Utilization of Pen Devices Can Improve Diabetes Treatment for LTC Residents
Author Affiliations: Dr. Resnick is Professor, University of Maryland School of Nursing, Baltimore, MD.
Abstract: The prevalence of diabetes is increasing at an alarming rate worldwide, and, coupled with an aging population, it is expected that the number of persons with diabetes requiring long-term care will increase substantially over the next several decades. Therefore, it is imperative that optimal treatment is provided to reduce the associated health problems and improve the quality of life for those with the disease. Many of the barriers to adequate glycemic control can be overcome, and insulin therapy should be considered with the patient at the time of diagnosis. Traditional vial-and-syringe delivery is a valid insulin therapy option, but studies have demonstrated that some patients prefer pen devices over vial and syringe. Pen devices have also been associated with fewer hypoglycemic events and reduced emergency and physician visits. This delivery approach, therefore, may have a significant impact on patient quality of life. (Annals of Long-Term Care: Clinical Care and Aging 2008;16[11]:28-32)
___________________________________________________________________________________________________________________________________
Background
Diabetes mellitus is a chronic condition that requires lifelong treatment. By 2030, it is projected that the disease will affect nearly 4.4% of the worldwide population.1 In 2005, it was estimated that 7% of the U.S. population (approximately 20.8 million people) had diabetes that resulted in a $132 billion burden on the economy.2 The prevalence of diabetes is highest among the elderly. In 2004, 16.7% of persons age 65-74 years had been diagnosed with diabetes, which was approximately 12 times the rate of people aged younger than age 45 years (1.2%).1,3 Many of these elderly patients are admitted to nursing facilities for long-term custodial care, where the prevalence of diabetes is estimated to be between 8% and 25%.4
As life expectancies increase worldwide, the number of people who will require long-term care is expected to increase as well.5 When this demographic shift is coupled with the increasing prevalence rates of diabetes in the elderly, an even greater number of nursing care facility residents will require diabetes care. This will further increase the burden on the economy, and optimal LTC treatment are needed to reduce health problems and improve quality of life for those with the disease.
Management of Glycemic Control in LTC
Inadequate glycemic control is a major cause of diabetic complications such as cardiovascular disease, diabetic neuropathy, kidney disease, and nervous system damage.2,6,7 Intensive glycemic control, which is considered the critical marker of successful diabetes treatment, can prevent or delay the progression of these devastating complications.7-10 Glycemic control is defined by the American Diabetes Association as a glycosylated hemoglobin (A1c) value of less than 7% for patients in general, whereas the recommended A1c goal for individual patients is as close to normal as possible without significant hypoglycemia.11
However, not all individuals in LTC settings will benefit from strict glycemic control. In this setting, target A1c levels should be individualized, and a less-stringent target of 8% is more likely to be realistic and appropriate.12,13 In patients who are considered frail, have a life expectancy of less than 5 years, or present with any condition or comorbidity indicating that the risks of glycemic control would outweigh the benefits, quality-of-life considerations should take precedence over general guidelines. To this end, the American Medical Directors Association (AMDA) clinical guidelines for the management of diabetes in the nursing home does not stress the use of A1c as the gold standard for diabetes management; however, the philosophy of optimal glycemic control is certainly important for LTC residents.12 Many of these patients are managed on insulin, and it is essential to discuss diabetes management goals, and how these are related to current diabetes guidelines11,12 with the patient and/or his or her proxy. These goals should be reviewed regularly along with the management plan.
Impact of hyper- and hypoglycemia
In elderly patients, an adequate level of glycemic control prevents some of the acute complications of diabetes (eg, delays in wound healing) and symptoms of hyperglycemia (eg, polyuria and fatigue).13 Interestingly, achieving adequate glycemic control has also been associated with improvements in overall cognitive function and improvements to memory, attention, concentration, and conceptual thinking in the elderly.13,14 Unfortunately, complications of hyper- and hypoglycemia are noted to occur in the course of diabetes management and have an impact on residents’ quality of life.6,7 Hypoglycemia is a serious complication of diabetes management in elderly patients and is a major barrier to achieving tight glycemic control.15 Hypoglycemia has been shown to be an important risk factor for reduced health-related quality of life16 and can increase the risk of cardiovascular events (myocardial ischemia, angina), stroke, impaired cognition, and falls in the elderly.17,18 Hypoglycemic events are often attributed to insulin administration errors and, in the LTC setting, can be related to high staff turnover and inadequate assessment of resident status.14,19
Hypoglycemia can be a frightening event for both residents in LTC settings and their caregivers, and outcomes of even a mild episode can be poor and are more devastating than in younger patients. For example, hypoglycemia causing dizziness or weakness in a frail elderly person may cause a fall and result in an injury that requires hospitalization.19 A general lack of awareness of the early signs and symptoms of hypoglycemia among residents and their caregivers can also contribute to an increased risk of serious hypoglycemia.20 Older adults, when compared with younger individuals, are more likely to experience neurologic symptoms of hypoglycemia, such as dizziness, weakness, and confusion.14,21 Notably, a lower glycemic threshold to hypoglycemia in the elderly may limit the time available to treat the condition, thereby increasing the risk of developing incapacitating neuroglycopenia.21
Insulin Therapy: Potential Implications of Pen Device Use for LTC Residents
It is common practice to prescribe human insulin or an insulin analog for patients with diabetes. However, the use of traditional vial and syringe for delivery has several disadvantages, including difficulty of drug storage and transportation, fear of injection, impact on lifestyle, lengthy training time, and social embarrassment, all of which may affect patients’ adherence to therapy and, subsequently, glucose control.22 Furthermore, insulin dosing via syringe is associated with a high risk of dosage errors.23 In some states, individuals living in assisted living (AL) facilities may be forced to move to a nursing home setting if insufficient nursing services are available to administer insulin on a sliding scale basis.
One option to facilitate insulin administration is the use of pen devices. Although no studies have specifically assessed the use of pen devices in older patients with diabetes living in LTC facilities, such patients are likely to experience the benefits demonstrated in general populations of patients with diabetes. The use of pen devices as method of insulin administration has been shown to make the insulin administration procedure quicker; assure more accurate dosing; improve reliability, durability, convenience, and discretion; and are reportedly easy to use.24,25 In addition, pen devices can significantly improve quality of life, irrespective of injection regimen or metabolic control prior to pen use26 and are associated with positive psychosocial benefits27 and improved well-being.28-31
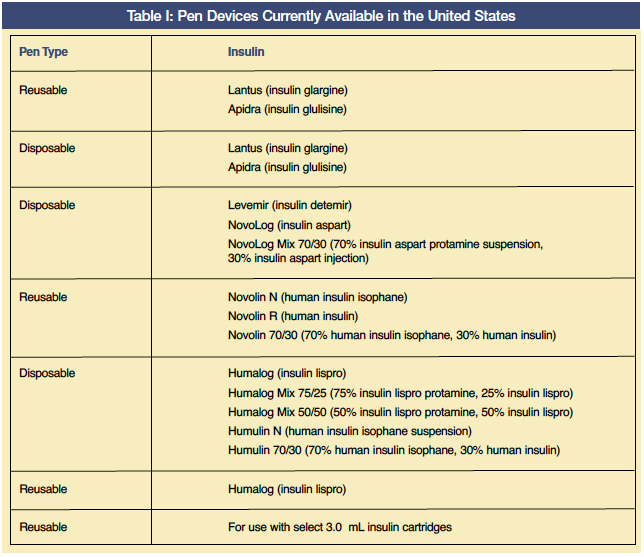
A number of pen devices are now available in the United States (Table I), and studies have shown that patients who independently manage their insulin prefer this method of administration over vials and syringes.29,32-37 In an observational study that included 1622 insulin-treated patients (mean age approximately 57 years) who switched from vial and syringe to a pen device, there were statistically significant improvements in all items of the Diabetes Treatment Satisfaction Questionnaire (eg, ease of treatment, flexibility, hypoglycemia status, and satisfaction).32 In another study of 372 patients with type 2 diabetes (52% age ≥ 60 years) who switched to an insulin pen device, significant improvements occurred in all measures of patient-reported outcomes, including convenience, flexibility, and overall preference.34 In a randomized, open-label, comparative, crossover trial that included 121 patients with type 1 or 2 diabetes (mean age, 57 years), 74% of patients indicated a preference for an insulin pen over the vial and syringe.29
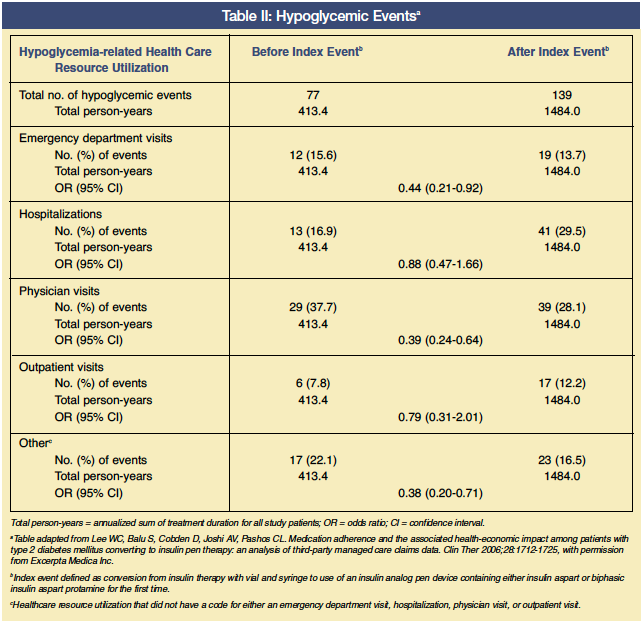
A recent health economic study demonstrated the real-life value of switching from conventional human or analog insulin injection (vial and syringe) to an insulin analog pen device.38 In this study, a pre-post analysis was performed on a cohort of 1156 patients with type 2 diabetes from an integrated medical and pharmacy claims database containing information on more than 40 million covered lives from 57 managed care health plans in the United States. The mean age of this population was 45 years and, therefore, was likely to be mostly community-based. A total of 595 (51%) patients were previously treated with a human insulin vial and syringe and 561 (48.5%) patients were previously treated with an insulin analog vial and syringe. In this study, the number of hypoglycemic events was significantly reduced after switching to a pen device (odds ratio, 0.50; 95% CI, 0.37-0.68; P < 0.05) and the incidence of hypoglycemia was reduced by nearly two-thirds in patients who were adherent to therapy (incident rate ratio 0.35; 95% CI, 0.21-0.92; P < 0.05). With regard to hypoglycemia-related healthcare utilization, there were significant decreases in emergency department and physician visits for hypoglycemic events, but not in hospitalizations or outpatient visits (Table II). The insulin pen device was also shown to be cost effective; total all-cause annual treatment costs were reduced by $1590 per patient (from $16,359 to $14,769; P < 0.01) after switching to the pen device.
It should be recognized that one of the risks associated with pen use is potential needlestick injury. In a recent 1-year retrospective study conducted in 24 sentinel French public hospitals, the incidence of healthcare workers receiving needlestick injuries from injection pens was six times higher than from disposable syringes.39 It has been suggested that healthcare workers are mainly injured when they have to recap or manually disassemble the needle from the pen in order to store the pen for later use.40 In response to this problem, the newer “passive” pen devices now automatically provide needle safety after the injection has been completed, without the nurse or caregiver having to modify their behavior.
Conclusion
Insulin therapy is often appropriate for LTC residents and should be given as needed to optimize quality of life by decreasing the risk of hyperglycemia or hypoglycemia that commonly occurs with some oral agents and vial-administered insulin. In LTC, the day-to-day impact of diabetes management on functional activities, mood, and quality of life is of great importance. As pen devices are associated with improvements in quality of life and well-being, they may be a useful option for insulin delivery among LTC residents. For the nurses who administer insulin, the pen devices can greatly reduce the time required for preparation of insulin injections and the risk of dosing errors.
For residents in AL facilities who may be able to self-administer insulin with a pen device, the benefits may extend not only to increasing their sense of independence, but also to decreasing the cost of their care. Overall, these devices are likely to improve patients’ quality of life and compliance with insulin therapy, thereby resulting in improved long-term clinical outcomes and lower associated healthcare resource utilization and costs.
Acknowledgments
The author thanks Mark Walker, PhD, of Complete Medical Communications, who provided medical writing support funded by Novo Nordisk Inc.
The author has received speaker honoraria from Amgen and Ortho Biotech, and has been a consultant or paid advisory board member for Amgen and Janssen/Johnson & Johnson.