Managing Chronic Constipation in Long-Term Care Settings
Constipation in the elderly is common and has a significant impact on quality of life and use of healthcare resources in long-term care settings. A careful history, medication assessment, and physical examination are helpful in obtaining relevant clues that help direct management. Fiber supplementation and osmotic laxatives are effective for many patients. Simplifying bowel programs saves time and energy and provides a more unified approach to care. Special effort should be taken to identify features inherent to the elderly, and treatment should be based on the patient’s overall clinical status and capabilities. Facilities should establish policies and procedures that promote good bowel function, understand the factors that contribute to this problem, and approach each resident to best meet his or her expectations. (Annals of Long-Term Care: Clinical Care and Aging 2009;17[9]:22-24)
__________________________________________________________________________________________________________________________________
Constipation is variably defined, and its diagnosis is often arbitrary. Chronic constipation (CC) is a common problem in the elderly, with a variety of etiologies including pelvic floor dysfunction, medication effects, and numerous age-specific conditions. Most epidemiologic studies demonstrate a higher prevalence of constipation and laxative use in the elderly,1,2 particularly in the institutionalized, where studies suggest a prevalence for constipation as high as 50%, with up to 74% of nursing home residents using daily laxatives.3 The more patient-centered we make our approach to constipation, the greater the variability and the higher both the incidence and prevalence of symptoms.
 In addition to advanced age, risk factors for CC include female sex, nonwhite race, physical inactivity, low income and education level, medications, dietary intake, and depression.4 Severe constipation is seen almost exclusively in women, with elderly women having rates of constipation two to three times higher than that of their male counterparts.5 The elderly, who often underestimate their stool frequency, frequently plan their days around their bowel movements, and treatments often precipitate loose stools and incontinence.
In addition to advanced age, risk factors for CC include female sex, nonwhite race, physical inactivity, low income and education level, medications, dietary intake, and depression.4 Severe constipation is seen almost exclusively in women, with elderly women having rates of constipation two to three times higher than that of their male counterparts.5 The elderly, who often underestimate their stool frequency, frequently plan their days around their bowel movements, and treatments often precipitate loose stools and incontinence.
Treatment of CC depends on the underlying physiologic etiology, being mindful of other factors that may influence the presentation, as shown in the “The Ten ‘D’s’ of Constipation” in Table I.
As a general rule, patients who do not respond to fiber supplementation can be advanced to osmotic laxatives, which can be titrated to clinical response. Stimulant laxatives and prokinetic agents are typically reserved for patients with more refractory constipation. No single agent or program is best for all patients or situations. The commonly used categories of agents are listed in Table II.
Treatment needs to be tailored not only to etiology but also to medical history, medications, overall clinical status, mental and physical abilities, tolerance to various agents, and realistic treatment prospects. Monitoring bowel movement frequency, stooling patterns, fecal soiling, and use of laxatives may help in the development of an overall treatment regimen tailored to the individual patient. Specific issues for institutionalized patients need to be addressed with standardized, supervised bowel programs. Each facility should have a program and policy in place that is easy to understand and simple to implement.
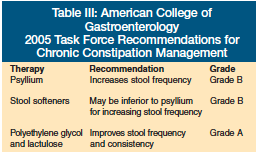 Clinicians should also be mindful of what evidence exists for our patient population in treating their condition. The last definitive word from the American College of Gastroenterology was published in 20051 (Table III), though at least one newer agent, lubiprostone, has shown effectiveness in a population over age 65.6 The task force cited insufficient data to make recommendations for all other treatments, including combination laxatives.
Clinicians should also be mindful of what evidence exists for our patient population in treating their condition. The last definitive word from the American College of Gastroenterology was published in 20051 (Table III), though at least one newer agent, lubiprostone, has shown effectiveness in a population over age 65.6 The task force cited insufficient data to make recommendations for all other treatments, including combination laxatives.
There are also a number of interventions that take excessive time and provide very little benefit. “Lubricate the bowel” has been an institutionalized mainstay of an approach to CC that is now severely out of date. There is no evidence that excess fluid improves constipation in individuals who are adequately hydrated.7 Certainly, people who are dehydrated have more difficulty with constipation, but individuals with adequate fluid have constipation for other reasons.
No matter the care setting, if we overly fixate on hydration, we are wasting time and resources and misdirecting our energies. It takes a lot of effort for some of our frailest patients to get to the bathroom, and there is always a greater chance to slip and fall. In fact, if we overhydrate, a condition known as “water intoxication” can develop, where we experience fluid and electrolyte imbalance characterized by confusion, listlessness, and even apathy.
It is also a myth that fiber improves symptoms of constipation in all patients.8 It is appropriate to provide enough bulk and fluid to form soft stool, but in patients with severe constipation it can make their symptoms worse. In addition, in patients with slow bowel transit,9 natural fiber has an opportunity to sit in the gut and ferment. The longer it lingers, the more gas it creates. Many a nursing home has gone through the process of adding fiber to the meal plan only to back off when cramps, bloating, and flatulence take over.
There is also no proven evidence that products containing two or more laxatives are better than one, and the risks may outweigh the benefits.1 No studies using combinations have been shown to be more effective than single agents. Moreover, with combinations we are never quite sure what may be working and what might be causing even more problems.
It is often written and regularly taught that exercise is good for the bowel. Appropriate activity (ie, just being up and about) seems to make the most sense. It also holds true that when people are immobile, their bowels slow down and constipation gets worse.10 However, formal trials of moderate-intensity exercise training in long-term care residents failed to provide any particular benefit for patients with constipation.11 Whether it was strength training, functional training, or combined training, the control group did best over 6 months with their symptoms of constipation.
There is no frequency of bowel movement or consistency of stool that should be considered ideal. The relationship between our bodily habits and our daily routines are tightly linked. A person-centered approach understands these variables and listens for the unique tick of our personal metronome. Long before there were drugs, people were taking advantage of the body’s natural rhythms and the food products around them to help produce normal bowel movements. How good we feel and how well we perform contributes to the rhythm of life.
Once we understand an individual’s internal clock, we can use it to an advantage for both ambulatory as well as functionally compromised individuals. In the nursing home, prompted voiding is a strategy often employed to help with spontaneous urination or bowel movements rather than incontinence.
A basic understanding of gut physiology can play to our advantage, and the neuroendocrine functions of the bowel are continuing to be elucidated.12 The gastrocolic reflex that young parents first discover in their newborns, and then forget about in later life, is a powerful reaction that can be put to good use even as we age. Feed a baby, and shortly thereafter you will be changing a diaper. As we age, we never completely lose this reflex, and for many adults, the routine of a bowel movement (or the timing of a bowel movement) can often be clocked from the time of breakfast, lunch, or even dinner (though the reaction is stronger earlier in the day).
The meal is often followed by the physiologic response that prompts peristalsis in the bowel, a mass movement, and defecation. Whether it is 30, 60, or 90 minutes after a meal, the bowel kicks into gear and the physiologic response predictably repeats itself. With good timing, we can go to the bathroom with high expectations. The habit that includes psychological preparedness and relaxation helps with the defecatory process.
Breakfast is also often the time of starting the day with caffeine. This natural stimulant has been used throughout the ages for a variety of functions. Caffeine is a good bowel stimulant, and whether in coffee, tea, soft drinks, or even chocolate, it can be used to advantage. Never discourage the patient with constipation in their use of caffeine if it seems to produce a positive response. Since we take most of our caffeine in some type of fluid, this also works to our advantage.
Fluid in excess makes us urinate more, but appropriate amounts of fluid help keep stool the right consistency. (Appropriate hydration to create good lubrication and a bulky stool has been addressed in previous articles in this Journal.) In order for many of our bulk-forming laxatives to work, fluid and fiber go hand in hand. A larger, bulkier stool creates a better physiologic stimulus, reduces bowel-wall tension, and drives the mass movement in the colon. A bulkier stool at the rectum also serves as the appropriate stimulus to prompt the sensation for defecation and then muscular relaxation at the anus.
As we listen to our patients, not having a good bowel movement can ruin an otherwise good day. Conversely, starting the day with one is always a good sign. Taking advantage of the body’s natural rhythms may be one of the best ways to treat CC. It is also highly patient-centered, as should be our entire approach to CC.
Dr. Tangalos has received speaker honoraria from and is an advisory board member for Medical Communications Media and developed an educational series for E-IMPACCT, a program on constipation supported by an educational grant from Takeda Pharmaceuticals.
Dr. Tangalos is Professor of Medicine, Mayo Clinic, and Medical Director, Bethany Samaritan Heights, Rochester, MN.










