European Respiratory Society Annual Congress
September 12-16, 2009 Vienna, Austria
Update on the H1N1 Influenza Epidemic
The European Respiratory Society held its 19th annual congress in Vienna, Austria, September 12-16, 2009. This meeting has become the most important annual gathering of clinicians and researchers in the respiratory field (over 18,000 in attendance this year). This year’s congress was met with great anticipation because of its unique timing with respect to developments in the H1N1 influenza epidemic. The highlight of the congress was an up-to-the-minute symposium on the H1N1 pandemic, including sessions on the history and epidemiology of the influenza virus, clinical experience with the current pandemic, strategies for prevention and containment, and recommendations for health system preparedness. Key points from the symposium are summarized below. For more extensive review of the H1N1 pandemic developments and updates on clinical recommendations, visit the Centers for Disease Control and Prevention (CDC) website at www.cdc.gov and the World Health Organization (WHO) website at www.who.int.
H1N1 Influenza: Panic or Pandemic
Background and Epidemiology
An epidemiologist from WHO presented an interesting historical review of influenza epidemics and the epidemiology of the current H1N1 pandemic. Virtually all influenza disease that affects humans originates in bird species. The influenza virus is well adapted to infecting and transmitting through avian hosts. The influenza virus can also infect mammalian species wherever birds and mammals co-exist, but the virus must then mutate to successfully transmit from mammal to mammal. When the virus has made that mutation and adapts to transmission in the mammalian host, that animal is then a reservoir of a new strain of influenza that is potentially more infective to other mammals.
The current H1N1 virus has made the successful mutation from bird to swine, and then to humans, and has proven exceptionally successful in human-to-human transmission. In contrast, the H5N1 influenza virus, “avian influenza,” which is very infectious among bird species and is transmitted by both domestic and migratory birds, has shown only limited infectivity and ability to spread from human to human. Human cases of H5N1 influenza have been reported in Asia, Africa, Europe, and the Pacific, and it is extremely pathogenic, 60% fatal. Fortunately, it has not yet made the mutation for successful mammalian infection and transmission.
As of September 2009, there have been approximately 300,000 documented cases of H1N1 influenza worldwide and over 3000 deaths. Although this appears to be a mortality rate of about 1%, the denominator of total cases is likely much higher than 300,000 since many countries only report severe cases. To put these mortality statistics in perspective, the “Spanish flu” of 1918 was estimated to have killed over 40 million persons, and the “Asian flu” of 1957 and the “Hong Kong flu” of 1968 each killed 1-4 million persons worldwide. The annual seasonal influenza typically kills 250,000-500,000 persons each year.
These mortality statistics might seem to bode well for this pandemic; however, the CDC is forecasting up to 2 billion cases of H1N1 influenza worldwide. Even if the mortality rate is less than 1%, the huge denominator of cases could result in a high number of fatalities. Epidemiologists also caution that the greatest numbers of fatalities with the 1918 pandemic, also an H1N1 virus, came later in the second and third waves of the outbreak. The biggest difference between this pandemic and that of 1918 is that we appear to have an effective vaccine that is soon going to be widely available, as well as antiviral drugs to treat infected persons. Viral strain monitoring shows that the viral types in the southern hemisphere seen over the recent months have remained similar to strains isolated from the spring outbreaks in Mexico and the United States that were used for vaccine development. So far, more than 10,000 H1N1 isolates have been tested for sensitivity against the antiviral agents oseltamivir and zanamivir, and only 21 have demonstrated resistance (10 in the United States).
The H1N1 virus is taking over as the dominant type of influenza virus in most parts of the world; recent monitoring in the United States shows that influenza activity for September is already much higher than usual in 21 states. It is clear that our “flu” season has started, and the strains isolated are virtually all H1N1.
The epidemiology of case characteristics with this pandemic is different than seasonal influenza, and similar to the pattern of the 1918 pandemic. Most of the cases (70%) are in persons between the ages of 5 and 65 years, with predominance in school-age kids and young adults. Older persons appear to enjoy some residual natural immunity from previous experience with an H1N1 strain of influenza. Although healthy elderly persons may have some natural protection, the CDC still lists residents of long-term care and assisted living facilities as high risk, and they are high priority for early vaccination and aggressive antiviral therapy if infected. Other high-risk groups include pregnant women, immune-suppressed/compromised persons, those with pulmonary diseases such as asthma, chronic obstructive pulmonary disease, tuberculosis, diabetes, or major organ failure. They are the most likely to have severe complicated illness and increased mortality risk similar to seasonal influenza. However, 41% of the fatalities have been in young and otherwise healthy individuals, and severe obesity also appears to be a risk factor for complicated illness that is unique to this pandemic. Severe disease in persons who do not have other apparent risk factors appears to be due to an overreaction of the individual’s immune system to the virus (“cytokine storm”), resulting in a severe hemorrhagic pneumonitis and pulmonary failure.
Clinical Management
The clinical pattern of H1N1 influenza, to date, has been very similar in most cases to seasonal influenza, and for the vast majority of individuals affected, the course of illness will be benign and require symptomatic and supportive treatment only. Initial symptoms are usually respiratory (ie, cough, sore throat, rhinorrhea), but often include other common symptoms of influenza illness such as fever, chills, myalgias, headache, nausea, vomiting, diarrhea, and fatigue. For most, the treatment will be minor analgesics, antipyretics and fluids, and relative quarantine to avoid exposure to others. Individuals are considered infectious from 1 day before onset of symptoms until at least 24 hours after their fever subsides. The transmission of the disease is largely by droplet infection, so infected individuals should cover their nose and mouth when coughing or sneezing. Handwashing with a germicidal agent, especially after coughing or sneezing, may also help to avoid contaminating objects since the virus can survive up to several hours on an inanimate surface. Infection rates of close household contacts are about 18-21%, so it helps if the ill person can stay confined to a separate area of the home and wear a mask when in common space with other family members. Healthcare workers or caregivers of persons requiring nebulizer or ventilation treatments should wear the fitted N95 masks since those types of treatments can aerosolize viral particles and increase risk of infection.
Home care of high-risk persons is somewhat more involved and starts with vaccination (if possible) of all high-risk persons and their close contacts before exposure. Most persons with a competent immune system should have protection from the present strain of H1N1 virus within 8 days of a single vaccine dose. High-risk persons who come down with influenza-like symptoms should be immediately started on an antiviral medication that is effective against the H1N1 virus (oseltamivir or zanamivir), and if a close contact of a high-risk person becomes sick with an influenza-like illness, the high-risk individual should be started on a prophylactic course of medication that continues for 10 days after the last exposure. Since early initiation of medication in the course of illness affords much better benefit, some consideration should be given to providing the high-risk patient with a prescription in advance of any illness that could be filled should symptoms develop. The delay in treatment that might occur in scheduling a doctor’s visit when health systems are overloaded could compromise the patient’s recovery. To date, 100% of persons who have had serious cases of H1N1 influenza requiring hospitalization had fever (> 38 degrees C or > 100.4 degrees F), cough, and dyspnea. If persons have that triad of symptoms, they should seek medical care. Some severe cases also had gastrointestinal symptoms (nausea, vomiting, and diarrhea) with complications of dehydration.
As with seasonal influenza, residents of long-term care and assisted living facilities present a special challenge in managing their care in this H1N1 pandemic. This is a high-risk group of persons living together, sharing meals, activities, caregivers, and most with regular contact with outside family members. Vaccination of staff has been shown to reduce cases of influenza in residents, hospitalization, and mortality, so this is a very high priority.1,2 However, when a close contact of a resident (staff, another resident, or family visitor) develops active disease, chemoprophylaxis as decribed above should be intiated. In the heat of the pandemic, it is very likely that persons hospitalized for acute illness may be transferred to these facilities for post-acute care. Space and staffing shortages as descibed below could make it very difficult to segregate influenza-afflicted residents from others, and high resident-to-staff care ratios may challenge good infection control practices. Medical directors and directors of nursing should review and update their plans for infectious disease outbreaks in their facility, with special attention to monitoring exposures and antiviral treatment and chemoprophylaxis protocols. A comprehensive planning checklist for pandemic preparation for long-term and residential care administrators and directors is available at the www.flu.gov website.
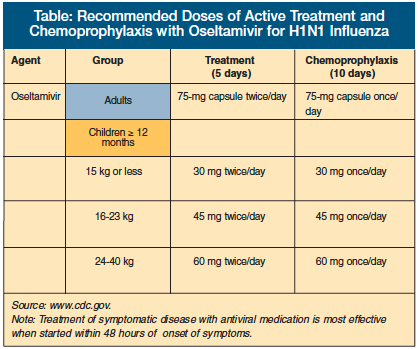
The Table provides the recommended doses for active treatment and chemoprophylaxis with the neuraminidase inhibitor oseltamivir for H1N1 influenza. The antiviral agents amantadine and rimantadine are not effective against the H1N1 virus but still may be needed in situations where both seasonal influenza and H1N1 co-exist. Seasonal influenza has considerable resistance to the neuraminidase inhibitors. At present, the predominant viral influenza experience in the United States is overwhelmingly the H1N1 strain, but physicians must keep aware of influenza patterns in their communities and institutions since effective medication regimens may change depending on the dominant strain or the development of resistant strains. In general, zanamivir is not recommended in persons with underlying respiratory diseases such as asthma or chronic obstructive pulmonary disease. WHO is recommending starting with oseltamivir when initiating treatment, and it is discouraging the use of chemoprophylaxis because of concerns about development of resistant viral strains. The CDC, however, does recommend chemoprophylaxis for healthcare workers and individuals who are actively caring for persons with severe H1N1 disease, and to continue for at least 10 days after exposure.
Public Health Strategies
Public health measures are critical for optimal management of the pandemic, and they will be especially important in poorer countries that have limited healthcare resources. They begin with basic avoidance of contact with infected persons. Persons with influenza-like illness or symptoms are urged to stay home from work, school, and other public places until at least 24 hours after the last fever. If it is necessary to go out in public, the person should wear a mask and cover his or her mouth and nose when coughing or sneezing. It is estimated that school closings early in the outbreak of H1N1 influenza in a community could reduce the spread of disease by 30-50%. Good handwashing practices have been shown to reduce infection rates by 41%, and similar reductions can be seen with disposable masks. A study from the United Kingdom showed that alcohol-based hand-cleansing products are effective germicidals, but the protection is gone within a few minutes as soon as the alcohol evaporates.3 A germicidal foam lotion product, however, that leaves a residual film on the skin was effective protection for up to 3 hours. For persons in a high-exposure situation, the longer-lasting germicide is preferable. The high efficiency N95 fitted masks reduce infection rates by 91%, which is comparable to glove, gown, and mask isolation procedures in hospitals. The N95 mask is somewhat difficult to wear and breathe through for long periods, but it is the best protection for persons who cannot avoid exposure.
The successful development of a 1-dose vaccine has been a major breakthrough in the management of this pandemic. High-risk persons and healthcare personnel will be the first priority in targeting the initial vaccination efforts. Production capacity by manufacturers may limit mass immunization programs initially, but it is expected that vaccine will be available for most people in the United States within the next few months. Persons with egg allergy and persons who have had a bad reaction to influenza vaccine in the past should not be vaccinated, but everyone else should be encouraged to get vaccinated for their own personal health, as well as that of the public. Unfortunately, many poorer countries of the world cannot afford vaccines and will have to rely more on avoidance measures. However, WHO is sponsoring a program of vaccine donation from wealthier nations that will be distributed by WHO to countries in need.
Health System Preparedness
The part of the pandemic that may be most difficult to anticipate is the adequacy of response of health systems to the fluctuations in disease burden. With the forecast of up to 2 billion cases of H1N1 influenza in the next year or two, healthcare systems will experience something between a stressful overload to an overwhelming tsunami of disease burden that could result in excessive morbidity and mortality. A projection of health system needs in the United Kingdom anticipated a greater need of intensive care unit beds than are available and a much greater need of pediatric intensive care. Fortunately, planners have been working on this problem for several years since the concern about an avian H5N1 influenza pandemic arose. A generic template of preparation based on the “4 S’s” (system, staff, stuff, and space) has been devised:
System: It is important to have a system-wide overview of the capacity to respond to increased demand in order to anticipate bottlenecks in patient care. The system must not only have adequate intensive care facilities, but also step-down care plans to move patients expeditiously to less intensive settings. Post-acute care, home care, and nursing home care settings should prepare to increase the acuity of services offered (infusion therapies, assisted ventilation, etc.) to accommodate decongestion of hospital beds. Staff: Staffing is critical both in adequacy of numbers and competency. The template calls for a designated staff leader who is not inundated with clinical responsibilities, whose main responsibility is to provide monitoring and oversight of staffing needs. Recent experience with this pandemic has demonstrated that staff shortages are likely. This is because of increased care system demands, but also because some staff will be sick, caregiving at home, or may refuse to work in a high-exposure setting. Staff will also need review of infection control procedures and special precautions in caring for influenza patients. Shortages of intensive care nursing staff (especially pediatric) and respiratory therapists are likely, and the staffing leader may need to cross-train staff from other departments (emergency, anesthesia) to be available as back-up.
Stuff: This “S” pertains to the supplies and equipment needed to function effectively in a crisis. Disposable and durable respiratory supplies may be in short supply nationwide, and a plan to anticipate shortages should include some advance stocking, equipment testing and maintenance, and inventory of other possible sources for back-up or resupply (eg, intubation equipment, ventilators in emergency dept or anesthesia).
Space: Space will be the most challenging problem for many health care systems and may present ethical dilemmas as well as care problems. To anticipate the space problem, care systems should develop a step-down plan of care to move patients expeditiously to non-intensive and post-acute care settings. Even though entities within a community care system may be owned and operated by separate, even competing, organizations and businesses, advance discussions regarding coordination of resources in a crisis, space use, diversion of patients to most appropriate settings is recommended. In the event that a hospital or intensive care department is full, the decision to further allocate limited resources should fall to a designated triage officer or team. It is recommended that an a priori triage protocol based on prognosis, comorbidities, and age be adopted in advance to make this process rational and objective.
(For a more detailed review of this plan, see the supplement to the Chest journal.4)
Conclusions
Although the H1N1 pandemic has been relatively benign and manageable to date, WHO and other public health officials remain cautious in their predictions. There is always concern that the virus may mutate in a way that would make the disease more severe or medications and vaccines less effective. An additional concern is that a public apathy may develop. Persons may decide that this is not much of a personal threat and disregard basic public health measures and vaccination recommendations that are so important in pandemic containment, relying on the fact that there is an effective drug to take should they become seriously sick. It is an ongoing task of healthcare providers to stay apprised of clinical developments in the H1N1 pandemic that may change patient care recommendations, and to continue to advise our patients of the public health importance of vaccination and avoidance of exposure.
Dr. Keenan is a retired professor from the Department of Family medicine, University of Minnesota, Minneapolis.









