MIH for Patients With Dementia: the CHAMP Program
In recent years mobile integrated healthcare (MIH) has reenvisioned EMS’s ability to handle community needs, including high healthcare utilizers. One such pilot is the Christian Hospital Community Health Access Program (CHAP) in Saint Louis, Mo., which seeks to reduce 9-1-1 use, emergency department visits, and hospital admissions for patients who frequently utilize the healthcare system.
As part of its mission to integrate healthcare and social support resources, CHAP partnered with Memory Care Home Solutions (MCHS), a program that provides education and training for lay caregivers of persons living with dementia (PLWD) to help extend and improve quality of life, particularly in the home setting.
Together CHAP and MCHS created the Community Health Access and Memory Project (CHAMP), an effort to provide in-home medical surveillance and caregiver training to 30 PLWD-caregiver dyads.
The Community Need
Approximately 10% of the U.S. geriatric population have dementia.1,2 Dementia is often undiagnosed and prevalent among those with congestive heart failure (CHF), pneumonia, myocardial infarction (MI), and chronic obstructive pulmonary disease (COPD). Due to impaired executive functioning, patients are often unable to follow disease management instructions and adhere to medication regimens.
Research shows caregiver education and training yield positive outcomes for both caregivers and PLWDs.3 Targeting caregiver burden and self-care by implementing specific skills training to create a problem-solving approach to managing the disease can be useful for both the caregiver and PLWD. Combining caregiver training with approaches to modify the home environment has been shown to lessen caregiver burden and delay nursing home placement.
The Program
Possible PLWD-caregiver dyads were identified by any approved referral source aware of this program. These sources included hospital social workers, hospital case managers, CHAP staff, MCHS staff, and area skilled nursing facilities.
Once a patient was referred, CHAP performed an initial home assessment to ensure they would qualify for the program. The initial assessment included a full medical assessment, medication reconciliation, medication inventory, fall risk survey, and needs assessment. The initial assessment also included the Short Blessed Test (SBT), a dementia screening tool, performed by the CHAP advanced practice paramedic (APP). Additionally, both the PLWD and caregiver were educated about the CHAMP program and asked for consent to be enrolled.
Once patients were enrolled, MCHS staff, the CHAP APP, and the CHAP medical director developed a care plan to best meet their needs. MCHS and CHAP staff visited the PLWD at predetermined intervals as outlined in the care plan and agreed upon by the team.
MCHS staff completed initial caregiver training consultation (CTC), which consisted of dementia education, discussion and problem-solving of current symptoms and challenges, and connection to other community resources related to dementia, caregiving, and aging.
All clients were offered up to four additional sessions with MCHS occupational therapists to learn strategies for adapting the caregiver’s approach to routine and challenging dementia behaviors, as well as environmental modifications. Clients received follow-up phone calls at regular intervals, including three, six, and 12 months after the initial CTC date.
Our Results
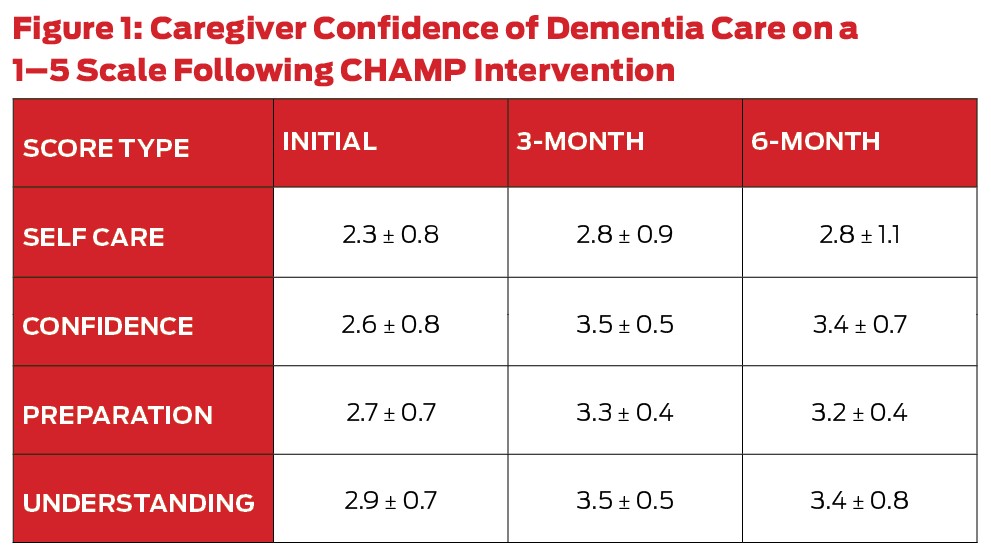
We worked with dyads to improve quality of life at home for the PLWD and caregiver alike. This included safety assessments, caregiver training, and education on dementia and behavioral care strategies, plus referrals to community resources. Following the intervention, caregivers’ confidence, understanding of dementia, and preparedness for the future trended toward improvement. These results were sustained over six months.
Despite a small sample size, we were able to demonstrate no increase in hospitalizations or 9-1-1 calls and a decrease in the number of ED visits from three to two a month. This means more time spent at home for patients and fewer lost workdays for caregivers.
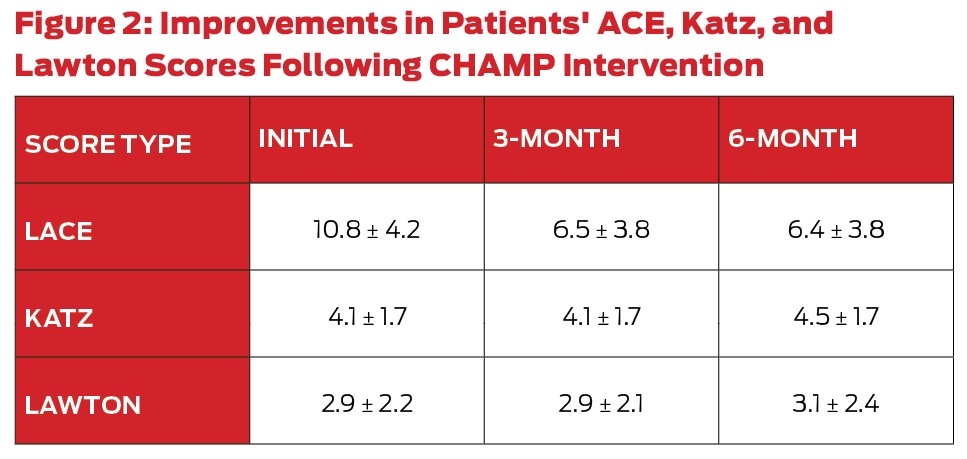
Patients maintained function for activities of daily living (ADLs) and instrumental activities of daily living (IADLs) measured by the Katz and Lawton scales. Specifically, the Katz Index of Independence in ADL measures independence/dependence in such activities, including bathing, dressing, toileting, transferring, continence, and feeding. Scores range from 0–6, with a higher score indicating more independence.
The Lawton Scale measures ability in instrumental activities of daily living such as the ability to use the telephone, shopping, food preparation, housekeeping, laundry, ability to access transportation, responsibility for medications, and ability to handle finances. The score ranges from 0–8, with a higher score indicating more independence.
Notably, patients experienced a significant decrease in risk for hospital readmission as measured by the LACE readmission risk index. Specifically, the LACE index measures the risk of hospital readmission based on recent length of stay in the hospital; whether the stay was an acute admission; patient comorbidities; and frequency of emergency room visits in the prior three months. The score range is from 0–19, with a higher score indicating a higher risk of readmission.
MCHS adapted the LACE index to examine emergency room visits within a three-month period, rather than a six-month period as it aligns with their follow-up intervals.
Clinicians found many patients had very severe dementia at the time of referral to our program. Using the dementia behavior tool, we noted patients who are referred to our program have typically exhibited multiple dementia problem behaviors within the last month (average 8.8 on a 0–24 scale), and these behaviors are challenging and upsetting to their caregivers (average 15.3 on a 0–96 scale). The severity of disease was emphasized by the fact that nearly one-third of PLWDs were placed in long-term care or passed away during the intervention.
What does this mean for the future?
The geriatric population is the fastest growing segment in the U.S., with estimates that a fifth of the total United States population will be 65 or older by the year 2025. A recent study notes this population places a heavy burden on our EMS systems and that the geriatric population consisted of a third of all EMS patients transported.
This innovative collaboration between EMS and a community-based organization may be a way to improve the health of people who suffer from dementia and their caregivers. Screening performed by EMS may allow for earlier identification and coordination with healthcare systems. With earlier screening and referrals, we hope we can make even bigger impacts on the lives of this population.
References
1. Graham JE, Rockwood K, Beattie BL, et al. Prevalence and severity of cognitive impairment with and without dementia in an elderly population. Lancet, 1997 Jun 21; 349(9,068): 1,793–6.
2. Plassman BL, Langa KM, Fisher GG, et al. Prevalence of Dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology, 2007 Nov; 29(1–2): 125–32.
3. Gitlin LN, Winter L, Dennis MP, Hodgson N, Hauck WW. A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers: the COPE randomized trial. JAMA, 2010 Sep 1; 304(9): 983–91.
Melissa Kroll, MD, is EMS clinical instructor in the Division of Emergency Medicine at Washington University in St. Louis.
Amy Sobrino, MSW, LCSW, is program services coordinator at Memory Care Home Solutions and founder and president of Effingham Area Alzheimer's Awareness.
Hawnwan Philip Moy, MD, is assistant medical director for the St. Louis City Fire Department and emergency medicine clinical instructor and core faculty in the EMS Section of the Division of Emergency Medicine at Washington University in St. Louis. He completed his emergency medicine residency at Barnes Jewish Hospital/Washington University in St. Louis and his EMS fellowship at the University of North Carolina in Chapel Hill.