Nasolabial Flap for Nasal Reconstruction and Beyond
© 2023 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Questions
1. When and how are nasolabial flaps typically performed?
2. What are the various types of nasolabial flaps?
3. When should you employ one-stage vs two-stage procedures?
4. What are some other uses of nasolabial flaps?
Case Presentation
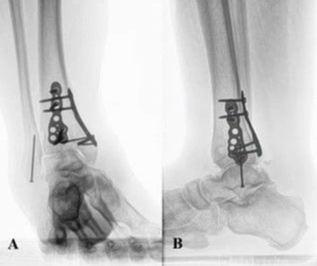
A 77-year-old female presented with a large circular Mohs defect on the right nasal side wall that resulted from the excision of squamous cell carcinoma (Figure 1A). The defect measured 2 x 1.9 cm. The oncology workup was negative for metastatic disease. She was taken to the operating room and underwent two-stage reconstruction using the right nasolabial flap (NLF) pedicle flap. The first stage consisted of elevating the flap and then suturing it over the defect (Figure 1B). The second stage took place 3 weeks later and consisted of the division and inset of the flap. The patient was offered a debulking procedure 3 weeks later, but she declined and was happy with the outcome (Figure 1C).

Q1. When and how are nasolabial flaps typically performed?
NLFs are cheek flaps harvested from an area of prominent cheek fat lateral to the nasolabial crease referred to as the nasolabial fold. After soft tissue injury due to trauma or excision, NLF is ideal for facial reconstruction of the nose and cheek. It provides proximity to the area, is a soft tissue color and texture match, and hides a scar in the nasolabial crease.1 Prior to excising the flap, the area of the defect should be prepared by reverticalizing the edges, a reverse Gillie test should be performed, and a template should be created to ensure that the flap can adequately cover the defect and can appropriately rotate into position.1 The flap is elevated by making the inferior incision along the nasolabial fold, and the superior incision is marked based on the template created to ensure adequate tissue is harvested.1 Typically the flap is based superiorly due to the ability to harvest more tissue; however, a flap with an inferior base may also be used, particularly in cases of upper or lower lip defects and reconstruction of the floor of the nose or columella.2 Once lifted the flap is carefully thinned under the dermis to preserve the subdermal plexus.3 The NLF can then be maneuvered and inset into the area of the excised defect and sutured under a slight degree of tension to reduce the risk of late pivot-cushioning deformity.1,3 The donor site is subsequently closed primarily and the flap is dressed.1 Division can then be performed, if necessary, within 3 weeks of the initial procedure.1
Q2. What are the various types of nasolabial flaps?
Advancement (V-Y) NLFs move in the direction of their long axis to reach a superior defect. This technique is mostly used for infraorbital, medial canthus, and lateral nasal reconstruction and is well suited for reconstructing the area where the lower or middle third of the nose meets the cheek.2
Rotation NLFs are created with a pivot point at the base and the lateral limit of the defect coinciding with the medial margin of the flap. This one-stage flap is indicated for reconstruction of the upper lip lateral segment or a defect on the nasal side wall, preferably at 30 degrees to 60 degrees of flap rotation.2
Transposition NLF is a variant of the rotation type where the NLF is lifted and rotated to reach an immediately adjacent defect in a single stage. This technique is indicated for oral cavity reconstruction and is often used for reconstruction of complex alar and nasal tip defects. The flap can also be folded upon itself to restore nasal lining, often in combination with other flaps.2,4
Interpolation NLFs are like transposition flaps except the flap is lifted over an area of normal skin to reach the defect. This technique is used when there is not enough tissue or mobility in nearby skin to cover a defect with primary closure or an adjacent flap. This requires two stages as the bridge must be disconnected approximately 3 weeks later once vascular supply is established between the wound and the flap. These are suitable for nasal tip or columella reconstruction.2
Propeller-type NLFs are island flaps, which involve skin excision from pedicles, that are axially rotated to reach the defects.2 An advantage of this technique is that it allows for mobility; however, it requires perforator dissection that can be time-consuming.2 This is often preferred for reconstructing perinasal defects.2
Q3. When should you employ one-stage vs two-stage procedures?
The size and complexity of the nasal defect are important factors that influence a plastic surgeon's decision to perform a one-stage or two-stage surgery using an NLF for nasal reconstruction. In general, one-stage surgery may be preferred for smaller defects that are relatively straightforward to repair. For example, if the defect is adjacent to the flap and is in the alignment axis of the flap, then a one-stage surgery with rotational NLF is often performed.5 Advancement (V-Y) NLFs are also performed in a single stage and have been used for reconstruction of nasolabial fold and nasal sidewall defects following excision of basal cell carcinoma with excellent results.6 In contrast, two-stage surgery may be preferred for larger or more complex defects, not adjacent to the flap, that require more extensive reconstruction. For example, a two-stage surgery using an NLF may be necessary to repair a large defect on the front of the nose that involves both the skin and the underlying cartilage.5 In this case, the surgeon would first raise the NLF and leave it in place with a stent to maintain its blood supply. The stent would then be removed, and the flap would then be transferred to the defect in a second procedure 2 to 3 weeks later. It is important to note that the choice between a one-stage or two-stage surgical approach will depend on a variety of factors, including the size and complexity of the defect, the location of the defect relative to the flap, and the overall health of the patient. In general, one-stage surgery may be preferred for smaller, more straightforward defects, while two-stage surgery may be preferred for larger or more complex defects.7
Q4. What are some other uses of nasolabial flaps?
NLFs are ideal for reconstruction of intraoral defects in the floor of the mouth, tongue, cheek, commissures, nose tip, nasal ala, and lower eyelids because of their versatility and good vascular supply.8 The subcutaneous pedicled NLF is ideal for small to moderate size intraoral defects. This technique involves passing the flap through a transbuccal tunnel to reach the oral cavity.4 Whenever NLF is used in intraoral defects, the risks of orocutaneous fistula and iatrogenic dermoid (inclusion) cysts should be considered.4 The risk of dermoid cyst formation can be reduced by de-epithelializing the skin near the base of the flap.4 NLFs can also be used for columella defects by using bilateral nasolabial fold flaps. The length of the flap provides enough tissue to reconstruct this challenging area. Recent case reports suggest that 2 transnasal NLFs provide aesthetic and functional results.9 In the lower lip, one-stage inferior NLFs allow functional and aesthetic outcomes with normal movements and sensation, adequate mouth opening and oral competence, and good color and texture match with adjacent tissues. NLFs can be used for large full-thickness lip defects in patients where microstomia cannot be tolerated and for commissural defects with buccal mucosal lesions, which need coverage after excision. However, oral incompetence occurs in commissural defects that may improve over time.10 Use of NLF for the upper lip is also an option with the rotational flap because it allows camouflaging of the rotation arc in the nasolabial fold.4 NLFs can additionally be used when reconstruction involves the nasal lining by turning over an interpolation flap.6 By pairing this with a cutaneous flap, such as a paramedian forehead flap as described by Lane et al, full-thickness nasal defects can be reconstructed in a way that is both functional and aesthetically pleasing.
Acknowledgments
Affiliations: 1University of Toledo, College of Medicine and Life Sciences, Toledo, Ohio; 2University of Toledo, College of Medicine and Life Sciences, Division of Plastic and Reconstructive Surgery, Toledo, Ohio; 3Jobst Vascular Institute: ProMedica Health Network, Wound Care Program, Toledo, Ohio
Correspondence: Richard Simman, MD, FACS, FACCWS; Richard.simmanmd@promedica.org
Disclosures: The authors disclose no relevant financial or nonfinancial interests.
References
1. Goh CS, Perrett JG, Wong M, Tan BK. Delayed bipedicled nasolabial flap in facial reconstruction. Arch Plast Surg. 2018;45(3):253-258. doi:10.5999/aps.2017.00878
2. Bayer J, Schwarzmannová K, Dušková M, Novotná K, Kníže J, Sukop A. The nasolabial flap: the most versatile method in facial reconstruction. nasolabiální lalok: nejuniverzálnější metoda pro rekonstrukci v obličeji. Acta Chir Plast. 2018;59(3-4):135-141.
3. Monarca C, Rizzo MI, Palmieri A, Chiummariello S, Fino P, Scuderi N. Comparative analysis between nasolabial and island pedicle flaps in the ala nose reconstruction. Prospective study [published correction appears in In Vivo. 2012 Jul-Aug;26(4):741-2]. In Vivo. 2012;26(1):93-98.
4. Rahpeyma A, Khajehahmadi S. The place of nasolabial flap in orofacial reconstruction: A review. Ann Med Surg (Lond). 2016;12:79-87. Published 2016 Nov 23. doi:10.1016/j.amsu.2016.11.008
5. Prakash S, Panda R, Kumar V, et al. Nasolabial perforator flap for one-stage reconstruction of nasal defects. J Cutan Aesthet Surg. 2017;10(1):22-27. doi:10.4103/0974-2077.204576
6. Lane JE, Bob Hsia LL, Merritt BG. Reconstruction of large transmural nasal defects with a nasolabial turnover interpolation flap. Dermatol Surg. 2020;46(7):899-903. doi:10.1097/DSS.0000000000002151
7. Weathers WM, Koshy JC, Wolfswinkel EM, Thornton JF. Overview of nasal soft tissue reconstruction: keeping it simple. Semin Plast Surg. 2013;27(2):83-89. doi:10.1055/s-0033-1351226
8. Singh S, Singh RK, Pandey M. Nasolabial flap reconstruction in oral cancer. World J Surg Oncol. 2012;10:227. Published 2012 Oct 30. doi:10.1186/1477-7819-10-227
9. Krogerus C, Demant M, Lindskow T, Hesselfeldt J. Reconstruction of columella and nasal vestibuli by bilateral nasolabial flaps - A case report. Int J Surg Case Rep. 2022;90:106694. doi:10.1016/j.ijscr.2021.106694
10. Shaikh AI, Khan AH, Tated S, Khubchandani N. Functional and aesthetic outcome of different methods of reconstruction of full thickness lip defects. GMS Interdiscip Plast Reconstr Surg DGPW. 2022;11:Doc02. Published 2022 Mar 8. doi:10.3205/iprs000163