Skilled Nursing Facility Value-Based Purchasing: Are You Ready?
Believe it or not, it has been over 4 years since the passage of the Protecting Access to Medicare Act (PAMA), which introduced a new system for reimbursing skilled nursing facilities (SNFs). Section 215 of the PAMA outlines the SNF Value-Based Purchasing Program1 and discusses this payment method specifically. However, while it has been 4 years since this program was introduced, the full program details and specifics about implementation are just being enacted now. There is some still time before the full impact of this change will be felt, but SNFs should already be preparing to deliver on what is expected.
The foundation for this value-based reimbursement system is the Centers for Medicare & Medicaid Services (CMS) SNF quality measures2 with several new measures that have been recently added,3 the most significant of which are those for readmissions and resource use. These include all-cause, all condition hospital readmission measures in addition to resource use as measured by the all condition risk-adjusted potentially preventable hospital readmission rate for SNFs. These measures are being applied not only to the largest SNFs but also to small facilities, many of whom may have been mistaken in thinking they would be exempt due to their size. CMS is required to ensure that the methodology being used achieves a high level of reliability and validity, especially for SNFs with a low volume of readmissions.
Shifting Focus
SNFs have not had to focus on such areas of care in the past, similar to how hospitals have not previously been responsible for issues that had occurred once a patient was wheeled to their car and returned home. Now, though, SNFs are being held accountable for events occurring well outside their facility walls.
This new level of accountability is the result of data demonstrating the significant waste of funds due to avoidable hospitalizations. According to 2010 data, 23.5% of patients discharged from acute care hospitals to SNFs were readmitted to the hospital within 30 days, at a financial cost of $10,362 per readmission or $4.34 billion per year.4 Of these readmissions, 78% were labeled avoidable. More recent evidence suggests that hospitalization rates for dual-eligible patients living in long-term care facilities decreased by 31% between 2010 and 2015.5 This decrease stems from the steadily increasing responsibility/accountability of SNFs, which has forced a focus on avoiding hospitalization through increasing their scope of services provided in house as well as being more aware and responsive to changes in condition.
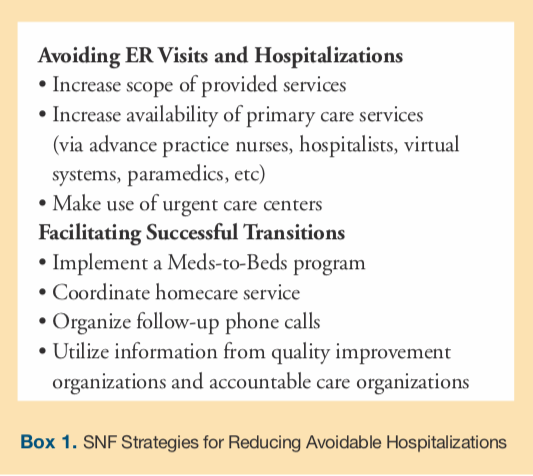
This new level of accountability requires SNFs to adjust their care processes. SNFs would be well-served to focus on 2 critical areas that they may not have previously been paying much attention to. These include (1) avoidable emergency room visits and hospitalizations that occur during patient stays (2) and transitions of patients from their facility to the community (Box 1). Facilities can augment their refocusing strategies based on data provided by CMS, who has already started providing data to SNFs quarterly through confidential feedback reports on their performance with respect to the CMS SNF quality measures.
Avoidable Emergency Room Visits and Hospitalizations
To begin addressing these problems, facility leaders should identify gaps in care. This means analyzing each and every unplanned emergency room visit and hospitalization. Many SNFs use the INTERACT program,6 which is increasingly being built into SNF electronic medical records systems. Many facilities using this program find that these transfers could have been avoided through increased availability of primary care services and by increasing the scope of services available within the SNF.7 Indeed, services that have historically only been available in the hospital are increasingly becoming a regular part of the SNF care plan. For example, telemetry monitoring8 or dialysis9 were previously not thought of as being available within an SNF, but, as facilities are being called upon to provide a higher level of care, services like these are now becoming more commonplace.
In terms of increasing availability of primary care services, SNFs, for some time, have looked to engaging advanced practice nurses (APNs). These APNs can either be directly employed by the SNF through one of the attending physician groups (via the health plan responsible for many of the residents in the facility) or by a health plan, typical via Special Needs Plans (SNPs).10 SNPs are Medicare Advantage Plans that can provide managed care to long-term care residents to produce improved clinical and financial outcomes. These improved outcomes come through the ability to provide skilled care without the Medicare required 3-day acute hospitalization prior to SNF admission. Increased access to primary care services is provided through the SNP’s own APN who is available in the SNF to immediately address clinical issues. SNFs sometimes rent out their APNs to SNPs which can assist in supporting their activities.
There is another approach SNFs can employ to address the following 2 challenges at once: the issue with patient’s gaining admission to the SNF and improving outcomes through advancing primary care services. To address these issues, facilities can develop a relationship with the local hospital to use their hospitalist as SNFist. This is one model for SNFist where hospitalists from a local hospital serve as attending physicians usually focused on the subacute unit. This provides increased continuity of care, since these same hospitalists were caring for these patients before their subacute admission while they were in the hospital. Hospitalists are also well-suited for this role as they are trained to deal with patients in need of complex, acute care.
Some additional innovative avenues for increasing primary care services are being developed through the use of virtual after-hour services11 and high-level provider services delivered within the SNF in-person on a timely as-needed basis.12
When services cannot be brought into the SNF, residents must be transferred for evaluation. This can be accomplished through the emergency room or, alternatively, by visiting an urgent care center—centers which are ever-increasing in numbers and level of services. By establishing a relationship with emergency departments whereby a Rapid Assessment + Initial Treatment (RAbbIT) can be implemented, SNF patients can be assessed in a timely manner, initial treatment can be started, then they can be transferred back to the SNF for completion of their care, thus avoiding a hospitalization.
Facilitating Successful Transitions
Now that SNFs are being held accountable for events that occur after a care transition is complete, more attention will need to be given to certain processes leading up to discharge. One area that can be given more attention is education on medications for patients. Staff should make sure patients fully understand how to use their medications and confirm that patients have access to these treatments once they leave the facility. Increasing the involvement by pharmacists through a program referred to as “Meds to Beds” may be helpful. In this program, pharmacists visit patients’ bedside and provide education about their therapies and medications—knowledge that is the foundation for adherence to therapy. Having a pharmacist provide medications along with education to a patient prior to their discharge home will help patients be more successful at remaining at home on discharge.
SNFs should also make an effort to track every patient discharge to ensure that each patient is receiving the proper care to allow them to remain at home. This can best be accomplished by connecting with patients on discharge within 48 hours, then at 10- and 30-day intervals. Besides gaining valuable information to track readmission rates, these contacts provide an opportunity to address any questions that may arise. But data on readmission rates can also come from the regional quality improvement organizations that are responsible for providing SNFs this type data. Accountable care and managed care organizations can also assist in providing this data to SNFs as well, since they have access to claims data, unlike SNFs. Continued tracking of this information can then be used to identify subsequent opportunities for interventions to improve care and reduce readmission rates in the environment outside the SNF.
In light of and in addition to the above recommendations, SNFs may be best served by having a strong relationship with homecare agencies that provide a continuation of SNF services within patients’ homes. While these homecare services are typically provided by nurses, there is a growing number of agencies that can provide just aides at home. These are individuals that assist with daily living assistance, prepare meals, provide light housekeeping and companionship, and run errands, which are often the services needed to support a patient transitioning from the SNF. Having a list of homecare nursing and aide services to support SNF patients at home is critical to maintaining adequate care for high-risk older adults at home.
Impact on Payments and Referrals
In addition to altering how SNFs deliver care to patients, the SNF Value-Based Purchasing Program will also impact reimbursement processes and referrals of patients to SNFs. This system will affect payments directly from Medicare, as SNFs able to deliver better outcomes will receive additional payments while those that fail to deliver on the quality measures will be penalized. In addition, it is likely that all other payers, from commercial to Medicaid, will likely follow suit with similar financial bonuses and penalties.
SNFs will also see an increase in the volume of referrals as health systems, payers, and providers look to increase their utilization of higher performing SNFs. The information regarding these CMS SNF quality measures is publically available on the Medicare SNF Compare website, which is meant to drive patients and their families to use these high performing SNF. This same information is being used by hospitals looking to reduce their readmission rates and improve the financial and clinical performance of their accountable care organizations, thus they will look for SNFs who can deliver better outcomes.
Conclusion
This new world of accountability is forcing SNFs to develop new processes to deliver on these accountable clinical and financial outcomes through new care models such as SNFist, the RAbbIT program, discharge/community follow-up, and other programs. These various interventions can be applied to improve clinical and financial outcomes for patients and payers alike. In the end, an increased volume of referrals and bonus payments will come to those SNFs that are able to deliver on the CMS SNF quality measures—especially the quality measures that focus on readmission rates—while patients are in the SNF and after they have been discharged to the community.
SNFs need to be ready for this new value-based purchasing world, or they will find themselves extinct.
References
1. Protecting Access to Medicare Act of 2014, 42 USC §113-193 (2014).
2. Centers for Medicare & Medicaid Services (CMS). Skilled Nursing Facility (SNF) Quality Reporting Program Measures and Technical Information. CMS website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Measures-and-Technical-Information.html. Updated August 21, 2017. Accessed March 21, 2018.
3. Centers for Medicare & Medicaid Services (CMS). Skilled nursing facility readmission measure (SNFRM) NQF #2510: all-cause risk-standardized readmission measure. CMS website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Other-VBPs/Technical-Report-Supplement.pdf. Published April 2017. Accessed March 21, 2018.
4. Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57-64.
5. Brennan N, Engelhardt T. Data Brief: sharp reduction in avoidable hospitalizations among long-term care facility residents. The CMS Blog. https://blog.cms.gov/2017/01/17/data-brief-sharp-reduction-in-avoidable-hospitalizations-among-long-term-care-facility-residents/. Published January 17, 2017. Accessed March 21, 2018.
6. Pathway Health Services. What is INTERACT. Pathway Health Services website. https://www.pathway-interact.com/about-interact/what-is-interact/. Accessed March 19, 2018.
7. Handler SM, Sharkey SS, Hudak S, Ouslander JG. Incorporating INTERACT II clinical decision support tools into nursing home health information technology. Ann Longterm Care. 2011;19(11):23-26.
8. Cardio Staff. www.cardiostaff.com. Accessed March 19, 2018.
9. DialyzeDirect LLC. https://www.dialyzedirect.com/. Accessed March 19, 2018.
10. Centers for Medicare & Medicaid Services (CMS). Your guide to Medicare Special Needs Plans (SNPs). US Government site for Medicare website. https://www.medicare.gov/Pubs/pdf/11302.pdf. Revised November 2011. Accessed March 19, 2018.
11. TripleCare. https://triple.care/. Accessed March 19, 2018.
12. DispatchHealth. https://www.dispatchhealth.com/. Accessed March 19, 2018.
To read more ALTC expert commentary and news, visit the homepage









