Protecting Staff and Resident Health Requires a Comprehensive Staff Immunization Program—During Flu Season and Beyond
ECRI Institute and Annals of Long-Term Care: Clinical Care and Aging (ALTC) have joined in collaboration to bring ALTC readers periodic articles on topics in risk management, quality assurance and performance improvement (QAPI), and safety for persons served throughout the aging services continuum. ECRI Institute is an independent, trusted authority on the medical practices and products that provide the safest, most cost-effective care.
Vaccines have helped to eliminate some very serious diseases in the United States and throughout the world. For illnesses that have not been fully eradicated, vaccines have helped to both lessen the effects of the illnesses and decrease the number of people affected. Various federal agencies and groups have recommended that personnel who work in aging services and home care be immunized against specific illnesses, such as hepatitis B virus (HBV) and influenza (flu), due to inherent risks from the job and resident or client susceptibility to some diseases.
Additionally, the risks associated with infectious outbreaks go beyond the direct impact of illness. Infectious outbreaks can have serious negative effects on the day-to-day care and service delivery environment—which then can act as root causes and contributing factors for other adverse events for both persons served and those delivering services. These outbreaks can simultaneously intensify resident and patient care workloads and affect continuity of staffing and scheduling. Comprehensive immunization programs can therefore be an important part of a provider organization’s risk, quality, and safety practices contributing to environments that help to inhibit adverse events.
CDC-Recommended Immunizations
Some vaccine-preventable illnesses are of particular importance to people working in aging services because they are at higher risk of exposure and because residents may be more susceptible to some diseases. For example, many aging services workers are frequently exposed to body fluids, which can pose an HBV risk. Additionally, older adults may be more likely to experience serious complications if they contract certain diseases; certain subpopulations of residents (eg, those who are immunocompromised) may be at even greater risk.
The potential for severe complications of vaccine-preventable illnesses can be higher in older adults than in other age groups because of decreased immunity and sometimes because of the communal living environment, for those who live in such settings. Cognitive or physical limitations may also increase illness severity because disease symptoms may be harder to identify, potentially delaying treatment and causing the individual’s condition to worsen.1 For example, the risk of dehydration may be higher among older adults with cognitive impairment who have the flu, as they may be unaware of their water loss.2 Because some vaccines do not provide as much protection to older adults, vaccination of personnel who work for aging services providers can be even more imperative than in other settings (eg, hospitals).
Infection prevention and control programs are essential to all aging services and home care providers, and maintaining staff immunity is an important component of these programs. The Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP) recommends that health care personnel (HCP) be vaccinated against or have evidence of immunity to measles, mumps, and rubella; tetanus, diphtheria, and pertussis; varicella; and seasonal flu.3 HBV vaccination is recommended for personnel who are at risk for exposure to blood or body fluids (in addition, the Occupational Safety and Health Administration [OSHA] requires employers to make HBV vaccine available to such employees). For certain other diseases (eg, meningococcal disease, typhoid fever, polio), ACIP recommends vaccination only for specific groups at high risk (eg, those who travel to countries where the disease is more common).3 In addition, ACIP annually updates its general recommendations on vaccination against seasonal flu, and these recommendations address immunization of HCP.4 CDC has also published guidance on evaluating staff members’ HBV immunoprotection after vaccination.5
ACIP emphasizes that the recommendations applicable to all HCP concern more than just those with responsibility for direct resident or patient care. In its recommendations on immunization of HCP, ACIP uses the following definition of HCP3:
HCP are defined as all paid and unpaid persons working in health-care settings who have the potential for exposure to patients and/or to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air. HCP might include (but are not limited to) physicians, nurses, nursing assistants, therapists, technicians, emergency medical service personnel, dental personnel, pharmacists, laboratory personnel, autopsy personnel, students and trainees, contractual staff not employed by the health-care facility, and persons (e.g., clerical, dietary, housekeeping, laundry, security, maintenance, administrative, billing, and volunteers) not directly involved in patient care but potentially exposed to infectious agents that can be transmitted to and from HCP and patients.
Staff who are not directly involved in resident care may frequently enter resident areas. Also, many of these illnesses are highly contagious, so even staff who might not directly expose residents could expose a coworker who may have resident contact. In addition, staff may miss work or be less productive if they become sick or have to take care of sick family members.
ACIP specifically lists long-term care (eg, skilled nursing, assisted living) and home care as settings that its recommendations for immunization of HCP apply to. But it also states that the recommendations are not limited to those settings listed. Therefore, aging services providers should carefully consider which staff throughout the organization the recommendations apply to, instead of simply limiting their immunization programs to skilled nursing or “health care” settings. Accordingly, use of the term “health care personnel” in this article refers to all individuals included in ACIP’s broad definition.3
The ACIP guidelines state that organizations should review the vaccination and immunity status of HCP upon hire and at least annually. Immunization records should be maintained for HCP; records should include documentation of the individual’s immunity status regarding recommended vaccine-preventable diseases (documented disease, vaccination history, or serology results), vaccinations administered, and postvaccination adverse events. In the event of an outbreak, up-to-date, well-organized records can help the organization identify susceptible personnel and take appropriate action. 3
Vaccination Programs and Promotion
Vaccination programs for staff are important to promoting vaccination. Aside from state or employer requirements for vaccination, the literature suggests that no one specific method or component will make a campaign successful; rather, a multifaceted approach to increasing vaccination rates is often suggested. Active promotion of the vaccines also seems particularly helpful in ensuring high acceptance rates among staff.6 Many organizations offer tools and other resources to promote vaccination, including a toolkit available for purchase from AMDA – The Society for Post-Acute and Long-Term Care Medicine.7
Organizations should determine whom to include in the vaccination campaign, remembering that most of ACIP’s recommendations regarding immunization of HCP apply to CDC’s broad definition of the term. Potential factors to consider include levels of care, services provided, staffing patterns and rotations, infection risks faced by staff who work at other organizations as well, and physical spaces, amenities, and staff shared by residents from different units or levels of care.
Under certain conditions, temporary and agency staff may be considered employees of the organization for specific purposes (eg, compliance with OSHA’s blood-borne pathogens standard8). Therefore, organizations may wish to outline requirements for specific immunizations in contracts with staffing agencies. They should also get written confirmation of immunizations from the staffing agency (eg, up-to-date immunization records) and ensure that the agency staff members’ immunizations stay current. This is especially important for immunizations that are required by law or regulation.
The use of vaccine declination forms may cause personnel to evaluate their options before declining the vaccine, potentially increasing the vaccination rate. Additionally, these forms can give organizations valuable information about the reasons for vaccine refusal. Aside from using declination forms, potential ways to track reasons for declining vaccines include surveys and focus groups. Declination forms and surveys are not standalone interventions; rather, they should be part of a multifaceted approach to improving immunization.
Although there may be a limit to the increase in vaccination rates that educational efforts can inspire,9 education is an important component of a vaccination program. Surveys of HCP have indicated that some do not receive the necessary information to make a decision regarding vaccination.9 For example, staff may not know which vaccines are recommended for them, may underestimate their risk of infection for or the severity of certain diseases, may have misconceptions about individual vaccines, or may underestimate the potential effect of their decision not to vaccinate on the organization’s residents or clients.
Reviewing the components of the vaccination program can help aging services and home care organizations understand how to improve the program. A thorough review can help organizations understand the strengths and weaknesses of vaccination efforts; subsequent changes, and possible addition of strategies to the program, can help to increase the vaccination rate.
Many organizations recommend tracking vaccination rates as a patient safety and quality goal. Also, knowing its vaccination rate can help an organization understand where it lies in reference to various recommendations and benchmarks. Increasing rates not only will improve the health of personnel but also may protect vulnerable residents and clients from disease complications.
Promoting Flu Vaccination
A major focus of vaccination promotion efforts is annual vaccination against seasonal flu. Unlike the other immunizations that are recommended for all HCP, seasonal flu vaccination should be repeated annually. Seasonal flu is also a major cause of morbidity and mortality that is easily spread. In aging services, seasonal flu vaccination should be part of a comprehensive plan to prevent and control influenza. CDC offers “A Toolkit for Long-Term Care Employers: Increasing Influenza Vaccination among Health Care Personnel in Long-term Care Settings,” which can help the organization design and evaluate such a plan.10
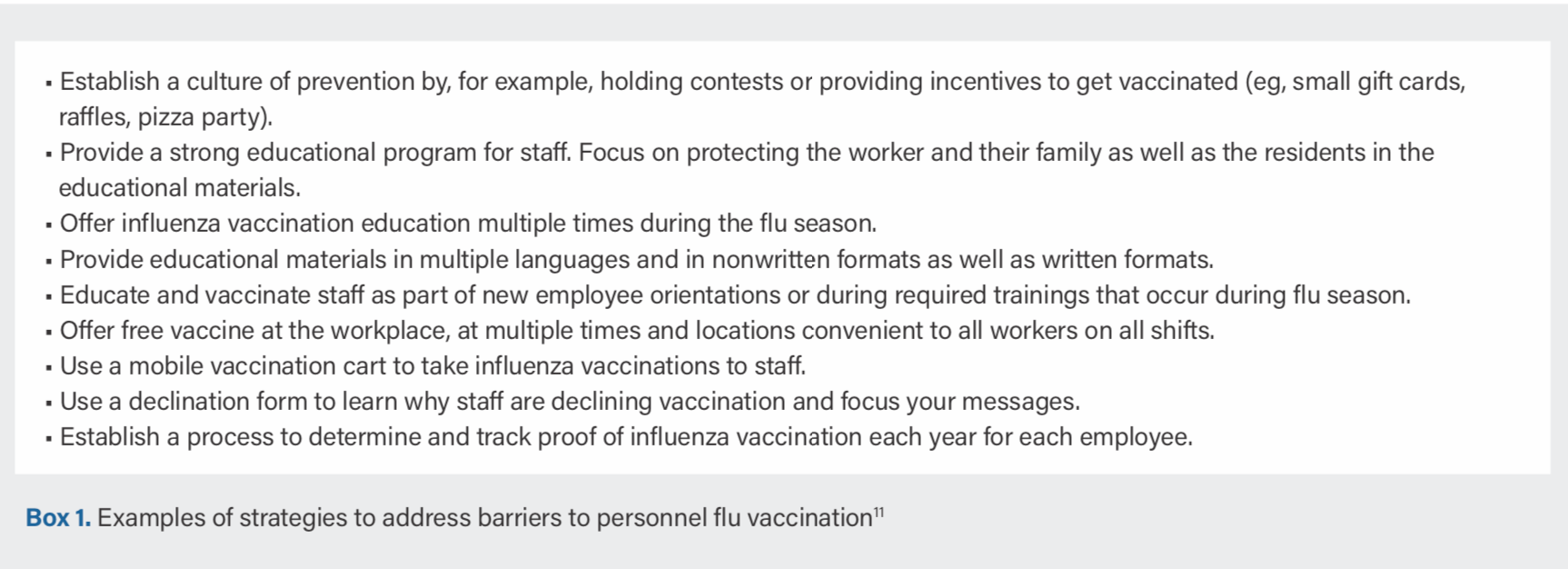
Aging services organizations should aim to maximize flu vaccination coverage among HCP. According to the CDC toolkit’s section on barriers and strategies, a multifaceted approach may be the most effective way of increasing successful flu vaccination among long-term care staff. Individual strategies included in a multifaceted approach may address barriers such as inadequate access to flu vaccine, decentralized work environments, high staff turnover, language or literacy barriers, low enthusiasm for vaccination, and beliefs about vaccination (eg, flu is not a serious illness, flu vaccine causes illnesses).11 The toolkit lists strategies to address each barrier (Box 1).
Finally, requiring annual seasonal flu vaccination as a condition of employment seems to be very effective in achieving high flu vaccination rates. Although it is now supported by many professional organizations, mandating vaccination is still controversial.12 Some health care organizations have required only that every worker participate in their vaccination program—for example, by either receiving the vaccine or signing a declination statement.
Conclusion
Staff members who contract vaccine-preventable illnesses experience negative effects on their own health. They may also transmit infections to residents and may be less productive or miss work, which can in turn affect the quality of resident care. For some vaccine-preventable diseases, personnel can transmit infection before symptoms start or while remaining asymptomatic. Older adults generally, and some subpopulations specifically, are more susceptible to particular diseases or more likely to develop complications. Immunization of personnel protects both staff and residents or clients.










