whether it is a pulsatile or expansile mass. Finger movement and sensation should be assessed to check digital nerve and flexor tendon integrity. Some have advised performing an Allen test; however, this test is not typically used to assess digital vessels.
Investigations can include plain radiographs to rule out any bony injuries and radio-opaque foreign bodies. Other modalities include ultrasound, which is often the preferred imaging modality, but magnetic resonance angiography or computed tomography angiography can also be used.2
Surgery is the mainstay of treatment. Early treatment is recommended for symptom relief if there are signs of compromised distal perfusion and for prevention of complications, such as aneurysm rupture and thrombosis.2,4 Commonly, the affected segment of artery is ligated and excised. If distal perfusion is compromised, reconstruction is required, either by direct anastomosis of the two ends of the artery or, if this is not possible, by applying a vein graft to bridge the gap.
References
1. Rivera PA. and Dattilo JB. Pseudoaneurysm. StatPearls. Updated 9th March 2022. Accessed 2nd April 2022. https://www.ncbi.nlm.nih.gov/books/NBK542244/
2. Vinnicombe Z, Little M, Nicola A, Ibañez. A rare case of digital artery aneurysm. JPRAS Open. 2019; 20: 87 – 91. https://doi.org/10.1016/j.jpra.2019.03.002
3. Shutze RA, Liechty J, Shutze WP. Palmar artery aneurysm. Proc (Bayl Univ Med Cent). 2017; 30: 50 – 51. https://doi.org/10.1080/08998280.2017.11929524
4. Strauch B, Melone C, McClain SA, Lee BT. True aneurysms of the digital artery: case report. J Hang Surg. 2004; 29A: 54 – 58. https://doi.org/10.1016/j.jhsa.2003.09.012