Vestibular Disorders in an Aging Population: Practical Applications for Long-Term Care Facilities
Dizziness and vertigo have become increasing concerns as the population of older adults continues to grow. Vestibular balance disorders are common contributors to the near-epidemic number of falls that is steadily increasing among elders, which has resulted in a sharp rise in emergency department visits and admissions to long-term care facilities. Although commonly placed beneath the general heading of “dizziness,” vestibular dysfunction constitutes a well-defined category of disorders that is often identified by both a distinctive history and characteristic physical findings. A plethora of systemic illnesses and disabilities typically encountered in this age group are often associated with reports of dizziness, which make managing vestibular disorders all the more challenging and complex. This article provides an overview of common vestibular disorders, including benign paroxysmal positional vertigo, vestibular neuritis, and Meniere’s disease, and outlines general diagnostic and treatment considerations. (Annals of Long-Term Care: Clinical Care and Aging. 2012;20[6]:20-25.)
____________________________________________________________________________________________________________
Vestibular dysfunction occurs in 35.4% of Americans aged 40 years and older and contributes to the high number and frequency of falls in the elderly population.1 Falls have become a major health problem. They are the foremost cause of both fatal and nonfatal injuries among individuals aged 65 years and older,2,3 and they contribute to a significant number of emergency department visits and increased admissions to long-term care (LTC) facilities. As a significant risk factor for falls, balance disorders should be identified and managed both to prevent future falls and to counteract the deleterious physical and mental impact that dizziness and vertigo frequently have on elders.4 Loss of balance typically results in loss of mobility and independence, which may prove devastating for individuals already suffering from the ill effects of aging and LTC confinement. In this article, we review common vestibular disorders and discuss diagnostic and treatment considerations for elders.
Understanding Dizziness and Vertigo
Dizziness is a generic term that refers to a wide array of subjective symptoms, a sampling of which includes feeling faint, unsteady, light-headed, or experiencing a swaying or spinning sensation. These terms have been bandied about by patients and clinicians alike and often represent subjective descriptions or personal interpretations rather than clinically factual diagnoses. Sloane and colleagues5 define dizziness as an all-encompassing term that may be broken down into four subsets: vertigo; presyncope; disequilibrium; and other sources of dizziness, such as anxiety, ocular pathology, or a tilting environment. A multitude of ailments and conditions may contribute in varying degrees to a report of dizziness, including eye disorders (glaucoma, macular degeneration); peripheral sensory organ deficits (peripheral vascular disease); arthritides of the cervical spine, hips, and knees; and multisensory disorders (diabetes).4
When referring to disorders of the vestibular system, dizziness and vertigo are the two most commonly used terms in the medical literature. Dizziness is perhaps one of the least understood conditions affecting all age groups, but becomes particularly confounding when present in those aged 65 years and older. Elders often have an array of systemic illnesses that have the potential to wreak havoc on their balance and oftentimes overlap those symptoms relating to vestibular pathology. Vertigo and dizziness, by their very nature, often result in self-imposed inactivity, which, in turn, gives rise to reduced muscle mass and diminished motor coordination,4 circumstances that may further complicate both diagnosis and treatment.
Vertigo conveys the perception of movement, and has been defined as an illusion of motion of one’s self (subjective vertigo) or of one’s surroundings (objective vertigo).6 Casual use of the term vertigo frequently engenders the notion that an inner ear or vestibular disorder is present, and when so used, should be critically addressed by the treating clinician, who must discover whether true vertigo is actually present. Although vertigo may be associated with either peripheral or central pathology (Table), approximately 80% of cases are peripheral in origin, most commonly representing benign paroxysmal positional vertigo (BPPV), vestibular neuritis (VN), or Meniere’s disease.5,7 Vertigo of central origin has been amply described in cases of migraine-associated vertigo (MAV), brain stem ischemia, cerebellar infarction, intracranial hemorrhage, head trauma, cervical spondylosis, multiple sclerosis, and seizure disorders.5,7

Overview of Vestibular Disorders
The vestibular system is a pivotal component in an information-gathering network that serves to control motion and balance by working in concert with the visual and somatosensory systems. Somatosensory input from an assemblage of sensors in the lower limbs and spine provides postural details about the position of the body relative to the body’s center of gravity. Visual input serves to control gaze fixation, visual acuity, and clarity during movement of the head and body. The processing of incoming sensory data by the central nervous system and the resulting musculoskeletal system responses are a cooperative endeavor that may be thought of as representing the three independent legs of an imaginary tripod that remains stable and in proper balance as long as each limb performs its stated function in unison with the others (Figure 1).
An insult to any of the aforementioned sensory components often results in dizziness or vertigo, which typically abates once compensatory mechanisms are brought into play by the other contributing systems. As one ages, however, compensatory vigor and the ability to recover from dizziness and vertigo become increasingly less efficient, as degenerative changes and concurrent illness limit the sensory, musculoskeletal, and/or neural components from rebounding. Loss of sensory hair cells and degenerative changes of peripheral vestibular neurons and the supporting elements that subserve participating end organs have been identified in an aging vestibular system.8 Other factors that may have an impact on compensatory recovery include medications, level of arousal, and environmental input.9 Further, a transient easing of vestibular symptoms may occur during a period of quiescence and then suddenly return. At times, these symptoms may reemerge in the guise of an entirely new clinical entity in elders. Such is the case, for example, when VN or Meniere’s disease later appears with findings that are consistent with BPPV.6
Benign Paroxysmal Positional Vertigo
BPPV may occur in up to 42% of all cases in which vertigo is present.6 It warrants particular attention, as it represents not only the most common vestibular disorder among all age groups, but also becomes more prevalent during an individual’s fifth to sixth decade of life. In one study, 9% of elderly patients were found to have undiagnosed BPPV during assessments for entirely unrelated issues.6
BPPV is typically identified by repeat episodes of positional vertigo, and features relatively short-lived rotatory or spinning sensations when the patient’s head is placed in certain provocative positions (ie, on the same plane as the semicircular canal), such as occurs when rolling over in bed, bending over, or in backward extension. Evidence suggests that BPPV is caused by one of two likely events: canalithiasis or cupulolithiasis. Canalithiasis is the result of misplaced debris from the otolith organ that enters the posterior semicircular canal, the most dependent canal within the labyrinth. Cupulolithiasis arises from the deposition of otoconia onto the cupola. Both processes initiate movement of the endolymph and, in so doing, stimulate sensory cells. When the head is placed in a provocative position, abnormal nystagmus and vertigo quickly ensue after a latency of 5 to 10 seconds. These fleeting episodes of nystagmus and vertigo typically last no longer than 60 seconds.6 Although causative events may be difficult to identify, the presence of BPPV has been associated with head trauma, VN, Meniere’s disease, prolonged bed rest, ear surgery, and infection.6 It has been noted that aged individuals with unrecognized BPPV have to cut back on a number of motor activities, suffer from depression, and may have experienced a fall within the 3 months leading up to their vertigo evaluation.10
Once diagnosed, BPPV often resolves spontaneously. If it persists, introducing either one of two conservative therapeutic modalities is warranted. The first, commonly referred to as habituation exercises or Cawthorne-Cooksey exercises, was initially proposed by Cawthorne in the 1940s. The intent of these exercises is to impart tolerance of vertigo by the vestibular system without attending to the source(s) of the problem. These particular exercises typically include movements that bring about the onset of vertigo. Initially, the exercise regimen involves simple movement of the head, eyes, and body while the person is in a secure, sedentary position. These exercises are followed by more complex integrative movements that are in tune with routine daily activities. The exercises are intended to diminish vertigo to those offending positions or movements. The second therapeutic modality for BPPV, canalith repositioning procedures (Epley or Semont maneuver), seek to relocate the offending canaliths from the posterior semicircular canal to a safe location where fluid dynamics are no longer affected. The Epley maneuver is most commonly used to treat BPPV of the posterior canal. In brief, the head is moved in a series of predetermined positions to force canaliths from remaining in the posterior canal and directs them to the vestibule, where they no longer cause vertigo.
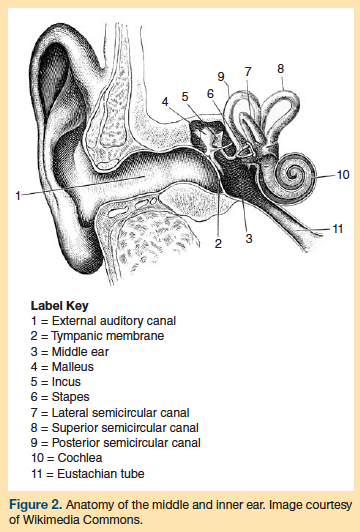
Of the three semicircular canals (lateral, superior, and posterior; Figure 2), the posterior canal is most commonly involved in BPPV and is clinically identified by the onset of vertigo and nystagmus when the Dix-Hallpike maneuver is performed. This maneuver places the head in various preset provocative positions (first with the patient sitting upright with his or her legs extended and then with the patient in the supine position) that typically result in stimulation of the posterior semicircular canal with resultant characteristic nystagmus and identifiable vertiginous patterns6 (Table). The presence of nystagmus may serve as a window to the vestibular system and sheds light on the vestibulo-ocular reflex.
The lateral semicircular canal is seldom involved in BBPV, but if such appears to be the case, the supine roll test,6 rather than the Dix-Hallpike maneuver, is performed to confirm the diagnosis. During the supine roll test, the physician quickly turns the patient’s head to the side to check for nystagmus while the patient is in the supine position. The patient’s head is returned to the face-up position until the nystagmus stops. The process is then repeated, with the patient’s head being turned to the other side.
Each semicircular canal is oriented in a different plane; thus, the diagnostic maneuver used depends on which canal is being investigated (Figure 2). As previously stated, the Dix-Hallpike maneuver is performed to assess pathology of the posterior canal, whereas the supine roll test is used to evaluate the lateral canal. Any head-hanging maneuvers, however, should be performed and interpreted with caution, particularly in patients with vertebrobasilar disease or cervical spine derangement.4
Vestibular Neuritis
VN typically presents with an acute onset of incapacitating, whirling vertigo, but generally occurs without any change in hearing acuity. VM differs from labyrinthitis, described as inflammation of the labyrinth of the inner ear causing vertigo, often in conjunction with hearing loss. The vertigo experienced in patients with VN is typically accompanied by nausea, vomiting, and diaphoresis, all of which lead to prostration and an underlying fear of a potentially more serious condition. This vertigo may last for hours or weeks, and generally resolves spontaneously, although a sense of unsteadiness may persist for a period of time thereafter. Supportive treatment is adequate in most cases with the use of antiemetics, vestibular suppressants, or both in the early phases of the attack, when symptoms may be at their worst and most debilitative. An antecedent or concurrent viral process has long been implicated in VN and gives rise to inflammation of the superior division of the vestibular nerve. Clinical signs include the presence of spontaneous nystagmus and diminished vestibulo-ocular reflexes.
Meniere’s Disease
Meniere’s disease, also known as endolymphatic hydrops, is a labyrinthine disorder of unknown etiology. It is characterized by the classic reports of vertigo, fluctuating hearing loss, tinnitus, and aural fullness in the affected ear. An overabundance of endolymph (hydrops) results in a ballooning out and distortion of the membranous labyrinth, which likely causes membrane disruption. Characterized by remissions and exacerbations, the vertigo experienced by individuals with Meniere’s disease, which may last for hours, is often accompanied by nausea and vomiting.6 Clinical changes may ensue as the disease progresses, with fluctuating hearing loss commonly evolving into a permanent loss in the affected ear. Vertigo may ultimately subside, but it is occasionally replaced by a feeling of disequilibrium.11 Treatment for Meniere’s disease includes salt and caffeine restriction, diuretics, and transtympanic steroid injections. Of the approximately 10% of patients who fail to respond to medical management, surgical intervention (endolymphatic sac surgery, labyrinthectomy, or vestibular neurectomy) has been described.12
Migraine-Associated Vertigo
MAV may present as an actual symptom of a migraine and is often referred to as vestibular migraine (VM).13 On occasion, MAV appears with any one of a number of disorders or injuries, including BPPV, cerebellar disorders, head trauma, or depression. Vertigo has been described as spontaneous or positional in cases of VM and may precede, follow, or accompany migraine headaches. The presence of typical migraine symptoms, such as photophobia, phonophobia, and auras, helps to confirm the diagnosis of VM. Many of the medications used in the treatment of migraine headaches may also prove helpful in treating VM. Stress management, avoidance of known triggers, and vestibular rehabilitation (discussed in greater detail in the “General Treatment Considerations in Elders” section) have all been used with varying degrees of success.13
Superior Canal Dehiscence Syndrome
Often unrecognized in the differential diagnosis of peripheral vestibular disorders is superior canal dehiscence syndrome, which features attacks of vertigo and oscillopsia, defined as a visual disturbance in which fixed and nonmobile visualized objects appear to oscillate. Oscillopsia is classically brought about by the presence of loud sounds or the application of pressure within the ear canal. Computed tomography (CT) imaging may identify an area of dehiscence in the bone located above the superior canal. Treatment of superior canal dehiscence syndrome entails surgical repair of the dehiscent bone should symptoms persist.
Visual Vertigo
A number of patients with vestibular disorders have been found to suffer from visual vertigo, a condition in which vestibular symptoms are evoked or exacerbated when certain visual stimuli come into view. These stimuli commonly include walking down the aisle of a supermarket, watching movies, or sitting in a moving car or train. In a 2001 study, Guerraz and colleagues14 found that 17 of 21 patients diagnosed with visual vertigo had a confirmed history of or were currently experiencing vestibular dysfunction. The presence of visual vertigo may help explain why some patients with vestibular disorders experience ongoing vertiginous episodes or vary in their recovery response to standard balance therapy. A number of individuals with vestibular disorders have been shown to be visually dependent, indicating that they rely on visual cues more so than vestibular or proprioceptive cues in maintaining spatial orientation and balance. Those visually-dependent patients who suffer from a balance disorder note an increase in symptoms when in certain visually provocative environments, such as those previously noted.14 Use of other rehabilitative modalities, particularly those promoting visual stimulation, may be required in an attempt to initiate compensatory mechanisms when visual vertigo is diagnosed.
General Diagnostic Considerations in Elders
Specific diagnostic considerations were outlined for each verstibular disorder under the “Overview of Vestibular Disorders” section of this article, but there are some general diagnostic considerations that should be kept in mind when confronted with an elder reporting dizziness or vertigo. A proper detailed history is of the utmost importance in these individuals, as it often proves decisive in arriving at a diagnosis. As mentioned previously, a vestibular disorder may be likened to a tripod with sensory, central nervous system, and musculoskeletal legs (Figure 1). Determining which leg of the imaginary tripod is off-kilter or nonfunctional is the initial challenge and is often instrumental in helping to establish the correct diagnosis.
At the outset, being able to identify true vertigo from all of the other subjective reports that fall under the heading of “dizziness” is a critical first step, as vertigo is a well-established feature of vestibular dysfunction. Although the overwhelming majority of individuals reporting dizziness receive a diagnosis of a nonvestibular disorder,5 it should be appreciated that vestibular and nonvestibular disorders often occur concurrently in elderly patients. Requesting collaboration with various specialties will likely prove helpful in peeling away the myriad of other overlapping conditions that often lend additional confusion to an already perplexing vestibular disorder.
Vestibular function testing has been proposed whenever the etiology of vertigo or dizziness is unclear, treatment has proven unsuccessful, or more than one vestibular disorder is being considered as the diagnosis. This testing focuses on eye movements, nystagmus in particular, and evaluates the integrity of the vestibulo-ocular reflex in response to labyrinthine stimulation, positional changes, and rotational testing.6 Magnetic resonance imaging and CT imaging should be strongly considered for patients who display neurologic findings, who possess stroke risk factors, or in whom routine vestibular function testing proves inconclusive.
General Treatment Considerations in Elders
Treatment of vestibular disorders depends on the underlying pathology and the patient’s physical constitution and capacity for vestibular compensation. El-Kashlan and colleagues9 define this compensation as a capacity to achieve partial or total functional recovery. A reshuffling of processes at the level of the brain stem and cerebellum occurs during compensation, but may be negatively impacted upon by a number of factors, including medication, concurrent illness, and debility. When performing a Dix-Hallpike procedure or vestibular rehabilitation, care must be taken in debilitated elders, particularly those suffering from obesity, cervical spine pathology, vertebrobasilar disease, or other restrictive musculoskeletal disorders.4 Customization should help offset any confusing results or untoward complications that may surface in the performance of testing or therapy.
Vestibular rehabilitation remains the mainstay of treatment for vestibular disorders. Customized rehabilitation exercises result in central nervous system habituation and adaptation to those provocative movements of the head, body, and eyes that are found to initiate or contribute to vestibular symptoms.15 These rehabilitative programs have contributed to a reduction in both symptoms and disabilities while helping to establish improved balance and postural stability.4
Anxiety and vestibular disorders appear to be closely interrelated. Shared or overlapping neural circuitry may help explain why dizziness occurs among many patients suffering from anxiety, and why anxiety, avoidance, and autonomic arousal are often encountered among individuals with vestibular disorders.15 Compensatory mechanisms and vestibular rehabilitation may lead to a more favorable outcome if behavioral modification and other adjunct therapies, such as mindfulness and cognitive-behavioral techniques, are incorporated into vestibular rehabilitative regimens. Relapse rates are also diminished when these behavioral modalities have been so integrated.15
Sloane and colleagues5 recommend treating dizziness with a management-oriented approach, rather than being guided by a specific diagnosis. This treatment-oriented strategy includes such traditional considerations as attending to underlying psychiatric, visual, and polypharmacy issues as well as nontraditional approaches, such as acupuncture and rocking chair therapy. In the final analysis, when recovery fails, balance control falters, often resulting in increased levels of stress or despondency and decreased levels of activity and socialization.5
A review of the patient’s current medications by the treating clinician may help shed light on a number of perplexing issues that frequently appear in the presence of dizziness in general and vertigo in particular. Polypharmacy, defined by the number of medications prescribed to an individual or the issuance of medications that may not be needed, should be carefully considered when evaluating aging patients with vestibular disorders. Wetmore and colleagues4 list H2 blockers, urinary antispasmodics, laxatives, and tricyclic antidepressants as medications that need to be monitored and eliminated should the issue of polypharmacy arise. These authors contend that more than 50% of aged patients are prescribed at least one nonindicated medication.
As in the case of visual vertigo, where visual motion desensitization may be added to the treatment protocol to develop tolerance to provocative visual stimuli, other individualized techniques should be added to routine therapies if recovery is lagging or proves elusive. Older individuals suffering from vestibular disorders must be encouraged to participate in light to moderate physical exercise, which has been found to decrease the risk of falling, increase quality of life, and help counteract the depression reported to occur in more than 42% of patients with
dizziness.4
Careful monitoring of comorbid systemic diseases, such as diabetes, is of paramount importance. Diabetes has been described as being vestibulotoxic because of its contribution to ischemic changes in the vestibular structures and the abnormal glucose metabolism theorized to occur in the labyrinthine fluids.1,16 An increase in otoconial debris has been described in patients with type 1 diabetes, often resulting in a greater chance of developing BPPV among those who have had diabetes for an extended period of time.17 Viewing vertigo and dizziness in a geriatric patient as a potential multisystem and multisensory condition may provide needed insight when managing these most difficult and challenging cases.
The casual use of antiemetics and anticholinergics should be avoided in persons with vestibular disorders, as they may hinder or delay compensatory mechanisms that are often the basis of recovery. Seeking to relieve some of the more troubling symptoms associated with vertigo with vestibular suppressant medications may be clinically sound early on; however, their use should be discontinued on an individual basis so as to allow compensation to bring about alleviation and welcomed relief to those patients who are experiencing these often incapacitating symptoms.
Conclusion
Elderly persons, particularly those in LTC facilities, typically suffer the ill effects of vestibular disorders, which have been shown to contribute to the marked increase in falls that typically occur in this population. The dizziness associated with a number of systemic diseases adds an additional layer of confusion when seeking to identify a suspected vestibular disorder. An exacting history is frequently the decisive first step in determining the diagnosis. Successful treatment outcomes rely on the need for customized treatment regimens to accommodate individual deficits and disabilities, and should therefore be instituted for each and every patient who is referred for vestibular rehabilitation.
The authors report no relevant financial relationships.
References
1. Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004. Arch Intern Med. 2009;169(10):938-944.
2. Owens PL, Russo CA, Spector W, Mutter R. Emergency department visits for injurious falls among the elderly, 2006. HCUP Statistical Brief #80. October 2009. Agency for Healthcare Research and Quality; Rockville, MD. www.hcup-us.ahrq.gov/reports/statbriefs/sb80.pdf. Accessed May 17, 2012.
3. US Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). www.cdc.gov/injury/wisqars/index.html. Accessed May 25, 2012.
4. Wetmore SJ, Eibling DE, Goebel JA, et al. Challenges and opportunities in managing the dizzy older adult. Otolaryngol Head Neck Surg. 2011;144(5):651-656.
5. Sloane PD, Coeytaux RR, Beck RS, Dallara J. Dizziness: state of the science. Ann Intern Med. 2001;134(9 Pt 2):823-832.
6. Bhattacharyya N, Baugh RF, Orvidas L, et al; American Academy of Otolaryngology-Head and Neck Surgery Foundation. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008;139(5 suppl 4):S47-S81.
7. Lai YT, Wang TC, Chuang LJ, Chen MH, Wang PC. Epidemiology of vertigo: a national survey. Otolaryngol Head Neck Surg. 2011;145(1):110-116.
8. Nadol JB Jr, Schuknecht HF. Pathology of peripheral vestibular disorders in the elderly. Am J Otolaryngol. 1990;11(4):213-227.
9. El-Kashlan HK, Shepard NT, Asher AM, Smith-Wheelock M, Telian SA. Evaluation of clinical measures of equilibrium. Laryngoscope. 1998;108(3):311-319.
10. Helminski JO, Janssen I, Kotaspouikis D, et al. Strategies to prevent recurrence of benign paroxysmal positional vertigo. Arch Otolayngol Head Neck Surg. 2005;131(4):344-348.
11. Staab JP, Ruckenstein MJ. Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg. 2007;133(2):170-176.
12. Goebel J. Practical Management of the Dizzy Patient. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:301-319.
13. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256(3):333-338.
14. Guerraz M, Yardley L, Bertholon P, et al. Visual vertigo: symptom assessment, spatial orientation and postural control. Brain. 2001;124(Pt 8):1646-1656.
15. Naber CM, Water-Schmeder O, Bohrer PS, Matonak K, Bernstein AL, Merchant MA. Interdisciplinary treatment for vestibular dysfunction: the effectiveness of mindfulness, cognitive-behavioral techniques, and vestibular rehabilitation. Otolaryngol Head Neck Surg. 2011;145(1):117-124.
16. Klagenberg KF, Zeigelboim BS, Jurkiewicz AL, Martins-Bassetto J. Vestibulocochlear manifestations in patients with type 1 diabetes mellitus. Braz J Otorhinolaryngol. 2007;73(3):353-358.
17. Yoda S, Cureoglu S, Yildirim-Baylan M, et al. Association between type 1 diabetes mellitus and deposits in the semicircular canals. Otolaryngol Head Neck Surg. 2011;145(3):458-462.










