Wild on Wounds and AALTCN 2011 Conference Recap
The Wild on Wounds (WOW) and American Association for Long Term Care Nursing (AALTCN) 2011 conference, which took place at Caesars Palace, Las Vegas, NV, September 8 and 9, was all about the “WOW” factor, kicking off with attendees being greeted by jugglers and ribbon twirlers as they waited for the keynote address to begin. Before introducing the speaker, Craig Karges, a well-known mentalist and illusionist, the audience got warmed up by clapping, singing, and dancing to “We Are Family.” While the conference offered the wound and long-term care communities an abundance of educational opportunities, the presenters also emphasized the importance of enjoying and taking pride in what you do every day, whether you are tasked with managing slough and eschar or finding a solution to a long-term care challenge.
The theme of the keynote address was extrasensory perception, and audience participation was an integral component of the show. The first participant was a woman named Tami, who was called up on stage to blindfold Craig and tape around his eyes to ensure he could not see. She was then asked to write a word on the whiteboard, but not say it out loud, and Craig was tasked with guessing what that word was. Tami wrote “wound,” and Craig wrote the same word directly below it. The audience clapped as Craig joked about how easy that was. Another attendee came up on stage and brought with her a name badge from a random individual in the audience. Still blindfolded, Craig correctly guessed the name on the badge. The audience clapped again. A man in the audience was then asked to come up onstage with his wallet. He was asked to take out a bill and place his hands over the serial number. Craig guessed the denomination of the bill and started to read off the numbers, all of which were correct. The man responded, “you are a dangerous man,” to which the audience cheered.
The tricks became increasingly complex throughout the address, but it was not all about putting on a show. Craig also imparted some key messages. He noted that we all have extraordinary gifts because of our powerful brains and that we should never underestimate our abilities. He then proceeded to demonstrate his ability to memorize, which is a feat he taught himself. Sixteen people in the audience were each randomly selected to name a tangible object, which were then written down on a whiteboard for the audience to see. Facing away from the board, Craig was able to recount each of the 16 items, in any order, and starting from any number. While he would not give away the tricks to his elaborate illusions, such as table levitation, he did provide tips on how one’s memory can be improved. He noted that people frequently complain of having poor memory, but that any impairment in this faculty is generally attributable to not focusing on or paying attention to what is truly important. We are often distracted, he said. For example, when we are first introduced to someone, we may pay attention to inconsequential details, such as what the person is wearing, rather than his or her name, he noted. “Learn to use [your mind], learn to work with it, you are only limited by your imagination,” he concluded. The audience cheered as Craig exited. Thereafter, the Buzz Report—a session intended to keep wound care providers up to date on developments in their industry—commenced.
The Buzz Report
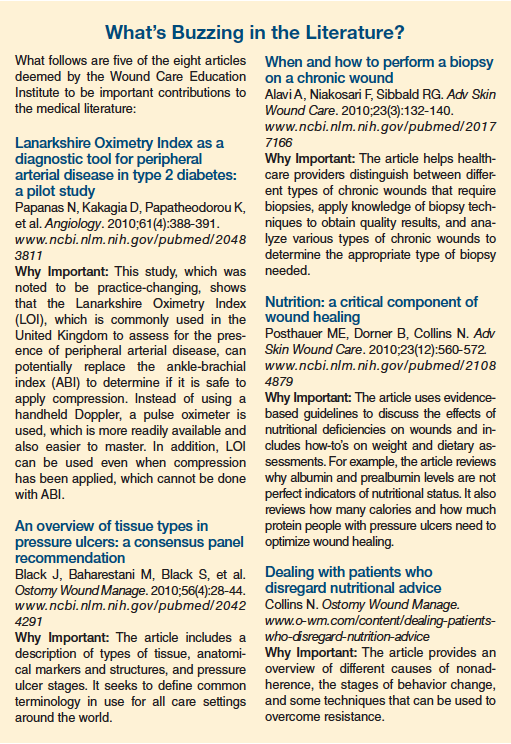
Because the wound care market is constantly changing, the Wound Care Education Institute (www.wcei.net) uses the Buzz Report to provide conference attendees a quick snapshot of their marketplace, including an overview of the latest news, products, and literature (some are outlined in the sidebar) that has the potential to change practice. The literature component was added for the first time this year. The organization felt this addition was warranted because more than 6 million biomedical articles are published annually, making it impossible for healthcare providers to stay on top of every important development.
What’s Buzzing in the News?
The following news items were outlined during the news component of the Buzz Report:
• Healthpoint has changed its name to Healthpoint Biotherapeutics. Several new products are anticipated and others have been recently acquired, such as Regranex Gel, a prescription drug for the treatment of deep neuropathic diabetic foot ulcers. More information on the company can be found online at www.healthpointbio.com.
• Hydrofera Blue, a moist wound dressing, is now promoted and distributed by Hollister Wound Care (www.hollisterwoundcare.com). The product’s formulation remains the same.
• Derma Sciences (www.dermasciences.com) received US Food and Drug Administration (FDA) clearance for MediHoney Hydrogel. It will be available in early 2012 with and without an adhesive border.
• As part of the Medicare Hospital Value-Based Purchasing Program, Medicare payments to hospitals will be based on quality and not quantity, as determined by 17 process-of-care measures and 8 patient satisfaction measures. Medicare reimbursements will be reduced to hospitals with high levels of preventable 30-day readmissions for three high-volume conditions: acute myocardial infarction, heart failure, and pneumonia. Patient satisfaction measures will be assessed upon the patient’s discharge from the hospital and will focus mainly on how nursing care was perceived by the patient. Hospitals will be paid based on how its measures compare with those of other hospitals. Lower-scoring hospitals will receive reduced Medicare payments, whereas high-scoring hospitals will be paid a bonus from those reductions. As of January 2012, the Centers for Medicare & Medicaid Services (CMS) will also start to look at “present on admission wounds.” If a wound worsens during hospitalization, or readmission or outpatient therapy is required following hospital discharge, the hospital will incur a higher cost per beneficiary. In addition, new scoring measures will be added, including hospital-acquired pressure ulcer stages III and IV. While initially applied to hospitals, it is anticipated that the same measures will be applied to long-term care facilities, clinics, physicians’ offices, and home care in approximately 2 years.
• Nursing homes have been hit with a $3.87 billion Medicare cut for 2012.
• On February 24, 2011, the FDA issued an update on complications associated with negative pressure wound therapy systems. Since 2007, 12 deaths and 174 injuries have been attributed to these systems. The FDA makes the following recommendations: (1) select patients carefully (eg, do not use with a malignant wound); (2) assess risk factors first (eg, anticoagulant use); (3) monitor frequently; and (4) if the system will be used at home, use the teach-back method to ensure the patient and his or her family understand how to use the system. The FDA’s update regarding these systems can be viewed at www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm
244211.htm.
AALTCN Sessions
Following the Buzz Report, conference goers could attend various educational sessions on wound care or the AALTCN director of nursing (DON) certification program. The DON program covered a myriad of topics, from running a nursing department to addressing lateral violence in the workplace. Whether attendees intended to become DONs or not, the program was designed to provide nurses with the knowledge they need to take the lead in tackling challenges they may face at their facilities.
Administration of a Nursing Department
During the “Administration of a Nursing Department” session, Lori Gutierrez, BS, RN-C, DON-CLTC, RAC-CT, CBN, clinical educator and long-term care consultant, Clinical Advisors for Resources and Educational Services, LLC (www.clinicaladvisorsllc.com), and an Annals of Long-Term Care advisory board member, discussed the nurse executive’s diverse range of responsibilities, which include administrative, clinical, educational, and public relations tasks. With so many different tasks required, numerous core competencies are essential for success, including the ability to effectively communicate and build relationships, a through understanding of the healthcare environment, leadership skills, business savvy, and unwavering professionalism.
Gutierrez noted that a mission statement is crucial to a nursing department’s success. The mission statement should outline the department’s mission (reason for being), vision (the underlying belief that guides the department), and standards (what the department hopes to achieve). If a mission statement is missing, one needs to be developed promptly. Even if one is in place, it should be reviewed to ensure it is current. She reported that she had consulted at one facility and discovered that their mission statement had not been updated in decades. Gutierrez proceeded to provide a few tips that DONs can use to develop an effective mission statement:
• Ensure the department’s vision is tangible so that people can understand it (eg, “to deliver competent care”).
• While the mission statement needs to incorporate core values that outline what the department believes in, these “beliefs” must always be rooted in evidence-based practice.
• Standards that are outlined need to be proactive in their approach, rather than reactive.
Another point of discussion was that DONs need to understand the big picture. This requires defining expectations, such as by setting standards and developing job descriptions; facilitating fulfillment of expectations, such as by communicating, educating, and providing staff with adequate resources; evaluating fulfillment of expectations, such as by conducting audits and surveys; and analyzing findings and employing strategies to correct deficiencies, such as by assembling a task force. While these tasks may seem daunting, they do not solely fall on the DONs shoulders. “You can’t do it alone, ever!” said Gutierrez, noting that there is a 9-month turnover for DONs. She stressed that every DON needs to have the right members on the team and the ability to delegate responsibility to these individuals.
Gutierrez proceeded to discuss the shift in managerial duties that have taken place in the 21st century. She noted that whereas control was previously at the top, there is now a shift to empower all levels of staff. DONs need to serve as role models, while making authentic connections with staff, the community, vendors, administration, other departments, regulators, families, residents, and volunteers. “You have to build bridges so that you can work well together as an interdisciplinary team,” she said.
To promote communication and collaboration, Gutierrez noted that DONs need to leave their offices and interact with staff and residents. She also noted the importance of conducting regular meetings, but emphasized that DONs should always go into the meeting with an agenda. The agenda should get distributed to all attendees before the meeting, and the meeting must start and end on time. When emailing people, whether to send them an agenda or discuss another matter, it is crucial to think about what you are putting in there, she noted. “Never put a patient’s name in the email. You can violate HIPAA [The Health Insurance Portability and Accountability Act of 1996 Privacy and Security Rules] regulations,” she warned.
Reducing Avoidable Hospitalizations
Pressure ulcers and unhappy families are the main reasons for lawsuits, noted Lisa Byrd, PhD, FNP-BC, GNP-BC, gerontologist, during a session that tackled the problem of avoidable hospitalizations and outlined some strategies that can be employed to avoid this costly issue. Byrd started the session by reviewing the scope of the problem, noting that of the 1.5 million residents in 16,400 US nursing homes, 33% are hospitalized each year, costing over $4.5 billion annually. While only 10% of elderly patients have dementia, the prevalence is between 60% and 70% in nursing homes. Since nursing home residents tend to be sicker, there is a much higher risk of hospitalization in this population, despite the fact that many hospitals do not know how to properly care for nursing home patients and generally cannot handle people who are not able to care for themselves, said Byrd.
Over the next 10 years, there will be a push to treat nursing home residents at the facility, rather than sending them to the hospital. According to Byrd, this is feasible because a substantial percentage of acute hospitalizations are avoidable. Currently, many residents are sent to hospitals simply to avoid lawsuits. However, hospitalizations can be harmful in some cases, putting residents at risk of numerous complications, such as delirium, pressure ulcers, and urinary incontinence from indwelling urinary catheter use.
To prevent residents from being hospitalized unnecessarily, a model needs to be established that includes education, follow-up care, and support. Geriatric concepts need to be taught to prescribing practitioners and to all nursing home staff, Byrd said. To ensure proper education of all essential parties, effective communication is imperative. This entails using proper language at all times; for example, it is not acceptable to use medical jargon when educating patients and families.
One model that Byrd discussed as a means of preventing unnecessary hospitalizations is the physician–nurse practitioner team approach. This model requires the following: (1) a prescribing practitioner to make rounds on a scheduled basis, preferably 2 to 3 days every week; (2) a protocol system for reporting problems; (3) a protocol system to treat residents; and (4) appropriate follow-up assessments. The goal is to prevent problems from occurring and to quickly treat any that may arise. One way to accomplish this objective is to remain cognizant of any acute changes in a resident’s condition, which Byrd defined as “any sudden clinically important deviation from the resident’s physical, cognitive, behavioral, or functional status.” Because certified nursing assistants are the ones interacting with residents the most, it is crucial for healthcare providers to try to maintain consistency of this staff and to pay attention when they voice a concern over a resident’s condition.
Certainly, not all hospitalizations are avoidable, said Byrd, noting that there are many cases in which residents need to be transferred, including the following scenarios:
• Acute abdominal pain of moderate to severe intensity with intractable vomiting;
• Chest pain that cannot be readily attributed to noncardiac causes;
• Fall with potential fracture;
• Hypertensive crises (systolic blood pressure, >230 mm Hg);
• Active gastrointestinal bleeding with hypotension and tachycardia;
• Respiratory distress that does not respond to oxygen, nebulizers, or suctioning.
Every institution should have a protocol in place to ensure any problems are properly reported. Procedures should be established for reporting issues that require immediate attention, findings that are nonimmediate, and findings that are routine. A reporting protocol ensures nursing staff understand what they need to report and what they are reading in reports, said Byrd. When developing protocols, it is important that they adhere to geriatric guidelines (eg, diabetic elders do not always require tight glycemic control if they have multiple comorbidities).
Addressing Lateral Violence
During the session on lateral violence, Nita Kasan, RN, MS, chief nursing officer, The College Network, provided the audience with an overall view of the nursing landscape before delving into the issue of lateral violence, a problem that may be more prevalent in nursing than previously thought. Kasan noted that there are >3 million registered nurses working in the United States. The average age of a nurse is 47 years and the average age at graduation is 31 years. Although nursing is the nation’s top profession in terms of growth until 2018, a nursing shortage remains. This is in part because of an 8% turnover rate and not enough graduates to fill vacancies. In addition, many older nurses are coming out of retirement to rejoin the workforce, making it more challenging for new graduates to find jobs and causing friction with younger staff members because of differing schools of thought.
Kasan defined lateral violence as any “behavior that is consciously or unconsciously used to control, undermine, or undervalue any individual or group.” Examples include imparting unwarranted or invalid criticism, shouting, socially isolating someone, gossiping or spreading rumors, taking credit for another’s work, allocating unrealistic workloads, blaming someone without proof, rolling eyes and crossing arms, and demonstrating impatience with questions or refusing to answer them. Lateral violence can be a persistent problem or a single event, and it can be instigated by coworkers, supervisors, or subordinates, but it is generally found to occur between nurses. Although it can affect nurses at all levels, newly licensed or hired nurses, hospital pool and traveling nurses, and nursing students are at especially high risk.
While many people do not want to refer to this phenomenon as violence, Kasan noted that the fact that there are victims indicate that it is a form of violence. Lateral violence can be driven or exacerbated by turf issues, miscommunication, and the culture at a facility, she said. Precipitating factors may include a nurse or other staff member receiving special attention from a physician, obtaining a promotion that others feel is undeserved, and staffing shortages.
Kasan noted that the phenomenon of “nurses eating their young,” which is how lateral violence is often colloquially described in nursing, should never be considered normal and is something that must change. Its impact is huge, said Kasan, noting it can lead to errors, stress, frustration, reduced collaboration, and many physical and emotional disorders, such as depression, insomnia, and eating disorders.
Kasan stressed that proactive prevention strategies need to be devised on a personal, organizational, and national level. She noted that several important resources are already available, including the American Association of Critical-Care Nurses (AACN) Healthy Work Environment Team Assessment tool (www.hweteamtool.org), which allows nurses to compare their work environment’s current health against standards set by the AACN. In addition, a free Web-based survey tool is available from the Center for American Nurses (www.centerforamericannurses.org), which can be obtained by e-mailing Diane Scott at diane.scott@centerforamericannurses.org.
The session concluded with Kasan urging the audience to take a stance against lateral violence. “The bottom line is that nurses have to be educated to recognize lateral violence, empowered to refuse to accept abusive coworker behaviors, and challenged to reverse workplace culture that tolerates such behavior,” she said.









