Institutional Strategy for the Prevention and Management of Influenza and Pneumococcal Disease in the LTC Setting
Influenza and pneumococcal disease are major causes of morbidity and mortality within the long-term care (LTC) continuum. Influenza kills an average of 36,000 Americans annually, with more than 90% of those deaths occurring in the elderly. While vaccination rates of LTC facility residents for influenza and pneumococcal disease have increased over the past decade, rates now appear to have reached a plateau. Since frail or debilitated individuals may not respond to vaccination with a protective immune response, low rate of immunization in healthcare workers, contact care, and communal living further increase the risk of transmission. Given the significant rates of morbidity and mortality, strategic steps must be taken to prevent and manage influenza and pneumococcal disease in LTC. (Annals of Long-Term Care: Clinical Care and Aging 2010;18[2]:20-26)
_____________________________________________________________________________________________________________________________________________________
Introduction
Influenza and pneumococcal disease are major causes of morbidity and mortality within the long-term care (LTC) continuum. Influenza kills an average of 36,000 Americans annually,1 with more than 90% of those deaths occurring in the elderly; residents of LTC facilities are particularly at risk.2,3 In one well-studied outbreak, 65 residents developed influenza, of whom more than half developed pneumonia and two died.4 Illness rates up to 60% and fatality rates as high as 55% have been documented during influenza outbreaks in LTC facilities.5-8 Influenza and pneumococcal disease cause more deaths in the United States than all other vaccine-preventable illnesses combined.9,10 Influenza and pneumonia combined represent the fifth leading cause of death in the elderly; up to 20,000 residents of LTC facilities succumb to these illnesses (influenza and pneumococcal pneumonia) every year.11,12 The goal of this article is to discuss the strategic steps that must be taken to prevent and manage influenza and pneumococcal disease in LTC settings.
Vaccination in LTC
Since frail or debilitated individuals may not respond to vaccination with a protective immune response, low rate of immunization in healthcare workers, contact care, and communal living further increase the risk of transmission. Given the significant rates of morbidity and mortality, strategic steps must be taken to prevent and manage influenza and pneumococcal disease in LTC. Institutional interventions that can limit the spread of both the seasonal and H1N1 virus and reduce the morbidity and mortality of those infected can be of benefit to those living in LTC facilities.
Ample evidence exists to show that influenza vaccination of both residents and staff is beneficial in reducing hospitalizations and mortality rates.13 While vaccination rates of LTC facility residents for influenza and pneumococcal disease have increased over the past decade, rates now appear to have reached a plateau. Among Medicare beneficiaries, influenza and pneumococcal vaccines remain underused despite the fact that both are cost-effective, covered under Medicare Part B, and efficacious.
Federal regulations provide financial and regulatory incentives to increase influenza and pneumococcal immunization rates. The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) and the American Medical Directors Association (AMDA) recommend that influenza and pneumococcal vaccinations be targeted to persons who are over age 65 and those who are chronically ill. The influenza and pneumococcal disease vaccine is indicated for all residents of LTC facilities who are over age 65 and/or who have chronic medical conditions. This means that basically all residents of LTC settings are candidates for both influenza and pneumococcal vaccination.14 The Centers for Medicare & Medicaid Services (CMS) requires offering residents the influenza and pneumococcal vaccines, with rates reported in the Minimum Data Set (MDS) and as a Quality Indicator. So the question remains: Why aren’t we reaching Healthy People 2010 goals of 90% vaccination for both vaccines?15 (Note: Healthy People 2010 is a set of health objectives for the nation to achieve.)
While residents of nursing homes (NHs) are not in the “target” population for receiving priority for the H1N1 vaccine, a recent Journal of the American Medical Association article showed that persons age 50 years and older infected with the H1N1 virus had the highest mortality rates among all ages once hospitalized.16 Therefore, it would be prudent to offer residents of NHs the H1N1 vaccine if sufficient supply becomes available to permit their vaccination.
Waning Immunity in Older Adults
In older adults, waning immunity affects cellular responses and antibody titers. In addition, the immunological changes that occur in frail or debilitated individuals interfere with accumulating a protective response to vaccination.17 Influenza immunization decreases the risk of hospitalization and death, while pneumococcal vaccination decreases the risk of invasive disease. A subgroup analysis of data from immunocompetent older adults included five studies showing that the polysaccharide pneumococcal vaccine reduced the risk of invasive pneumococcal disease, with a pooled estimated odds ratio (OR) of 0.32 (95% confidence interval [CI], 0.22–0.47).18-21 The ACIP notes that although influenza vaccination in the frail elderly may not prevent illness, it is 50-60% effective in preventing influenza-related hospitalizations or pneumonia and 80% effective in preventing death.22-25 Waning immunity is thought to be an important risk factor for pneumonia in the elderly.25,26 (This knowledge of decreased morbidity and mortality should motivate both residents and staff to ensure that vulnerable elders are immunized.)
Healthcare Worker Immunization
Despite evidence that healthcare worker immunization protects residents from influenza and its complications (eg, death), vaccination rates remain unacceptably low.27 A literature review of 32 influenza immunization programs conducted in the United States, Canada, and Europe between 1985 and 2002 found that vaccination rates among healthcare workers ranged from 2.1% to a high of 82%, with the majority achieving rates less than 50%.28 (A 2003 CDC report showed that only 36% of the nation's healthcare workers were vaccinated against influenza, and that healthcare workers had been a source of influenza outbreaks in healthcare settings.29) According to the APIC, immunization will be especially critical for healthcare personnel during the 2009-2010 flu season because there will be more than one virus circulating. Healthcare personnel are of a younger population, and therefore those who are of the H1N1 “target” population should be sure to get immunized for both the seasonal and H1N1 vaccines, especially to prevent a workforce crisis.
Unvaccinated healthcare workers can introduce influenza into the LTC setting and spread infection once it is present. Studies have shown that low vaccination rates among healthcare workers are associated with influenza outbreaks in the LTC setting. On the other hand, higher levels of vaccination among healthcare workers are associated with a lower incidence of influenza infection.30 Influenza vaccination of healthcare workers protects vulnerable residents and decreases morbidity and mortality. In two studies conducted in NHs in the United Kingdom, vaccination rates of 50-60% among healthcare workers were associated with 40% reductions in mortality among residents.31,32 (One of the national health objectives for 2010 is to achieve healthcare worker vaccination levels of 60%.33)
AMDA stresses in its publication Immunization in the Long-Term Care Setting34 that possible reasons for low rates of influenza vaccination among healthcare workers include fear that the vaccine will give them the flu or that they will have severe vaccine-associated side effects, fear of injections, believing the vaccine is ineffective, inconvenience, cost, and many individuals not wanting to be told what to do. Healthy employees often consider themselves to be at low risk for “catching” influenza and are unaware of the role of transmitting influenza to vulnerable patients and their own families. Healthy employees may have few or even no symptoms once infected. Many healthcare employees do not seem to understand that even if asymptomatic, they may shed virus, exposing their patients, colleagues, and families. While healthcare workers report that they would stay home if they became ill, a study found that nearly 80% of healthcare workers went to work while being symptomatic with influenza-like symptoms.35
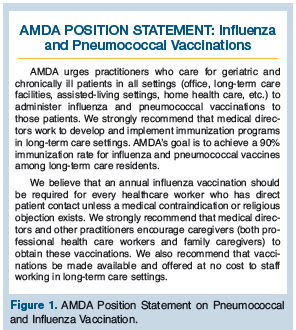 Widespread illness resulting from low vaccination rates among employees may also result in workplace absenteeism, increased work hours for remaining workers, and substantial costs for employers.1 In addition, staff vaccination decreases the likelihood that staff will become infected with the influenza virus and suffer severe illness.36 For all of these reasons, AMDA’s position statement (Figure 1) encourages LTC facilities to implement on-site healthcare worker immunization programs at no cost to the employee.
Widespread illness resulting from low vaccination rates among employees may also result in workplace absenteeism, increased work hours for remaining workers, and substantial costs for employers.1 In addition, staff vaccination decreases the likelihood that staff will become infected with the influenza virus and suffer severe illness.36 For all of these reasons, AMDA’s position statement (Figure 1) encourages LTC facilities to implement on-site healthcare worker immunization programs at no cost to the employee.
According to AMDA, consent procedures should be as simple as possible. Unless written consent is required by state law, it should be strongly discouraged. Requiring annual written consent by residents or surrogates may create an additional barrier to achievement of optimal vaccination rates. Consent policies and procedures should be clearly outlined for residents and family members at the time of admission. Consent for influenza and pneumococcal vaccinations should be obtained when a resident is admitted to the facility. The attending practitioner can order an annual influenza and pneumococcal vaccination for the resident simply by putting a check mark on a preprinted form and signing the order.
Federal regulations eliminated the requirement for specific practitioner authorization for the administration of pneumococcal and annual influenza vaccinations in LTC facilities.37 Nurses or pharmacists may be authorized by standing orders to administer vaccinations according to an institution- or practitioner-approved protocol without the need for a practitioner’s order or signature, where permitted by state law. According to the CDC, standing orders are the most consistent and effective method for increasing adult immunization rates. Studies have shown that standing orders can increase patient immunization rates to as high as 90%.22,38 A sample standing order policy by the Immunization Action Coalition can be found at www.immunize.org/catg.d/p3074.pdf.
Overcoming Barriers
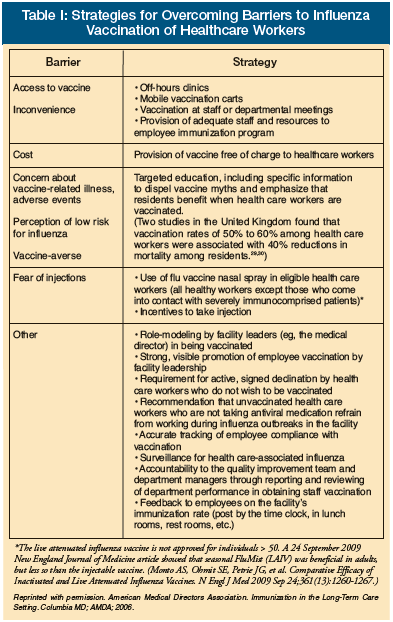 Some of the barriers to immunization in the LTC setting can be overcome with a leadership commitment to effective education and communication (Table I34).Therefore, leadership in LTC facilities should establish a yearly, organized campaign to promote immunization.39 Promoting immunization requires a strong component of education directed at residents, families, and staff. Most organizational barriers can be overcome through the establishment and implementation of detailed policies, procedures, and processes. The CDC, the 100% Immunization Campaign, and other organizations have sample policies, forms, and other tools that facilities can adapt for their own purposes.
Some of the barriers to immunization in the LTC setting can be overcome with a leadership commitment to effective education and communication (Table I34).Therefore, leadership in LTC facilities should establish a yearly, organized campaign to promote immunization.39 Promoting immunization requires a strong component of education directed at residents, families, and staff. Most organizational barriers can be overcome through the establishment and implementation of detailed policies, procedures, and processes. The CDC, the 100% Immunization Campaign, and other organizations have sample policies, forms, and other tools that facilities can adapt for their own purposes.
Staff Education
Information about vaccination should be part of ongoing staff orientation and education programs. Dispelling myths and misconceptions is crucial to a successful program. Visual tools and messaging appear to be more valuable to employee education than lecture. AMDA created a highly successful inservice DVD for healthcare workers that breaks down the myths and misconceptions of immunization, and uses healthcare employees of various ethnic backgrounds as “subject experts” explaining why they get immunized and why they feel that their peers should do the same.40 One large NH chain tracked the outcome on staff immunization rates using the AMDA DVD along with their annual influenza inservices and saw a rise of healthcare worker immunization of 28% above the previous year’s staff vaccine averages.
Unfortunately, even when vaccination is easy to obtain, as previously mentioned, some employees may be reluctant to be vaccinated when the primary reason is stressed for the protection of the frail residents they care for. It is important for healthcare workers to realize that they will benefit directly from receiving the vaccine. Therefore, programs to promote influenza vaccination should also emphasize benefits to individual staff members and their families.27
Nutritional Enhancement of Elderly Adults’ Immune Systems
LTC facilities should focus on institutional nutritional interventions that have been proven in the literature to provide benefit in relation to supporting elder adults’ immune systems to reduce the risk of infections. Nutritional enhancement of the immune system by supplementation for elderly adults appears to be a topic of exploration. It is known that nutritional status is a major factor influencing T cell responses. Immune changes in elderly persons may be secondary to deficiencies of macronutrients (energy and protein) and micronutrients (notably, vitamins B6, B12, and folic acid, as well as iron and zinc). Decreased immune response is associated with protein deficiency and protein energy malnutrition (a common problem in elderly adults), while deficiencies in the amino acids arginine and glutamine result in immune changes similar to those seen in the elderly. Micronutrient deficiencies may also play a role in poor immune response, especially zinc, vitamin D, and vitamin E.21 Fulop and colleagues21 pointed out that 200 IU of vitamin E supplementation for elderly NH residents “significantly reduced the risk of obtaining upper respiratory tract infection.” In addition, vitamin D supplementation may be helpful for frail older adults who have limited exposure to sunlight.41
Nutrient supplementation is often accompanied by an improvement in immune function, particularly in those who are nutrient-deficient.42 However, vitamins and minerals should be kept to the Recommended Dietary Allowances (RDAs) for optimal immune function. While the RDAs can be tied into effective immune function, studies have not shown that any further benefits are realized beyond those levels.43 In fact, Sriram and Lonchyna44 show that supplementation over and above the daily RDA can actually be harmful.
Phytosterol complexes are important because they target specific T-helper lymphocytes helping normalize their functioning, resulting in improved T-lymphocyte activity. Beta-Sitosterol complexes can have a positive result on the immune system by normalizing the dehydroepiandrosterone (DHEA):cortisol ratio.45 According to a published report in Alternative Medicine, stabilized rice bran seems to be one of the most potent and accessible sources of a complex mix of phytonutrients, beta-Sitosterols, and antioxidants,46 and one of the highest natural sources of phytosterols in nature.47,48 The phytonutrients and beta-Sitosterols in stabilized rice bran have been shown to enhance immune function, and therefore may be a supplement worth considering for elderly adults.49
Surveillance
The standard case definition for influenza lacks proven sensitivity in NH residents.The Wisconsin Veterans Home is a skilled nursing facility with an average daily census of 721, with four residential buildings within a two-block radius. Intense prospective surveillance, as part of funded prospective studies of influenza prophylaxis, was conducted over six influenza seasons.51 The first case of influenza in the last building affected occurred 27-64 days after the first case in this four-building facility. There was a common seasonal pattern of building attack rates. The study showed that if a season begins with severe outbreak in a single building, there would probably be similar attack rates in buildings affected later in that season. Delays between initial cases in buildings or facilities could allow clinicians to adjust defensive strategies after sampling attack rates and virulence in facilities affected earlier in the season. The decision to initiate influenza prophylaxis in a nursing building should optimally be made prior to the development of a full-blown clinical outbreak. Factors to consider included: (1) level of community influenza activity (a high level increases the likelihood of introduction by staff or visitors in multiple locations); (2) quality of the match between the circulating and vaccine strain (the most serious outbreak in the Wisconsin Veterans Home occurred during a year with a poor vaccine match—1997-98); (3) severity of outbreaks in NHs affected earlier in the season; (4) pattern of new clinical respiratory illnesses within the facility (clustered, severe cases demand prophylaxis); and (5) number and clustering of laboratory-confirmed cases (clustering implies transmission within the facility).
At the Wisconsin Veterans Home, clinicians initiate prophylaxis on the day that influenza is confirmed by rapid test if influenza is prevalent in the surrounding community—especially if there is a poor vaccine match or if they are aware of severe outbreaks in facilities affected earlier in the season. During an outbreak at the Wisconsin Veterans Home, a review of 154 culture-confirmed cases revealed that 19% never had a temperature greater than 99.5 degrees F during their illness, including five of 19 with infiltrates.50 Therefore, the Wisconsin Veterans Home utilizes “surveillance” case-finding criteria without a temperature threshold. A suspected case of influenza includes a new respiratory sign or symptom: cough, congestion, abnormal lung sounds, rhinorrhea, nasal congestion, sore throat, respiratory rate greater than 25, or deterioration in oximetry with supporting systemic symptoms and signs (fever, headache, myalgia, malaise, anorexia, heart rate > 100 bpm, deterioration in activities of daily living, or mentation). We realize, however, that such a broad definition is not specific for influenza infection, which may have an atypical presentation in impaired NH residents.
Once influenza is confirmed to be in the community, residents who meet the definition of a ‘‘suspect case’’ should have a nasopharyngeal specimen collected and tested for influenza to identify the first case in the facility. Negative rapid flu tests should be followed by culture or polymerase chain reaction (PCR), as rapid diagnostic tests are not sensitive enough to effectively rule out influenza.51
Outbreak Control
A CDC publication entitled “Infection Control Measures for Preventing and Controlling Influenza Transmission in Long-Term Care Facilities”52 declares that one case of confirmed influenza by any testing method in a LTC facility resident is an outbreak. Outbreak control measures should also be implemented in the face of “a sudden increase of acute febrile respiratory illness (AFRI) over the normal background rate.”52
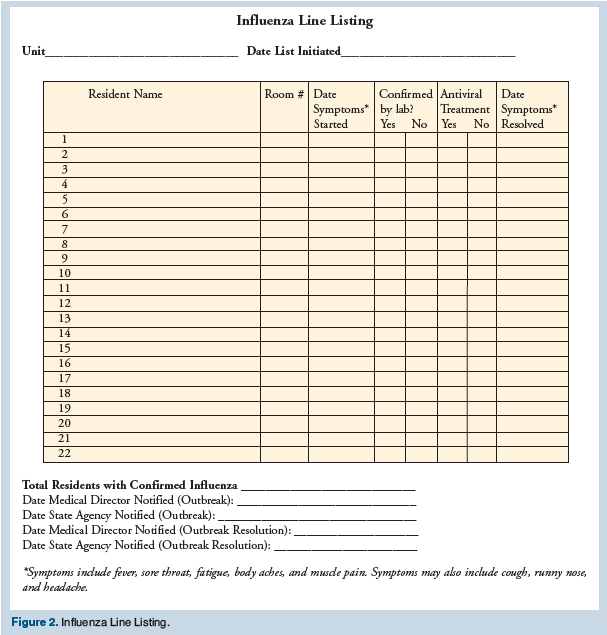
The outbreak threshold of a single NH–acquired, laboratory confirmed case is based on the likelihood that the single case represents the tip of an iceberg and the fact that influenza is extremely transmissible. Public health officials, therefore, recommend special control measures when there is evidence of transmission within the facility, rather than waiting for a full-blown “outbreak.” Once an outbreak is identified, a line list should be started and updated daily until the outbreak is over (Figure 2).
Antiviral Prophylaxis
Ideally, clinicians should begin antiviral prophylaxis within hours of receiving laboratory notification of a case of influenza (even on a weekend evening), within the context of a clinical outbreak of respiratory illness in the facility and/or an influenza outbreak in the community. Clinical benefit for treatment of infected residents is maximized when antivirals are begun within 48 hours of the appearance of symptoms. However, recent studies indicate that seriously ill hospitalized patients benefit even when treatment is started after 48 hours.53,54 The local health department should be notified as soon as possible that an influenza outbreak has been confirmed in the facility in states that require notification. The facility medical director should discuss antiviral medication use with the consulting pharmacist(s). Adequate antiviral medications should be available for immediate prophylactic use at any time, including evenings and weekends. Consult current CDC recommendations when choosing an antiviral agent.
Outbreak Infection Control Precautions
In addition to standard precautions, droplet precautions are appropriate in caring for a resident who has suspected or confirmed influenza. Table II34 lists additional infection control measures that are appropriate during a seasonal influenza outbreak. Precautions for pandemic influenza may go beyond seasonal influenza. While controversial, the CDC currently recommends the use of fitted N95 respirators at this time. The CDC also recommends 7 days of isolation and considering gastrointestinal secretions to be potentially infectious during the care of patients with suspected or confirmed H1N1 2009.55
Although isolation is difficult to achieve in the LTC setting, healthcare staff should attempt, to the extent possible, to keep infected residents in their rooms and away from other residents. In addition, communal activities on influenza-affected units should be canceled. The severity and spread of the outbreak may justify canceling communal activities throughout the entire facility for the duration of the outbreak. Because LTC facilities are social as well as healthcare environments, clinicians should try to the extent possible to balance infection control concerns and quality-of-life considerations.34
During the influenza season, it may be prudent to post signs at entrances and throughout the facility asking visitors not to enter if they have new respiratory symptoms. If an outbreak is particularly severe or widespread, a complete ban on visitors for the duration of the outbreak may be appropriate.
Summary
While influenza and pneumococcal disease are major causes of morbidity and mortality within the LTC continuum, strategies can be taken to reduce the incidence of these diseases in this setting. Increasing immunization rates among residents and healthcare workers is one major strategy that evidence shows will lead to improved outcomes. In older adults, waning immunity affects cellular responses and antibody titers. In addition, the immunological changes that occur in frail or debilitated individuals interfere with accumulating a protective response to vaccination. However, influenza immunization decreases the risk of hospitalization and death while pneumococcal vaccination decreases the risk of invasive disease. Unvaccinated healthcare workers can introduce influenza into facilities and spread infection once it is present. Studies have shown that low vaccination rates among healthcare workers are associated with influenza outbreaks in the LTC setting. In addition, it appears that nutrient supplementation may improve immune function, particularly in those who are nutrient-deficient. It is also critical that outbreak procedures be in place prior to any outbreak occurring, including a plan for antiviral prophylaxis.
Ms. Vance is an independent representative for Nussentials Corporation. Dr. Drinka reports no relevant financial relationships.
Ms. Vance is Director of Clinical Affairs, American Medical Directors Association, Columbia, MD; and Dr. Drinka is Clinical Professor of Internal Medicine/Geriatrics, University of Wisconsin, Madison, and Medical College of Wisconsin, Milwaukee.










