ARMOR: A Tool to Evaluate Polypharmacy in Elderly Persons
Background
Polypharmacy is a common problem encountered by clinicians caring for elderly.1 It is encountered in all care settings ranging from outpatient to long-term care (LTC), where it is particularly linked with falls and other associated problems.2 Polypharmacy refers to the use of multiple medications by a patient. The term is used when too many forms of medication are used by a patient, more drugs are prescribed than clinically warranted,3 or even when all prescribed medications are clinically indicated, but there are too many to take (“pill burden”). This has a potential to cause higher adverse drug reactions (ADRs) and drug-drug interactions (DDIs).
The financial impact of polypharmacy-related problems translates into a significant cost to the health system, and it has a financial bearing on patients as well as institutions.4,5 Redundancy and duplication of medications are common. Regulatory issues, particularly in LTC settings, also can influence prescribing patterns.
Lack of proper indications, inappropriate dosage, and subclinical toxicities of medications are common observations. “Prescribing cascade” is a known problem, where a medication results in an adverse drug event (ADE) that is mistaken as a separate diagnosis and treated with more medications, which puts the patient at risk for additional ADEs.6 Polypharmacy takes its own toll on limited physiological and financial reserves. It is common to see nine or more medications prescribed to elderly patients transferred for subacute rehabilitation from hospitals to nursing homes. These medications are prescribed by multiple providers at different times for different reasons. One such common example is medications started for a patient during a hospital stay by consultants and hospitalists that are not re-evaluated for appropriateness after discharge from the hospital by the physician in charge of care of that patient.
Some current strategies available to address this complex issue include “START” (Screening Tool to Alert doctors to the Right Treatment) and “STOPP” (Screening Tool of Older Person’s potentially inappropriate Prescriptions) criteria. START is an effort to help prevent omission of important appropriate medications and is organized by organ system.7 STOPP criteria are a useful guide to identify potentially inappropriate medications (PIMs), particularly in the hospital setting.8
In addition, a multidisciplinary expert panel recently developed a consensus agreement on a list of laboratory findings and medication combinations to help detect potential ADRs in nursing home residents.9 Zhan et al10 published modified Beers Criteria to develop a list of potentially harmful medications in community-dwelling elderly persons. A cross-sectional database study identified older patients receiving medications included in the Health plan Employer Data and Information Set (HEDIS 2006) criteria, using national data from Veterans Affairs.11 The HEDIS 2006 criteria was derived from the medications thought to be the most problematic in the elderly. Results for the HEDIS 2006 measure were similar to those of the 1997 Beers Criteria.12
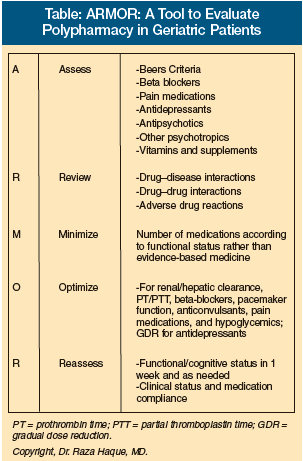
The ARMOR Tool
The ARMOR tool (Assess, Review, Minimize, Optimize, Reassess) is an attempt to consolidate these recommendations into a functional and interactive tool. It takes into account the patient's clinical profile and functional status, and tries to balance evidence-based practice with altered physiological reserves.13 ARMOR is an effort to approach polypharmacy in a systematic and organized fashion. Functional status, its restoration, and maintenance are the primary outcome goals. This tool also emphasizes quality of life as a key factor for making decisions on changing or discontinuing medications. Use of a certain medication is weighed against its impact on primary biological functions such as bladder, bowel, and appetite. Functional status and mobility is held up as the essential final outcome measure for any medication change using ARMOR.
Implementation of ARMOR
We used ARMOR in a LTC facility with an interdisciplinary team–based approach. Each patient and his/her chart was reviewed to provide recommendations on a monthly basis to all clinicians on appropriate dosing, potential ADRs, and regulatory guidelines mandated by state and federal compliance rules. We invited consultant pharmacists to join the interdisciplinary team to discuss each recommendation made, and to discuss our care plan with reference to our goals for a particular patient. Pharmacists were involved in changes being considered for further input if deemed necessary. In cases where a difference of opinion arose, all team members deliberated, with function and cognition as primary outcomes for guidance.
 The team consisted of a medical director, director of nursing, assistant director of nursing, physical/occupational therapy director, recreational therapist, and social worker. Each member reported on his/her subjective observations of function, behaviors, and cognitive status. The nursing director is responsible for contacting clinicians for implementing the proposed changes. The medical director meets with clinicians once in a quarter to discuss clinical impact or concerns regarding the recommendations. Clinicians are encouraged to adopt the proposed recommendations. Patients who are discussed in the team meeting include all new admissions for subacute geriatric rehabilitation, as well as those with frequent falls and behaviors. We recommend the use of ARMOR in comprehensive geriatric assessments and outpatient settings as well; it is also useful in monitoring and optimizing outpatient prescribing patterns.
The team consisted of a medical director, director of nursing, assistant director of nursing, physical/occupational therapy director, recreational therapist, and social worker. Each member reported on his/her subjective observations of function, behaviors, and cognitive status. The nursing director is responsible for contacting clinicians for implementing the proposed changes. The medical director meets with clinicians once in a quarter to discuss clinical impact or concerns regarding the recommendations. Clinicians are encouraged to adopt the proposed recommendations. Patients who are discussed in the team meeting include all new admissions for subacute geriatric rehabilitation, as well as those with frequent falls and behaviors. We recommend the use of ARMOR in comprehensive geriatric assessments and outpatient settings as well; it is also useful in monitoring and optimizing outpatient prescribing patterns.
The application of this tool has led to significant reduction in polypharmacy, reduced cost of care, and marked decrease in hospitalization at our facility. Falls and behaviors with potential of harm to self and other residents also showed a decline in frequency. Similar impact was seen in usage of psychotropic medications. The internal quality indicators (QIs) used by the facility further substantiated this trend.
ARMOR is a stepwise approach for assessment of a geriatric patient who is: (1) receiving nine or more medications; (2) seen for initial assessment; (3) seen for falls and/or behaviors; and/or (4) admitted for rehabilitation. The clinician first obtains heart rate, blood pressure (postural), and oxygen saturation rate at rest and with activity. A physician assessment and physical examination is followed by the following steps:
Step 1: A = ASSESS the individual for total number of medications and for certain groups of medications that have potential for adverse outcome:
• Beta blockers
• Antidepressants
• Antipsychotics
• Other psychotropics
• Pain medications
• Other medications listed in the Beers Criteria12
• Vitamins and supplements
Step 2: R = REVIEW for possible
• Drug-drug interactions.
• Drug-disease interactions.
• Drug-body interactions (pharmacodynamics).
• Impact on functional status (Timed Get Up and Go test).
• Subclinical ADRs.
• Weigh individual medication benefits against primary body functions (appetite, weight, pain, mood, vision, hearing, bladder, bowel, skin, swallowing, activity level).
Step 3: M = MINIMIZE nonessential medications:
• Eliminate medications that clearly lack evidence for their usage.
• Eliminate medications whose risks outweigh benefits and that have high potential for negative impact on primary functions (appetite, weight, pain, mood, vision, hearing, bladder, bowel, skin, swallowing, activity level).
Step 4: O = OPTIMIZE by addressing
• Duplication.
• Redundancy.
• Adjust renally cleared medications to creatinine clearance (glomerular filtration rate).14
• Adjust medications that are metabolized in liver for clearance.15
• Adjust oral hypoglycemics to blood sugar target and HbA1c.
• Consider gradual dose reduction (GDR) for antidepressants.
• Adjust beta blockers to allow physiological heart rate response.16
• Adjust beta blocker dose for pacemakers.
• Adjust anticoagulants for international normalized ratio (INR) guidelines and possible DDIs.
• Adjust seizure medications with free phenytoin level.
Step 5: R = REASSESS heart rate, blood pressure (postural), oxygen saturation rate (> 92%) at REST and ACTIVITY. Also reassess
• Functional status17 (Timed Get Up and Go test, activities of daily living [ADL] and instrumental activities of daily living [IADL] from Minimum Data Set).
• Cognitive status (Folstein Mini-Mental State Examination).
• Clinical status (clinical exam by physician for compensation of pre-existing diseases).
• Medication compliance (medication errors in the case of LTC).
Discussion
We have been using ARMOR for the following: subacute geriatric rehabilitation, outpatient comprehensive geriatric assessment, evaluation of multiple falls, behavior assessment in LTC, evaluation of delirium, GDR in LTC, and unexplained functional decline in LTC.
Our experience has shown a clear and consistent decline in the use of nine or more medications on our QIs for the past 6 months, compared to state and national averages (noted from Minimum Data Set coordination feedback from state regulatory oversight). We have also seen a reduction in falls and behaviors (with potential harm to self and others) in our facility, where we have regularly used this tool in an interdisciplinary approach for the past year. The number of hospital admissions, geriatric psychiatry admissions, and consultations has also been declining, as compared to other facilities in the vicinity, and prior to its systematic use for our own facility.
Use of antipsychotics and antidepressants have also been significantly reduced, as noted on QI data for the facility. Initial analysis of our data is supportive of our observations and hypothesis regarding utility of ARMOR.
Meanwhile, we see the value and applications for ARMOR for people involved in caring for elderly persons, particularly in LTC, and in other segments of geriatric care continuum. Its simplicity offers a systematic approach to polypharmacy for all levels of caregivers. Suggested applications for clinicians using ARMOR are:
Medical Directors – To effectively manage polypharmacy in an interdisciplinary approach and address important QIs and accomplish GDR successfully for their facilities.
Physicians – For those involved in caring for the elderly, to assess polypharmacy at initial and subsequent visits.
Physician Assistants/Nurse Practitioners/Nurses – As a supplemental tool in assessing falls, behaviors, and unexplained functional decline.
Residents/Fellows/Medical Students – As a guide to manage medications and understand the changed physiology. To help them appreciate the principal impact of aging on pharmacokinetics and pharmacodynamics.
Pharmacists – As an aid to understand the clinician’s position on certain prescriptions and rationale. It may also aid in improving communication between pharmacists and other members of the nursing home (NH) clinical team in appropriate documentation and in implementation of regulatory standards, with an optimal care plan tailored for each resident of the facility.
----------
The following is an example of a patient who was evaluated using ARMOR.
Case:
A 78-year-old male resident of a LTC facility has a history of type 2 diabetes, coronary artery disease (CAD), coronary artery bypass graft (CABG) ‘04, hypertension, depression, cerebrovascular accident (CVA) with mild hemiplegia, and osteoarthritis of the knees and hips. The patient developed a stage 2 left-heel ulcer. His functional status required assistance in transfer from wheelchair to bed. Despite all measures taken to improve skin care and healing by the facility wound care team, the ulcer failed to heal completely. Meanwhile, the facility was cited twice by the state over a 3-month period for this resident. Tests showed the following:
• X-ray of the left heel showed no evidence of osteomyelitis.
• His HbA1c was 5.9 mg/dL, reflecting excellent control.
• Arterial Doppler test showed minimal peripheral vascular disease (PVD).
• Pre-albumin and albumin levels were normal.
• No evidence of poor appetite was noted.
• Patient was being closely observed and encouraged to move his extremities on a scheduled basis.
• Complete blood count with differential, basic metabolic panel was normal. Serum creatinine was 1.2 mg/dL.
His medications included:
Sotalol 80 mg twice daily
Aspirin 325 mg/day
Fentanyl patch 25 mcg every 72 hr
Nitroglycerin S/L, as needed
Famotidine 20 mg/day
Acetaminophen/hydrocodone 5/500 mg 3 times/day
Sertraline 75 mg/day
Simvastatin 20 mg/day
Trazodone 25 mg/day
Ibuprofen 800 mg orally 3 times/day, as needed
Vital signs were: pulse 72/min, blood pressure 120/70 mm Hg, afebrile, weight 132 lb.
On exam, his heart, lungs, and the remainder of the exam were normal, except for residual weakness from his CVA. A 2-cm x 1-cm stage 2 ulcer on left heel noted without any purulence. Pedal pulses were diminished but palpable bilaterally. No edema noted on lower extremities on exam. Local treatment was continued, and sotalol was held with continued monitoring of cardiac rhythm and blood pressure. The ulcer promptly responded to this measure and healed completely in the next 2 weeks.
_____________________________
Stepwise Approach Using ARMOR:
Step 1: A = Assess
1. Notable for more than nine medications.
2. Beta blocker was noted as suggested by step 1.
3. Antidepressants sertraline and trazodone were noted for duplication.
4. Beers Criteria list medications noted (ibuprofen).
Step 2: R = Review
1. Potential drug-body interaction likely with peripheral microcirculations, and beta blocker (sotalol) was considered.
2. Likely DDI between nitroglycerin and sotalol was reviewed.
3. Risk of hypotension with concomitant use of two hypotensive agents. Hypotension is enhanced in older adults due to decreased baroreceptors response and decreased venous tone and hypotension.
4. Potential of beta blocker for delayed healing in skin ulcer through microcirculation change of unopposed alpha receptor activity affecting primary function of healing was noted.
5. Potential for cognitive impact and falls risk associated with nonsteroidal anti-inflammatory drugs (NSAIDs) were identified.
Step 3: M = Minimize
1. NSAID was eliminated for its duplications and potential risk of side effects.
2. Trazodone was discontinued due to duplication of treatment.
Step 4: O = Optimize
1. Medications were adjusted for estimated creatinine clearance (36 mL/min/1.732; Cockcroft-Gault equation).
2. Sotalol was initially held for 2 weeks for observations of its presumed impact on nonhealing peripheral ulcer.
3. Later dose was optimized for renal function.
Step 5: R = Reassess
1. Patient was reassessed for clinical and functional status in a few weeks.
2. Ulcers healed in 2 weeks.
3. Sotalol was restarted at a dose adjusted for creatinine clearance.
----------
Conclusion
The case presented in this article attests to the poor physiological reserves in most elderly. It supports the dictum of optimizing and re-evaluating the risk-benefit profile of any pharmacological agent and potential drug-body and drug-drug interaction. Elderly people pose unique questions. The role of beta blockers is well known in hypertension and most myocardial infarctions. However, physiology in this population is in a fragile but compensated homeostasis. Commonly used agents can easily change this equilibrium, resulting in severe compromise in functioning.
This case also highlights the effects of beta blockers on peripheral circulation in this population. The unopposed effect of alpha receptors on peripheral circulation is to produce vasoconstriction in peripheral tissue beds. Peripheral microcirculation is a function of balance between the adrenergic system, vascular caliber, and other local factors.
A systematic approach with ARMOR was able to effectively improve patient care and outcome. It also helped the facility to deal with regulatory issues posed by the nonhealing ulcer. Adverse drug reactions from commonly used pharmacological agents should be routinely evaluated.
The author reports no relevant financial relationships.
Dr. Haque is Assistant Professor and Clinical Director of Geriatric Services, Department of Family Medicine, College of Human Medicine, Michigan State University, East Lansing.










