Wound Care Technologies: Emerging Evidence for Appropriate Use in Long-Term Care
Introduction
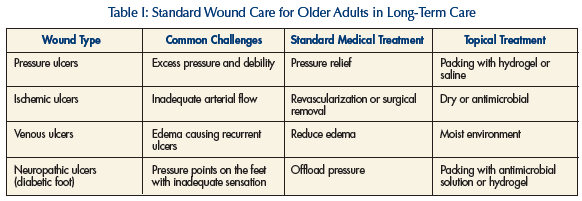
Wound management in long-term care (LTC) can present many challenges to the ultimate goal of complete wound healing. Healthcare providers frequently encounter and manage pressure ulcers, ischemic ulcers, venous ulcers, and diabetic foot (neuropathic) ulcers. All residents should be assessed for their risk of developing an ulcer. If a resident is at high risk, staff should implement aggressive maneuvers like nutritional support or pressure reduction to prevent an ulcer from occurring. If an ulcer develops, the primary goal is to completely heal the ulcer as quickly as possible and at a reasonable cost. Providers should identify ulcer type as a pressure, ischemic, venous, or neuropathic ulcer while understanding it can be mixed and have two or more components.1 To achieve this goal, providers should ensure good fundamental care (Table I),2 adequate nutrition, good blood supply, edema control, and excellent topical wound care. Good topical wound care enhances wound healing with a hydrating environment while minimizing necrotic tissue.3
To further achieve these goals and objectives, providers and LTC facilities often use a multidisciplinary approach. This multidisciplinary approach includes help from nursing, physical therapy, dietary, pharmacy, and occupational therapy, among many others who provide wound care support. Wound care technology can be utilized in addition to standard wound care to achieve these goals by all providers.
Wound care technology continues to expand with the development of devices and dressings to assist with wound healing. Often, this technology is used to obtain healing in a nonhealing ulcer, to hasten healing of an acute or chronic ulcer, or to reduce the cost of caring for the ulcer by reducing nursing burden. The provider should possess a reasonable expectation of what each technology provides and how it will help with resident care.
Many of the proposed technologies for wound care fail to evaluate all of the major healing outcomes and are very rarely studied in LTC. This review will evaluate the available evidence for commonly used technologies of negative pressure wound therapy, hyperbaric oxygen therapy, pressure reduction mattresses, silver-based dressings, and ultrasonic mist. Other technologies such as growth factors,4 topical electrical stimulation,5 and maggot therapy,6 among others, are available but will not be addressed in this article.
Search Methods
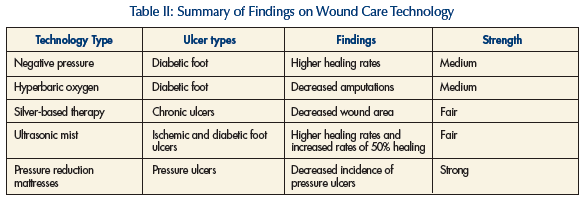
This review used different search methods to arrive at the evidence for each individual technology. Searches were made with the broad terms of wound care and the individual therapies of interest in this review (negative pressure therapy, hyperbaric oxygen therapy, silver- based therapy, and pressure mattresses), acknowledging that previous systematic reviews have been published that address, in part, these topics.7-10 Randomized controlled trials (RCTs) or meta-analyses of RCTs for each therapy published in the time period from 1960 to June 2007 included in MEDLINE or PubMed were eligible for this review. The primary measures of interest were complete wound healing, the time to wound healing, and cost-effectiveness. A summary of findings for wound care technology appears in Table II.
Negative Pressure Therapy (Vacuum Devices)
Negative pressure wound therapy (NPWT) is a common technology that is available in the nursing home. It is a closed system that utilizes negative pressure to drain wound fluid away from, and nutrients into, a wound. Medical-grade foam is placed over the wound, which is subsequently covered with a thin transparent biofilm, creating an airtight seal. Providers often utilize NPWT therapy for diabetic foot ulcers or pressure ulcers. Proponents of this therapy believe that wound healing is accelerated by drawing fluid out of the interstitial space or decreasing bacterial load in the wound.11 The exact mechanism of effect is not known.
There were few RCTs of NPWT therapy until 2005, with three RCTs in 2006 and 2007. Two different systematic reviews by both the Cochrane collaborative7 and the Agency for Healthcare Research and Quality (AHRQ)12 revealed only a small number of randomized prospective trials prior to 2005. The AHRQ review included six RCTs13-18 with 148 total subjects, 54 of whom came from a single trial.13 The overall strength of the evidence was considered to be fair, with only one intention-to-treat trial.12 Both systematic reviews judged the evidence from RCTs to be inconclusive relative to the benefit of NPWT for chronic wound healing.12
The strongest and most robust science involved a RCT in 2005 that was published after both systematic reviews.19 One hundred sixty-two patients were randomized to receive standard wound care (n = 85) versus NPWT (n = 77) in 18 outpatient wound care centers. This was an intention-to-treat analysis in subjects who had undergone a partial foot amputation. The population involved subjects with diabetic neuropathic ulcers without peripheral arterial disease. It was a slightly younger population and was predominantly male (81%). The authors found a higher complete healing rate in the NPWT group (56%) than subjects in the standard care group (39%) (P = 0.04).19 Subjects experienced faster healing rates in the NPWT group as well with 100% granulation at 42 days (IQR, 40-56) in the NPWT group as compared to 84 days (IQR, 57-112) (P = 0.002). It appears that NPWT may provide some potential benefit with ulcers; however, the current evidence is limited to use in diabetic foot ulcers with adequate arterial supply.
Despite better evidence of healing, cost-benefit analyses have failed to show a cost savings for NPWT therapy, notwithstanding lower nursing costs and faster healing times in the single study examining the question.13 Nursing staff must be trained to effectively use NPWT, thus adding to the overall cost. The therapy may improve complete healing rates and speed of healing in diabetic foot ulcers; however, the cost-effectiveness is unclear.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) has rapidly emerged as a potential alternative for healing chronic wounds since 1968.8 The biology behind the HBOT’s effectiveness has not been fully evaluated. A proposed hypothesis includes an increase in oxygen tension at the wound site.20 The etiology of chronic wounds involves reduced tissue perfusion through direct arterial ischemia or relative ischemia from edema or pressure that reduces blood flow to the skin. Some healing processes are oxygen-dependent, thus, the biological rationale for the use of HBOT. With this potential biological plausibility, providers have used HBOT for chronic wounds. The ulcer type with the most evidence is the diabetic neuropathic foot ulcer.8 The outcome of many of these studies has been amputation. This outcome is especially important for community-dwelling older adults and ambulatory LTC residents, because of both the high prevalence of this diabetic complication as well as the cost and decreased quality of life associated with amputation.
Previous systematic reviews8 have found only five RCTs that investigate HBOT in subjects with nonhealing ulcers.21-25 Four studies involved patients with diabetic foot ulcers.21,23-25 There were a total of 147 subjects in those four RCTs, with the largest trial enrolling 70 subjects. The primary outcomes for these four trials were subsequent amputation and complete wound healing. After pooled analysis, there were decreased rates of amputation in individuals who used HBOT as compared to regular care (relative risk [RR], 0.31; 95% confidence interval [CI], 0.13 to 0.71). The number needed to treat (NNT) was 4 (95% CI, 3-11).8 Only one trial of 18 subjects observed insignificant differences in healing at 6 months, but significant differences in rates of healing at 1 year, with a benefit of HBOT over standard care (62% healed in HBOT vs 0% in standard care; P = 0.026).25 Investigators evaluated the effectiveness of wound size reduction in one RCT of HBOT in subjects with venous ulcers.22 Of the 16 subjects, there was a reduction in wound size at 6 weeks; however, there was no difference in healing.22 Thus, HBOT might prevent amputations, but improved healing rates have not been conclusively demonstrated. In general, studies of ulcer healing with HBOT were small and involved single sites.
Hyperbaric therapy has limitations. It is expensive, with only one study performing a cost analysis.25 This British study involved 18 randomized subjects with diabetes who received HBOT or standard practices. The number of visits was lower in the HBOT group (33.75 visits/yr) as compared to the control group (136.5 visits/yr). Despite a higher ₤100 cost for each HBOT visit compared to a standard wound visit (₤58), the fewer visits in the HBOT group could account for a savings of ₤2960 a year.25 Thus, there might be cost savings; however, this was a very small trial in England and might not represent a cost savings in North America. A second major limitation is the lack of information on use of HBOT for pressure or ischemic ulcers. Both ulcer types are common in LTC, with the prevalence of stage 2 or higher pressure ulcers as high as 6.2%.26
HBOT remains an option for residents in facilities close to a hyperbaric chamber. However, many questions remain on use of HBOT in LTC residents. First, there are little data beyond the information on amputation, such as healing rates or speed of healing. Cost analysis is based upon only one study with 18 patients.25 There is no information on the use of HBOT for pressure ulcers or ischemic ulcers. Practical issues such as transportation to the HBOT chamber from the facility also remain a factor. The use of HBOT as a standard therapy for residents in general should be viewed with caution, and providers should utilize HBOT when the potential benefits to the resident can be defined.
Silver-Based Therapy
Silver-based therapy is a topical treatment used in chronic wounds in LTC. Silver agents have long been recognized for their broad-spectrum activity against bacteria, viruses, and fungi, which reduces the bioburden in the wound.27 Silver agents are used primarily for the silver ion effect, which may bind to the bacterial wall and cause disruption.27 Silver can be used as a cream (silver sulfadiazine) or in a matrix with another wound therapy, such as an alginate or foam. There have been three RCTs evaluating silver-based therapy.28-30 Eight hundred forty-seven participants were enrolled in these three studies with one trial having 619 subjects.30 The primary outcomes included complete healing, ulcer size post-treatment, and wound drainage. In the largest trial, the investigators found a 47% decrease in wound area with a silver foam as compared to a 32% decrease with best practice (P = 0.002).30 Exudate level in the silver group decreased from moderate to low, while it stayed the same in the best practice group (P = 0.0055). Complete wound healing was not evaluated. The ulcer types noted in the study included mixed ulceration (ischemic and venous) in 21% of subjects, venous ulcers in 46%, and pressure ulcers in 8%.30 The remaining two studies found no difference in wound healing with the silver compounds.28,29 One study did show a decrease in wound size with a silver foam as compared to a standard foam (45% vs 25%). Drainage also appeared to decrease in this study, with 19% with exudate in the silver-foam group versus 49% in the foam group.28
There are limitations with the supporting evidence of silver therapy. There are no RCTs that show superiority of silver-based therapy compared to other methods for complete wound healing. Systematic review of RCTs has also failed to support the superiority of silver therapy.9 It appears that there may be improvement in wound characteristics with decreases in drainage, exudate, maceration, pain, and size with silver therapy.30 How this correlates with clinical care in LTC has not been fully determined. Potential uses of silver-based therapy could include wounds with significant exudate, size, or pain. It is unclear how this therapy would work with ischemic ulcers. True cost analysis has not been performed for silver-based therapy; however, time for dressings has been lower in one study.30 Silver-based wound therapy can be used in LTC with the recognition of the limitations above.
Ultrasonic Mist
Ultrasonic mist is a newer wound technology based upon the effects of ultrasound using thermal and nonthermal mechanisms. Traditional contact therapeutic ultrasound is generally applied at a frequency of 1-3 MHz while the mist unit uses ultrasound energy at 40 kHz. Low-frequency ultrasound enhances metabolism, perfusion, and granulation.31 Two RCTs have evaluated ultrasonic mist and wound healing. One study was a single-center trial of 70 subjects who were randomized to either ultrasonic mist for 5 minutes three times a week with local best practice (LBP) or LBP alone.32 The primary outcome was 50% reduction in wound size at 12 weeks. 63% of individuals using mist therapy achieved the primary outcome as compared to 29% in LBP (P < 0.001).32 This study population included patients with predominately ischemic ulcers, with or without a venous component. A multicenter RCT with 133 subjects did examine the effectiveness of ultrasonic mist in achieving complete wound healing at 12 weeks for diabetic foot ulcers.33 Following exclusion of participants secondary to protocol violations, the investigators analyzed only 55 of the 133 randomized subjects. Using per protocol analysis, 40.7% of subjects (n = 27) randomized to ultrasonic mist achieved complete wound healing at 12 weeks as compared to 14.3% (n = 28) in the sham group (P = 0.0366).33 However, on using intention-to-treat analysis, there was no difference between the two groups.
Both RCTs have methodological problems that weaken the validity of the findings. The larger trial did have significant healing using per protocol analysis; however, using intention-to-treat analysis, there was no difference between the two groups. The other trial did not have blinding to the active intervention. The use of ultrasonic mist certainly might provide some improvement in healing; however, current studies leave questions as to the efficacy and effectiveness of this therapeutic modality. Additionally, there has not been a cost-effectiveness analysis favoring ultrasonic mist over conventional wound practices.
Pressure Reduction Mattresses
Pressure reduction is one of the fundamental concepts used in treating and preventing pressure ulcers. Traditionally, frequent repositioning still provides an excellent method of pressure reduction; however, it is time- and labor-intensive, and can be limited by patient characteristics and conditions. Pressure reduction mattresses are divided into different categories, with one being a continuous low-pressure (CLP) device, and the other a powered device with either an alternating low-pressure system or an air-fluidized system. A meta-analysis has been published that included 41 RCTs using mattresses for pressure ulcer reduction.10 Seven RCTs compared CLP mattresses to standard hospital mattresses10,34-38 and assessed the effect on the development of pressure ulcers (RR, 0.40; 95% CI, 0.21-0.74).10 Powered support surfaces were reviewed, with comparisons between alternating pressure surfaces and standard mattresses, as well as CLPs. One study of 482 subjects evaluated an alternating pressure surface compared to a standard hospital mattress. The use of the alternating pressure surface significantly protected against the incidence of pressure ulcers (RR, 0.32; 95% CI, 0.14-0.74). Eight trials comparing alternating pressure with CLP for the development of pressure ulcers found mixed results.10 Cost-effectiveness analysis for both prevention of pressure ulcers and treatment have been performed looking at both the cost of the device and the quality-of-life year per patient. CLPs are cost-effective for the prevention of pressure ulcers, and powered surfaces are cost-effective for treatment of pressure ulcers.39
These studies on pressure reduction mattresses demonstrate a reduction in the incidence of pressure ulcers as compared to standard mattresses, which is important for LTC. There does not appear to be one mattress or device that is markedly superior to another device. As such, it is reasonable to conclude that most high-risk individuals should be placed on pressure reduction mattresses. Residents in LTC would be considered high risk in many cases, thus, the potential need for widespread adoption of pressure reduction mattresses in facilities. Providers should utilize powered pressure reduction devices for the highest risk residents or in patients with ongoing deep, high-stage, nonhealing pressure ulcers.
Summary
The necessity of wound technology continues to grow as the complexity and prevalence of chronic wounds increases. It is clear that the most practical technology for LTC is the use of specialized wound mattresses that provide support for frail residents and could potentially prevent new pressure ulcers. Constant low-pressure devices provide practical solutions for most needs in LTC. Providers can use negative pressure, hyperbaric oxygen, silver therapy, and ultrasonic mist as potential options for nonhealing ulcers when warranted.
The authors report no relevant financial relationships.










