Breast Paraffinoma: A Case Report of 20-Year-Old Mineral Oil Injection in a Male Patient
© 2023 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Mineral oil injection represents a dated practice of rapid and inexpensive breast augmentation. After a latency period, surrounding tissue becomes inflamed and fibrotic. Breast paraffinoma is well-documented in women; however, only 3 cases of such masses in male patients exist in the literature.
Methods. We present a case of paraffinoma in a 63-year-old man from Puerto Rico who, desiring breasts, serially injected mineral oil into each breast daily for 13 years. Conservative management was initially attempted due to cardiac comorbidities and insurance authorization issues. The patient ultimately developed erosive wounds and therefore underwent excision of the bilateral breast masses as an en bloc specimen weighing 2.17 kg.
Results. Pathology indicated sclerosing lipogranulomatosis (paraffinoma). The quality of the wounds remaining warranted negative pressure wound therapy with serial debridement. The patient went on to successful reconstruction with a reverse abdominoplasty preserving periumbilical and intercostal perforators.
Conclusions. Plastic surgeons must educate patients against using exogenous injected materials for augmentation of the breasts, penis, or buttocks. Although uncommon in the US, certain populations like body builders and foreign immigrants are at higher risk for current or prior injection practices. Reverse abdominoplasty is a viable reconstructive modality for the large resulting defect.
Introduction
A common practice of breast augmentation in the 1950s through the 1970s was the injection of various materials, such as paraffin wax, silicone wax, or even epoxy resin.1 These products have been commonly infiltrated into all parts of the body, including the genitalia, lips, and most popularly the breast in attempt to enhance physical appearance.2 Of these injections, mineral oil rose to popularity due to its rapid results with a similar palpability as normal breast tissue and low material cost.1,3 This practice, once prevalent worldwide, and with the largest case series based in Southeast Asia, Brunei, has been largely abandoned given the now evident long-term complications of such injections.3
After injection, patients undergo a latency period where the body slowly reacts to the foreign substance, culminating in destructive inflammation and fibrosis to the surrounding tissue after several years.3 The main complication is the formation of paraffinoma, which occur when straight chain hydrocarbons like mineral oil are injected, causing the body to react to the foreign substance with granuloma formation.4
Patients who seek these injections from unlicensed providers for quick and cheap results are typically unaware of the dangers of such injections.3 Often the clientele are body builders, who inject for muscular contouring, or patients from developing countries without access to more sophisticated and modern methods of augmentation.1-3 Breast paraffinoma is well documented in women; a systematic review published in 2022 found 172 cases, with only 3 cases of injected breast paraffinoma in male patients.3 Here we present a 63-year-old cis male who serially injected mineral oil into his chest, eventually requiring operative intervention to remove the mass 20 years later.


Case Presentation
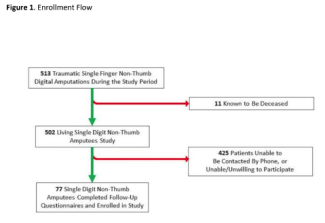
A 63-year-old man with a medical history of anxiety, coronary artery disease with stent placement, hypertension, hyperlipidemia, and myocardial infarction presented to our emergency department for assessment of chest pain. Upon questioning, the patient revealed that he had injected mineral oil at home into the 4 quadrants of each breast every day for 13 years. The patient was a cis male who identified as male but explained that he desired a more feminine appearance (Figures 1 and 2); he did not disclose any intention of transitioning to a transgender woman. He had immigrated from Puerto Rico to the US to seek treatment for these injections as he no longer desired the breast.
Due to his medical history, the patient needed cardiac and psychology clearance before surgical intervention. He reported that the increased hardening of his breast tissues was causing him pain at rest, inability to sleep, and significant pain with movement, leaving him unable to perform activities of daily living. He also had intermittent spontaneous bruising bilaterally. The patient developed depression due to the delay in surgery, and he became increasingly focused on removal.



Finally, 9 years after his initial presentation, clearances and insurance authorization were achieved, and surgical excision was scheduled. However, the patient presented to our emergency department prematurely due to cellulitis of his right breast with an overlying ulcerative lesion (Figure 3). The patient was admitted for intravenous antibiotics and underwent removal of his chest mass in the operating room. Operatively, we experienced difficulty achieving full excision in areas where the hardened scarred tissue was significantly adhered to the underlying pectoralis major or the overlying skin; there was concern for dermal involvement where excision would threaten perfusion. There were many small granulomatous nodules of scarred mineral oil injections. The bulk was excised en bloc; the entire specimen weighed 2.17 kg (Figure 5). En bloc removal was performed as the calcified masses were abutting each other and connected subcutaneously; this strategy ensured fewer granulomas were left behind. In effect, bilateral mastectomy was performed.
Pathology was consistent with sclerosing lipogranulomatosis (paraffinoma). Indocyanine green angiography (Stryker) was used to assess the overall perfusion of the skin flaps (Figure 4A). Some perfusion compromise was noted medially but appeared to improve; therefore, the remaining flaps were not completely excised during the operation. Negative pressure wound therapy was applied.
Four days later, the patient was taken back to the operating room for irrigation and debridement, replacement of the wound vacuum, and repeat fluorescence imaging to assess overall skin perfusion. Due to the quality of underlying tissue, impaired skin perfusion, and propensity for seroma, we determined that split-thickness skin grafts had a high probability of failure and therefore elected to again vacuum the defect and return for definitive reconstruction with reverse abdominoplasty and abdominal advancement flap, preserving periumbilical and intercostal perforators.

This reconstructive procedure was completed 6 days later (Figure 4B). His final surgery ultimately involved excision of the midline skin bridge as undermining caudally and cranially allowed to primary layered closure over drains. A postoperative compression wrap was placed. The patient was seen in clinic for drain and nylon suture removal, and his postoperative recovery was uneventful (Figure 6). The patient was happy with his cosmetic outcomes and did not request further chest contouring options.
Discussion
The injection of liquid paraffin, a mineral oil, into the breasts for augmentation is an outdated and dangerous practice. Although this method of cosmetic modeling is fraught with risk, it is still practiced commonly in Latin America, Asia, central Europe, and elsewhere by unqualified practitioners.5,6 Breast injections are most commonly seen among women and transgender women, with a wide age range reported in the literature from 26 to 69 years.3,7 The body responds with an inflammatory reaction that ultimately results in a paraffinoma, which is essentially a foreign body granuloma. Although some patients experience an acute response to the injections, the development of a paraffinoma may take years, as the breast parenchyma reacts to the mineral oil with chronic inflammation and fibrosis.3 Sclerosing lipogranuloma, as seen in our patient, is characterized by tissue injury causing endogenous lipid catabolism that leads to further subcutaneous inflammation.6 Giant cells, or histiocytes, also surround the cystic oil spaces created from the tissue destruction.8
The typical presentation of paraffinoma includes painless or painful breast lumps, skin discoloration or hyperpigmentation, nipple retraction, abscesses, and in severe cases, cancer and death due to an embolism.3 The development and severity of paraffinoma symptoms does correlate with the frequency and volume of injections.6 For example, larger and more frequent injections can escalate the timing of drastic inflammation to present around 3 to 6 months rather than years, as described in the case report by El Muayed et al. The authors had treated a male patient who injected 2.9 kg of mineral oil into their breasts, which ultimately led to the patient’s death 11 months later.4 Comparatively, our patient consistently injected mineral oil over the course of over a decade but did not exhibit symptoms to warrant medical attention for years. Our patient also progressed with chronic kidney disease, which is among the rarer incidents of paraffinomas.3
There is scant literature regarding the psychological impact of this practice. However, data on penile, breast, and buttock injections demonstrate self-esteem as driving motivation for these procedures.3,5,9 It is unsurprising, therefore, that our patient, a male who was not transgender, developed depression concerning his symptoms and appearance of his chest in the setting of escalating pain and deformity. Treatments of paraffinomas include mastectomy, which our patient had to remove the granulomatous tissue, excision, and incision and drainage.3 Mastectomy represents the only salvage when the paraffin is diffused throughout the tissue and has led to skin necrosis.3 Free flaps and skin grafts have even been used when extensive amounts of tissue have been removed.3 Our method of achieving primary closure via reverse abdominoplasty has been previously described in women undergoing bilateral mastectomies.10 This allows large anterior soft tissue defects to be covered and furthermore allowed for placement of bilateral chest drains, which was deemed prudent given seromatous fluid expressed bilaterally after wound vacuum removal.10
Conclusions
It is crucial for plastic surgeons to educate patients against using mineral oils, paraffins, and other oils for augmentation of the breasts, penis, or buttocks. These injections can be severely detrimental to the local tissue, with long-term effects being harmful to the psyche. Although not common practice in the US, injection of these substances should be deterred by plastic surgeons as they can recognize certain populations like body builders and foreign immigrants as higher risk for current or prior injection practices.8 When skin excision is required, primary closure may be achieved through reverse abdominoplasty, even in the setting of a large soft tissue defect.
Acknowledgments
Affiliations: 1USF Health Morsani College of Medicine, Tampa, Florida; 2USF Department of Plastic Surgery, Tampa, Florida
Correspondence: Bilal Koussayer, BS; bkoussayer@usf.edu
Ethics: Informed consent was obtained from all individual participants included in the study.
Disclosures: No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript.
References
1. Ho WS, Chan AC, Law BK. Management of paraffinoma of the breast: 10 years’ experience. Br J Plast Surg. 2001;54(3):232-234. doi:10.1054/bjps.2000.3533
2. Sarıca Ö, Kayhan A, Demirkürek HC, İğdem AA. Subcutaneous oleomas following sunflower oil injection: a novel case and review of literature. J Breast Health. 2016;12(3):141-144. doi:10.5152/tjbh.2016.3115
3. Yen Kok KY, Tripathi S, Telisinghe P. Breast paraffinoma: an obsolete but still important condition - experience with 60 cases and the literature review. Asian J Surg. 2023;46(1):321-327. doi:https://doi.org/10.1016/j.asjsur.2022.04.002
4. El Muayed M, Costas AA, Pick AJ. 1,25-Dihydroxyvitamin D-mediated hypercalcemia in oleogranulomatous mastitis (paraffinoma), ameliorated by glucocorticoid administration. Endocr Pract. 2010;16(1):102-106. doi:10.4158/EP09008.CRR
5. Martínez-Villarreal AA, Asz-Sigall D, Gutiérrez-Mendoza D, et al. A case series and a review of the literature on foreign modelling agent reaction: an emerging problem. Int Wound J. 2017;14(3):546-554. doi:10.1111/iwj.12643
6. Soebhali B, Felicio J, Oliveira P, Martins FE. Sclerosing lipogranuloma of the penis: a narrative review of complications and treatment. Transl Androl Urol. 2021;10(6):2705-2714. doi:10.21037/tau-21-228
7. Ahmed U, Freeman A, Kirkham A, Ralph DJ, Minhas S, Muneer A. Self injection of foreign materials into the penis. Ann R Coll Surg Engl. 2017;99(2):e78-e82. doi:10.1308/rcsann.2016.0346
8. Bjurlin MA, Carlsen J, Grevious M, et al. Mineral oil-induced sclerosing lipogranuloma of the penis. J Clin Aesthet Dermatol. 2010;3(9):41-44.
9. Downey AP, Osman NI, Mangera A, Inman RD, Reid S V, Chapple CR. Penile Paraffinoma. Eur Urol Focus. 2019;5(5):894-898. doi:10.1016/j.euf.2018.06.013
10. Tiong WHC, Basiron NH. Reverse abdominoplasty flap in reconstruction of post-bilateral mastectomies anterior chest wall defect. Case Rep Med. 2014;2014:942078. doi:10.1155/2014/942078