Ohio Diversion Plan Keeps Emergency Patients Moving
Emergency departments in Central Ohio are at maximum capacity, and a third hospital in the region has just gone on EMS diversion. The Columbus Division of Fire Alarm Office (FAO), which dispatches fire-based 9-1-1 EMS agencies, receives an automated phone call from the Central Ohio Trauma System’s (COTS’) web-based Real Time Activity Status (RTAS) mechanism and enacts the Emergency Patient Transport Plan (EPTP).
This assigns a new dispatcher as the EPTP transportation manager and notifies all hospitals in the area. Franklin County EMS agencies contact this manager for any stable patient transport, and, like an air-traffic controller, the manager starts directing transporting ambulances to hospitals and freestanding EDs (FSEDs) based on location and a predetermined capacity ratio. Unstable patients still go to the closest most appropriate hospital or FSED, and patients needing specialty care or who were recently discharged go to their established treatment facility.
Essentially, in Central Ohio, if three hospitals go on diversion, nobody is on diversion.
A Controversial Topic
Ambulance diversion is a controversial topic. How do we manage emergency patients when EDs are overcrowded and have no room for ambulance arrivals? Some cities and states have banned diversion. The Central Ohio Trauma System created the Emergency Patient Transport Plan. Some call it the “diversion plan,” but actually it’s an antidiversion plan. Twenty-one years after its inception, it has been through some iterations, but it is still an important part of access to emergency care in Central Ohio.
COTS, established in 1997, is a group of physicians, healthcare professionals, and other experts working together to improve patient outcomes related to trauma, emergency services, and disaster preparedness. The EPTP was one of its first large-scale collaborative projects and has been in place in Central Ohio since early 2000.
At that time the region looked like much of the nation: EDs suffered overcrowding, and daily ambulance diversions were common. From January–March 1999, 11 Columbus-based hospitals recorded a total of 900 total diversion hours.1 In Cuyahoga County there were an estimated 38,000 hours of ambulance diversion in 2000 and a fourfold increase in ambulance diversion from 1998–2000.2 EMS providers complained they often called two or three hospitals before finding one to accept a patient—sometimes patients who were critical. Said David Keseg, MD, then medical director for the Columbus Division of Fire, “We tell our EMS to call hospitals when they are en route, but there have been instances when a squad has been on the ramp to an emergency department and been diverted.”1
Driving from hospital to hospital kept units out of service for extended periods throughout the day. Leaders estimated diversion cost each unit nine hours of service daily. From the hospital perspective it became more and more difficult to accept ambulances as ED waiting rooms continued to fill. Many providers thought that was unsafe and diversion was their only option. Once one hospital went on diversion, a domino effect often occurred, causing crowding and subsequent ambulance diversions at nearby facilities.
In January 1999 the American College of Emergency Physicians released a policy stating that “EMS systems must develop mechanisms to address patient diversions.”3 COTS answered that call with a Diversion Task Force composed of EMS and hospital personnel. They met throughout the year and ultimately produced the EPTP. It was signed by all Franklin County hospital CEOs and EMS directors, as well as the chief of Columbus Fire in December 1999. The major attributes of the EPTP are described below.4
Commitment—All ED medical directors, nurse managers, and hospital executives verbalized a commitment to minimize ED diversion of EMS patients. EMS verbalized a commitment to work with the hospitals to seek an amenable solution.
Critical or unstable patients—Regardless of a hospital’s current diversion status, critical or unstable patients may be brought to that hospital’s ED at the discretion of EMS providers.
Selective diversion—No ED may selectively divert an EMS patient. EDs will either accept all EMS patients, or they are on divert status for all EMS patients.
Real-Time Activity Status (RTAS)/ED status activity webpage—This password-protected webpage allows hospitals to post their current ED activity status with the intention of facilitating communication. The page is to be updated minimally every six hours, or more based on significant changes in activity.
Simultaneous hospital diversion—When a predetermined number of hospitals are in EMS diversion status simultaneously, the EPTP is officially initiated. The Columbus FAO begins a methodical allocation of EMS patients to all adult Franklin County hospitals. Hospitals receive a fraction of EMS runs based on their ED bed capacity and overall inpatient bed availability. These numbers were preassigned and agreed on by stakeholders. When the EPTP is initiated, no hospital may divert or refuse an EMS patient.
History and Changes
The EPTP was activated for the first time in March 2000. It was in effect for 24 hours, during which the Columbus FAO assigned 147 transports. Both EMS and hospitals provided positive feedback. Hospitals liked the plan because they felt they had enough of a break between squads to decompress, and EMS reported good cooperation between hospital personnel and medics during what would normally be strained times.
With each activation the plan was debriefed, and in 2001 some areas of potential improvement were discovered. One resulting revision was that during the EPTP activation, patients would only be transported to one of the three nearest hospitals to prevent unnecessarily long transport times. It also established that the need for the EPTP would be re-evaluated by all hospitals every 12 hours at specific times to help facilitate timelier deactivations.
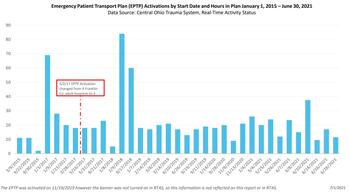
In 2003 the plan was changed to allow activation after four hospitals declared diversion status, but this was changed back to three hospitals in 2017. The thought is that activating the plan sooner allows for earlier decompression of regional hospitals and a quicker return to normal operations.
We added freestanding EDs to the plan in 2018 and created a subcommittee to review Columbus FAO and hospital diversion data at least quarterly. In 2019 private EMS agencies were invited to join the EPTP, and we added postactivation conference calls to review the data.
Right Patient, Facility, Time
Throughout all its adaptations the EPTP’s key tenets have not changed. No unstable patient will ever be diverted away from the nearest and most appropriate facility. Financial ability is never a factor in determining patient destination, and medical homes and continuity of care are recognized. Hospitals can declare diversion status as they see fit, but when three hospitals are simultaneously on EMS diversion, the EPTP is activated, and EMS ambulances are then distributed per the predetermined ratio. No ambulances can be refused.
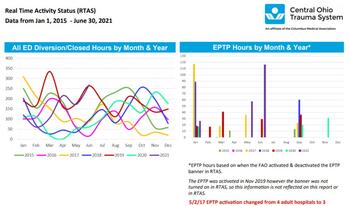
Since 2015 we have collected and analyzed data from the COTS RTAS system. Over the years we have noted multifactorial fluctuations in EPTP activation (Figures 1, 2). Certain years have had more active flu seasons, and when school starts in September, there is often a surge in diversions and EPTP activations. The common thread throughout these stresses is that we have an active plan that manages patient flow and access to care throughout the region. The EPTP and RTAS are under continuous performance improvement scrutiny to ensure the right patient gets to the right facility in the right amount of time. The next steps include expansion of the EPTP to EMS in counties contiguous to Franklin County and the advancement of automated processes between RTAS and the Columbus FAO and participating EMS, hospitals, and FSEDs.
The EPTP requires a collaborative effort between healthcare systems and numerous EMS agencies. It has remained an integral aspect of our EMS system in Central Ohio by focusing on the patient.
References
1. Somerson M. Emergency the ER’s Full. Columbus Dispatch, 1999 June 17.
2. Solov D, McEnery R. Will your ER be there for you? Cleveland Plain Dealer, 2001 Apr 1.
3. American College of Emergency Physicians. Policy statement, Ambulance Diversion, January 1999.
4. Central Ohio Trauma System. Emergency Patient Transport Plan Emergency Department Educational Flyer, March 2001.
Janine E. Curcio, DO, is a graduate of the OhioHealth Doctors Hospital EMS Fellowship. Reach her at janine.curcio@ohiohealth.com.
Natalie Ferretti, MD, is a graduate of the OhioHealth Doctors Hospital EMS Fellowship. Reach her at ferrettin@usacs.com.