Tips for Surviving the Flu Season Based on the CDC Guidelines for Long-Term Care
Abstract: Influenza (flu) infections are a serious and costly occurrence that can cause significant morbidity and mortality. This is especially true for immunocompromised and frail older adults, who have a reduced response to vaccination and often suffer more complications. Older adults in long-term care facilities (LTCFs) are at even higher risk for sequelae due to disease containment challenges in these settings. LTCFs need to have a clear plan while preparing their staff for the flu season. Based on the Centers for Disease Control and Prevention guidelines for LTCFs, authors provide a brief overview of flu infection and flu vaccination in older adults followed by a practical breakdown of preparatory steps, treatment, and management procedures for the flu season in the form of a Tip Sheet.
Key words: influenza, Centers for Disease Control and Prevention guidelines, vaccination, flu season, outbreak
Influenza (flu) infection is a serious disease that can lead to dangerous complications and high costs for treatment. The Centers for Disease Control and Prevention (CDC) estimates that the number of annual flu-related deaths averages anywhere between 12,000 to 56,000,1 and some estimates put the total annual economic burden of flu infection at $87.1 billion.2
The populations most vulnerable to flu complications include those with multiple chronic diseases and adults aged 65 and older, particularly if they are frail. Frail older adults also have the added risk of poor immune response to vaccines.3 It is for these reasons that medical directors and nursing chiefs in long-term care (LTC) environments should be particularly vigilant to prevent flu infections and consequent outbreaks.
In many LTC facilities (LTCFs), an open environment is encouraged, where residents can come and go freely, can intermingle between units, on outings, and in the dining room, and can regularly visit their families on passes. This open design and encouragement of free movement contributes to a greater risk for transmission and dissemination of flu infection. LTCFs are also challenged by staffing concerns. High staff turnover—with multiple floating staff who come in and out without always knowing standard facility protocols—poses a challenge to the implementation and enforcement of preventative measures, diagnostic procedures, and management of flu cases. To complicate matters further, older adults often do not present with the typical constellation of symptoms and signs of infection.4,5
The CDC has very specific guidelines for a flu outbreak in LTCFs, as outlined in Interim Guidance for Influenza Outbreak Management in the Long Term Care Facilities.6 In order to help LTC professionals prepare for the flu season, an overview of flu infection and vaccination in older adults is provided below, followed by a concise breakdown of the CDC guidance in the form of a Tip Sheet, detailing how to prepare for the flu season as well as flu outbreaks. (Please see Tip Sheet in attached PDF at end of page.)
Presentation of Flu Infection in Older Adults
Infections, like many clinical disorders in older adults, may present without typical symptoms. There may be absence of fever, headache, sore throat, myalgia, and cough. Rather, residents may manifest nonspecific findings of unexplained loss of appetite, generalized weakness, falls, varying levels of confusion, dyspnea, and/or some changes in activities of daily living.
Importance of Vaccination
It is well documented that vaccines can help reduce infection rates (flu and secondary pneumonia), hospitalizations, and mortality related to the flu, especially when the group itself has a high rate of vaccinations.7-9 The CDC also notes that outbreaks have been attributed to low vaccination coverage among staff.10 However, staff and resident vaccination can often be a challenge. LTCF staff may be unwilling to be vaccinated for a variety of reasons. Furthermore, local policies or union agreements may limit implementation of mandatory preventive strategies to reduce the exposure and transmission of influenza in their settings.
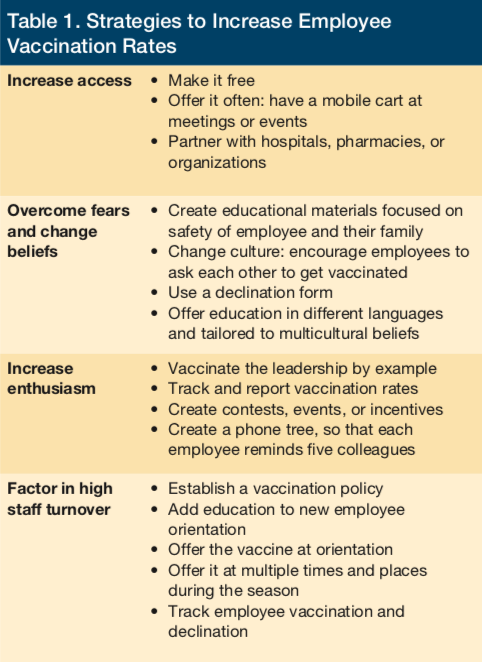
The CDC summarizes a number of barriers to employee vaccination along with strategies and resources to overcome these barriers.11 Some strategy examples can be found in Table 1. Of course, in order to further reduce the risk of transmission within a facility, these strategies can also be directed toward residents and their families.
Considerations for Using Tip Sheet
Some staff education and strategies to prepare for flu season include optimizing communication about the seriousness of any occurrence. During an outbreak of flu, the urgency can feel chaotic if people are not trained to react. Ensuring that staff are well-educated on flu infections and outbreak procedures is an excellent way to decrease feelings of inadequacy in staff and improve prevention and containment of flu infection. Materials containing an overview of the flu virus, vaccines, and precautions is recommended for all staff. This Tip Sheet can be printed, adapted into email form, or be integrated into a standard operating procedure document for easy distribution, so that people have a document to refer back to and are prepared to react quickly and calmly. A slide presentation can be created using this Tip Sheet as well. Facility managers may also want to create slide presentations for specific types of staff members, such as registered nurses, with more extensive information related to vaccination, isolation, and swabbing techniques included, as well as how to recognize symptoms and the best ways to respond.
It may be difficult to disseminate materials directly due to silos of management, but an attempt should be made to distribute information to department heads for self-education. Before flu season starts, it may be helpful to appoint a flu medical provider who is empowered to alert the staff with updates and who can be available to field questions and problems. In addition, medical providers should frequently be present on the unit to monitor for updates, to be available for questions, and to encourage or offer prophylaxis or flu shots.
Conclusion
Preparing for flu season in the LTC setting should start early and involve all staff members. The more informed staff are about the seriousness of a flu outbreak, the easier it will be to prevent and contain widespread infection in facilities. Having consistent and accessible protocols will keep staff focused and organized around the task of reducing morbidity and mortality associated with flu infection in the LTC setting. We hope this Tip Sheet may be helpful for facilities preparing for the flu season and in the event of flu outbreaks.
To read more articles in this issue, visit the 2017 November/December issue page
To read more ALTC expert commentary and news, visit the homepage
References
1. Centers for Disease Control and Prevention. Estimating seasonal influenza-associated deaths in the United States. CDC website. https://www.cdc.gov/flu/about/disease/
us_flu-related_deaths.htm. Updated December 9, 2016. Accessed August 22, 2017.
2. Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: Measuring disease burden and costs. Vaccine. 2007;25(27):5086-5096.
3. Song JY, Cheong HJ, Hwang IS, et al. Long-term immunogenicity of influenza vaccine among the elderly: risk factors for poor response and persistence. Vaccine. 2010;28(23):3929-3935.
4. Norman DC. Clinical features of infection in older adults. Clin Geriatr Med. 2016;32(3):433-441.
5. Castle S, Yeh M, Toledo, S, et al. Lowering the temperature criterion improves detection of infections in nursing home residents. Aging: Immunol Infect Dis. 1993;4(2):67-76.
6. Centers for Disease Control and Prevention. Interim guidelines for influenza outbreak management in long-term care facilities. CDC website. https://www.cdc.gov/flu/professionals/infectioncontrol/ltc-facility-guidance.htm. Updated March 28, 2017. Accessed August 22, 2017.
7. Carmen, WF, Elder AG, Wallace LA, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in the long-term care: a randomized control trial. Lancet. 2000;355(9198):93-97.
8. Pop-Vicas, A, Rahman M, Gozalo PL, Gravenstein S, Mor V. Estimating the effect of influenza vaccination on nursing home residents’ morbidity and mortality. J Am Geriatr Soc. 2015;63(9):1798-1804.
9. Arden N, Monto AS, Ohmit SE. Vaccine use and the risk of outbreaks in a sample of nursing homes during an influenza epidemic. Am J Public Health. 1995;83(3):399-401.
10. Saito R, Suzuki H, Oshitani H, Sakai T, Seki N, Tanabe N. The effectiveness of influenza vaccine against influenza a (H3N2) virus infections in nursing homes in Niigata, Japan, during the 1998-1999 and 1999-2000 seasons. Infect Control Hosp Epidemiol. 2002;23(2):82-86.
11. Centers for Disease Control and Prevention. Barriers and Strategies to Improving Influenza Vaccination among Health Care Personnel. CDC website. https://www.cdc.gov/flu/toolkit/long-term-care/strategies.htm. Updated September 7, 2016. Accessed August 22, 2017.









