Beyond Bingo: Meaningful Activities for Persons with Dementia in Nursing Homes
Introduction
The importance of redesigning nursing homes to better emulate living in one’s own home has driven regulation reform for decades. The early focus of addressing residents’ rights in the Nursing Home Reform Act1 has slowly expanded to a broader vision of creating “a culture of aging that is life affirming, satisfying, humane and meaningful.”2 Commonly called “culture change,” the movement to improve quality of life among older adults in nursing facilities and other long-term care (LTC) settings has gained considerable momentum.
The primary advocacy group, the Pioneer Network, emphasizes values such as knowing the person, putting the person before the task, emphasizing self-determination, promoting growth and development, and using the environment to its best potential.2 Many of these values are exemplified in the revisions of activities regulations set forth by the Centers for Medicare & Medicaid Services (CMS) in 2006. According to 483.15 (f)(1), “The facility must provide for an ongoing program of activities designed to meet, in accordance with the comprehensive assessment, the interests and the physical, mental, and psychosocial well-being of each resident.”3
This seemingly simple requirement is strengthened and expanded by definitions that characterize activities as enhancing well-being and promoting physical, cognitive, and emotional health, such as self-esteem, pleasure, comfort, creativity, success, and independence. An additional emphasis is placed on “person-appropriate” activities that are relevant to the specific needs, interests, culture, and background of individual residents, including those with dementia. “One-to-one programming” requires that caregivers provide assistance for those who cannot plan their own activity pursuits, or need special assistance, such as those with dementia.
Finally, the program of activities is defined as being a combination of large- and small-group, one-to-one, and self-directed activities that occur throughout the day, every day of the week. The investigative protocol that accompanies the rule reinforces the need for activities to be an ongoing program that is implemented throughout the day, one that is composed of activities that are compatible with the resident’s known interests, needs, abilities, and preferences, and that is implemented in an environment that promotes success.3
To determine compliance with the rule, residents, activity staff, nurses, nursing assistants, and social workers are all interviewed to determine whether the individual resident’s preferences and choices are assessed, activities are implemented in accordance with needs and goals, resident-specific outcomes are monitored and evaluated, and approaches are revised as appropriate.3 The proverbial “bottom line” in the activity revision is that the large-group programs that dominate activity calendars on a Monday-through-Friday basis are insufficient. The rule simultaneously calls for activities that are person-directed and for collaboration among team members to assure that meaningful activities are continuously available to residents. Language specific to persons with dementia emphasizes the important role that staff may need to play in identifying enjoyable activities that are consistent with the person’s level of current functioning, as well as implementing, monitoring, evaluating, and revising plans of care to ensure that needs and preferences are best met.
Training to Promote Activity Involvement
For many “pioneers” of culture change, the rule is an exciting opportunity. For others, the requirement is greeted with the same unenthusiastic response that has echoed throughout Nursing Home Reform: “More rules without any additional funding to make needed changes.” No matter which viewpoint one takes, the rule is in effect and will likely be a focus of compliance in future reviews. Just as facilities needed training to reduce physical and pharmacological restraints in the 1980s, many LTC settings currently need assistance to better understand viable activity options that promote the dual mission of quality of life for residents and regulatory compliance. In particular, training related to the needs of persons with dementia may be especially acute given disease-related deficits that interfere with communication, problem-solving, and initiation of activities.
As a result, a group of researchers collaborated to develop an innovative, self-directed CD-based training program, Dementia Training to Promote Involvement in Meaningful Activities (Table I). Information on which the training program is based was presented in a workshop entitled “Beyond Bingo and Painted Nails: Meaningful Activity for Persons with Dementia” at the American Association for Geriatric Psychiatry Annual Conference in March 2008. Underlying principles presented at the symposium and contained in the training CD are briefly reviewed in this article.

Activities in Dementia Care
An important first step in modifying activity programs for persons with dementia is to understand how dementia-related changes may influence the approaches required to meet activity needs and preferences. Important background information includes understanding cognitive losses that characterize dementia, such as expressing interests (eg, aphasia), identifying and planning activities (eg, executive function), and remembering how to do activities (eg, memory loss, agnosia). In addition, understanding the relationship between behavioral and psychological symptoms of dementia (BPSD) and unmet activity needs is equally, if not more, important for daily care providers.
Theory-Driven Activity Involvement
The Need-Driven Dementia-Compromised Behavior (NDB) model of dementia care4,5 provides an important framework for understanding how caregivers can adjust daily routines to reduce the risk of BPSD and promote comfort, function, and enjoyment in living. The NDB model suggests that BPSD are the direct result of both background factors that are fairly stable (eg, neurological factors, cognitive abilities, health status including physical functional abilities, psychosocial factors including premorbid personality) and more changeable proximal factors (eg, physiological and psychological need states, qualities of the physical and social environments).
The interplay between background and proximal factors produces need-driven behavior, the most integrated response a person can make given the limitations imposed by the dementia, strengths preserved from abilities and premorbid personality, and the constraints or supports offered by the environment. In the NDB model, background factors represent a profile of strengths, weaknesses, and usual coping style, and this information is used to individualize activities by tailoring them to these personal characteristics.
Recreational activities that are individually tailored to background factors appropriately enrich the physical and social environment (proximal factors) because they meet individual needs. NDB-derived activities match the resident’s current level of cognitive and physical functioning abilities, so that they are at an appropriate level and afford the opportunity for participation. Activities also match the resident’s style of interest—his/her personality—so that they provide preferred amounts of social stimulation and novelty, thereby capturing interest. Examining the “match” of abilities and interests (background factors) to the type, duration, and timing of activities (proximal factors) provides important framework for daily care providers.
The efficacy of recreational therapies derived from the NDB model was tested in 30 nursing home residents with moderate-to-severe cognitive impairments.6 Older adults in the sample were primarily female (77%), with a mean age of 82.3 (standard deviation [SD] = 7.5) years and Mini-Mental State Examination (MMSE) score of 8.6 (SD = 7.2). Subjects were randomly assigned to 1 of 6 possible order-of-condition presentations in a crossover experimental design with repeated measures of time on task, level of participation, affect, agitation, and passivity. Three conditions tested included: (1) activities matched to skill level only; (2) activities matched to interests only; and (3) the NDB-derived condition in which activities were matched to both skill level and interests. Findings indicated that significantly more time on task, greater participation, more positive affect, and less passivity occurred under the NDB-derived condition as compared to skill-level-only treatment and baseline levels. Agitation and negative affect improved under all treatments as compared to baseline,6 suggesting that activity involvement is superior to “usual care.”
Application in Practice
The NDB model suggests that the type and frequency of activities in which the person with dementia is engaged are highly relevant to the occurrence of BPSD. In too many instances, people with dementia are left alone, often with nothing to do. The losses that are a part of dementia—such as using language to explain needs or to plan their day—interfere with their engagement in preferred and meaningful activities. Too often, they wander aimlessly out of boredom, cry out for company or comfort, or sit alone, disengaged from human and environmental interaction.
Large-group activities that are often the focus of nursing home care are either too complex or stimulating for their level of function, have little in common with their current or long-standing interests, or are simply too long to be tolerated. The NDB model refocuses caregivers, asking that they think about the person’s background factors, the things that are reasonably stable. For example, understanding the extent of their cognitive impairment and retained abilities, physical limitations that are the result of their health problems that may influence activity choices, and long-standing personality traits and activity preferences/interests are all important considerations in devising a person-appropriate activity plan. Similarly, proximal factors are equally important. For example, the person’s level of physical and psychological comfort, and things that are going on—or perhaps not going on—in the physical and social environment clearly relate to activity involvement for those with dementia. In order to make activities person-appropriate for those with dementia, caregivers need to know the person well.
As outlined in Table II, several important factors interact and need to be considered in selecting individualized activities for persons with dementia: the person’s activity interests and preferences, cognitive level, physical abilities and/or limitations, any psychiatric problems or symptoms that might influence outcomes, communication abilities, and biological rhythms that may help caregivers time activities to be maximally beneficial.

Activity Options: Many Choices
In addition to knowing the person well, many caregivers need assistance to think more creatively about activity options for persons with dementia. Of note, an increasing body of research evidence supports the use of diverse recreational therapy interventions with persons with dementia. In specific, the NEST (Needs, Environment, Stimulation, and Technique) approach described by Buettner and Fitzsimmons7 provides substantial support with over 80 therapeutic protocols that fall into 10 categories, such as feelings (eg, Memory Tea), nurturing (eg, Animal-Assisted Therapy), relaxation (eg, Guided Imagery), adventure (eg, Wheelchair Biking), physical exercise (eg, Early Risers Walking Club), cognitive (eg, The Price Is Right Game), life roles (eg, Therapeutic Cooking), psychosocial clubs (eg, Jewelry Club), and Simple Pleasures (eg, Wave Machine).
As Buettner and Fitzsimmons emphasize, these strategies were developed and tested as recreational therapy interventions aimed at reducing identified BPSD8 and are optimally used by dedicated teams in LTC settings. The NEST approach recommends developing LTC staff teams composed minimally of a nurse and recreational therapist, along with representatives from other departments, who meet daily to address the needs of persons with dementia.7 These teams collaborate to fully assess behaviors, address unmet needs, adapt the environment to promote function, complete baseline assessments (as outlined in Table II), and select activity protocols based on the individual. Activity-oriented approaches may also be incorporated into more generalized “total unit” or milieu therapy programs for persons with dementia, and used as health promotion/BPSD prevention methods that are designed to reduce the overall risk of distress and discomfort by engaging older adults in meaningful activities.9
The examples described below were developed and tested by Buettner and Fitzsimmons7 and are described in detail in their NEST manual. Research evidence to support the effectiveness of these interventions and details related to the implementation steps are described elsewhere in the literature.5,6,10-17 Key outcomes associated with the use of therapeutic recreation interventions with older adults with dementia include the following: significant improvements in calming individuals with agitation (92-100% of the time) and alerting persons with passive behaviors (79-91% of the time)16; successful engagement of persons with dementia (eg, interested in and focused on the activity, positive affect and mood, minimal or no suspiciousness, agitation or restlessness, or frustration) in preferred small-group activities17; significantly higher levels of participation, time on task, positive affect, and less passivity6; and significantly decreased depression and improved sleep, and activity and engagement.15
Simple Pleasures
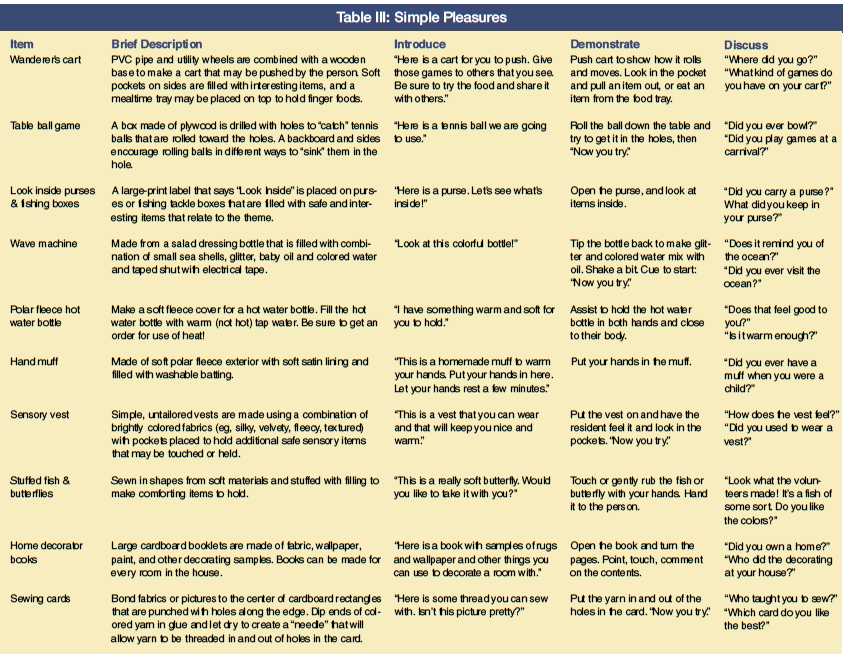
A group of multilevel sensorimotor interventions called Simple Pleasures18 offers an important starting point for devising activities that may be used by nonactivity personnel throughout the day. These interventions were developed and tested for persons with dementia in LTC settings and, by design, enhance opportunities for self-initiated activities and social interaction. Simple Pleasures items may be used for several purposes, such as passive behaviors (eg, sitting without active engagement with the environment or others), boredom (eg, behavior that suggests a craving for things to touch or interact with), or agitation (eg, restlessness, wandering, physically or verbally nonaggressive behaviors).
The “pleasure” derived from the item is observable in the amount of time spent on task, affective responses, and behaviors; for example, these may include alerting and engaging those who are passively sitting or, in contrast, distracting and calming those who may be escalating into more agitated behaviors. The activities are designed to be used one-to-one or in small groups of no more than five people. Length of the intervention ranges from 5-45 minutes, depending on the attention span of the person and his/her level of interest in the item. All items have been tested for safety and may be crafted by volunteers following directions that are provided free of charge online. Selected Simple Pleasures items are described in Table III.

Adventure-Based
Wheelchair Biking offers considerable opportunities for persons with dementia by combining small-group activities with rides on a Duet bike.7 Small-group discussions focus on past experiences with riding a bike. Discussion cues include, “How old were you when you first rode a bicycle? Do you remember what color it was?” and other prompts related to earlier experiences with riding bikes. The Duet bike has two parts: a wheelchair and a bike that is specially designed to fit the wheelchair, enabling the older adult to “ride” while an appropriately trained person (recreation therapist or his/her designee) peddles the bike. In the Wheelchair Biking protocol, short rides of 10-15 minutes are provided to participants. After the ride, participants tell others in the group about their ride.15 Although the investment to obtain this specialized bike is a consideration, many facilities successfully fundraise around the program and the opportunities it provides.
Life Roles
Therapeutic Cooking offers a familiar, family-like intervention that may simultaneously stimulate cognition skills, improve motor function (fine and gross, depending on the activity), and reduce anorexia.16,19 Cooking activities may involve different levels of engagement, such as planning menus, assembling food required by a particular recipe, using adapted equipment to prepare food (eg, using an apple peeler to prepare pie), stirring batter or placing dough on trays, preparing finger foods (eg, putting cherry tomatoes on decorative, plastic serving “trees”), and enjoying baked or prepared items in a group. Cooking may be combined with other activities, such as gardening in raised beds, setting or decorating the table, and, importantly, socialization related to past experiences and current interests.
Physical-Based Engaging persons with dementia in various types of physical exercises and activities is associated with improved sleep, function, and mood, as well as reduced restlessness and wandering. For example, Exercise for Function7 is a structured physical activity that combines range of motion (eg, head rotation, shoulder shrugs, knee lifts) with strengthening (eg, water jug lifts) and endurance (eg, tethered balloon ball) activities. A 20-minute exercise routine is choreographed to familiar music, with exercises moving from head to feet under the guidance of a therapist and used three times per week as a small-group intervention (eg, 3-5 residents).7 An alternative program engages early risers who are at risk for unsafe behaviors such as wandering, falling, or agitation. The Early Risers Walking Club7 is conducted 30 minutes a day, five days a week, starting at 7:00 AM. These morning walks are individualized and graded to increase as endurance levels improve.7
Cognitive-Based
The Price Is Right Game7 may be used for several purposes: cognitive stimulation related to guessing prices; appetite stimulation related to thinking about food; socialization, as foods and prices are discussed; and as a means to engage residents who tend to wander away from the dining room before meals are served. During the small-group intervention, a therapist introduces empty food containers as though they have just come from the grocery store. Two food items are held up, and residents are asked, “Which one do you think costs more?” After each guess, residents are shown the actual price (marked on the bottom of the item) and engaged in brief discussion (eg, “Do you think that is a fair price? What do you make with [name of item]?”). Another cognitive-based program is to play Dominoes,7 using regular or large dominoes, or picture dominoes as outlined in Simple Pleasures. Dominoes may be played according to rules with higher-functioning residents, while building structures or setting dominoes on edge in a line to be toppled may be preferred by mid-functioning residents. Lower-functioning residents benefit from color-matched dominoes or those with large wooden pictures.
Psychosocial Club–Based
A wide variety of “club-based” activities may be developed to address topics of interest: birds, bowling, cars, golfing, weather, needlecrafts, and fashion, among others.7 Club-based programs engage residents in small-group socialization, discussion, and activity engagement around the club theme, and are used to reduce depression, social isolation, passivity, sensory deprivation, restlessness, and wandering. Meetings are held once or twice per week for 30-45 minutes (depending on the club and its specific activities) and are led by a recreational therapist, nurse, or other healthcare professional. For example, Jewelry Club members are given a jewelry box filled with costume jewelry to sort through, rearrange, organize, or try on. Discussion cues are used to enhance socialization and interaction (eg, “Did you have a locket? Whose picture did you keep in it?”). As with all protocols, involvement in club-based activities is guided by residents’ individualized interests and preferences.
Nurturing
Another important group of interventions engages residents in caring or nurturing behaviors. Animal-assisted methods, including both Animal-Assisted Activities (AAAs) and Animal-Assisted Therapy (AAT), may contribute to well-being among residents but have different goals.7 Animal-Assisted Activities may be conducted by volunteers and largely involve visiting interested residents who enjoy animals (or the specific type of pet visitor). The exchange may have social, motivational, educational, or recreational benefits20 but does target a specific outcome and is not documented as a part of the person’s care. In contrast, AAT is directed by a healthcare professional, interactions with animals have specific therapeutic goals, and outcomes of the intervention are documented in the resident’s chart.
Each AAT visit involves three main components: (1) the approach, in which visual and verbal contact is made between the animal and resident, and the resident is invited to work with the animal; (2) the process, in which the animal-resident interaction is focused on meeting identified therapeutic goals; and (3) the closure, in which the resident rewards the animal, accomplishments are reviewed, the next session is planned, and goodbyes are said.7 Therapy animals are commonly provided by pet-handler teams, such as those registered by the Delta Society Pet Partners program.20 Potential benefits of AAT include increased communication, better attention to task, and improved self-esteem, confidence, and mood,20 as well as increased motivation and/or calming effects and reduced loneliness.7
Teamwork: Making It Work
As recommended in the NEST approach, collaboration among disciplines is essential for activity programs and therapies to be successful. The importance of collaboration is underscored by the CMS rules and investigative protocols that interview nurses, nursing assistants, and social workers, as well as activity directors and their staff. Although a wide variety of factors interact to determine outcomes of care, experience and research suggest that successful programs regularly have the full support of the facility administration to form a team, include key staff from all available disciplines to participate in the team, identify a leader who is knowledgeable about dementia and activity involvement, meet on a regular basis, and communicate well with others. Success also relies on building on the strengths of team members.
As activity methods and processes are put in place, the discipline of the team member is less important than the person’s interests and skills. For example, a nurse who is a coin collector may be the ideal person to lead the Coin Collector’s Club; a nursing assistant who plays guitar and sings might organize an evening sing-along; or a social worker who is an early-morning person may be ideally suited to escort the Early Risers Walking Club. Building on staff members’ natural interests and skills is essential to developing and sustaining programs. Other aspects of teamwork involve helping all staff members appreciate and assist with common aspects of activity involvement, such as helping residents be appropriately dressed and outfitted for the program. For example, wearing sturdy and well-fitting shoes for walking or wearing sunglasses and sunscreen for outdoor activities may be pivotal in the overall success of the program.
Staff collaboration also extends to resolving “competing demands” for residents’ time—such as adjusting medication schedules to best accommodate activities (eg, giving as-needed pain medications before or after the activity, adjusting timing to enable full participation), or making appointments to avoid conflicts with scheduled small-group activities. Another important aspect of teamwork is helping daily staff providers gain needed skills to successfully facilitate activity programs. Although recreation and activity personnel may be available during “business hours” (eg, 9:00 AM to 5:00 PM, Monday through Friday), both scheduled and “as-needed” programs may be needed at all hours of the day, every day of the week.
This issue is specifically addressed in the CMS discussion of Care Planning, which notes that activities may occur at any time and are not limited to formal programs provided by activity staff, and that all relevant departments should collaborate to develop and implement an individualized activity program for each resident.3 For example, nursing personnel may benefit from understanding the importance of and strategies for transitioning residents from one activity to another (eg, using the Price Is Right Game before meals, using a Simple Pleasures butterfly to engage a restless resident during personal care). Staff members may also need guidance and assistance to ensure that the residents, not the staff members, conduct the activity. For example, teaching staff caregivers to cue residents to start, demonstrating without “doing” the activity for the person, and providing verbal prompts without dominating conversations is important to activity success.
Summary
The 2006 activity revision provides important opportunities to advance the value of culture change in LTC settings. Developing and maintaining successful, person-appropriate activity programs for individuals with dementia relies on the cooperation and assistance of all team members, a basic working knowledge of dementia processes, and a sound knowledge of innovative, evidence-based activities that are matched to the interests and abilities of individual residents. Ongoing training and education of LTC staff, including but not limited to programs like the NEST and the CD-based Dementia Training programs, is a necessary first step in building facility-based, interdisciplinary teams that share responsibility for ensuring ongoing involvement in person-appropriate, meaningful activities for residents with dementia.
Acknowledgment
Content in this article was first presented by the authors as a workshop at the American Association for Geriatric Psychiatry Annual Conference, March 14, 2008, and is based on a CD-based training program funded by the Retirement Research Foundation, Chicago, IL. Dr. Buckwalter received grant support from Retirement Research Foundation (RRF), Dr. Smith received grant support from RRF and Wellmark Foundation, Dr. Buettner received grant support from RRF, the Alzheimer’s Association, and Florida Elder Affairs, and Dr. Kolanowski received grant support from the NINR: R01 NR 008910.
The authors report no relevant financial relationships. Dr. Smith is Assistant Professor and Dr. Buckwalter is Sally Mathis Hartwig Professor of Nursing, University of Iowa College of Nursing, Iowa City; Dr. Kolanowski is Elouise Ross Eberly Professor of Nursing, Penn State University, University Park; and Dr. Buettner is Professor of Therapeutic Recreation and Gerontology, University of North Carolina at Greensboro.










