Preparing Family Members for the Death of a Loved One in Long-Term Care
Abstract
Family members of long-term care (LTC) residents at the end of life often feel unprepared for the death of a loved one. Family unpreparedness can lead to increased health costs and an increased risk of poor health outcomes such as complicated or prolonged grief, mood disturbances, sleep disorders, and poor quality of life. The purpose of this article is to discuss what is known about preparedness for death, the assessment of preparedness, and evidence-based interventions to improve preparedness of family caregivers in the LTC setting. Twenty-two articles from 20 studies on preparedness were identified, but the literature is scarce on preparedness specifically in the LTC setting; most of the literature focuses on the white population and on the population with cancer. Key clinical implications include that health care providers should assess family preparedness, tailor teaching to a family’s cognitive and emotional processes, and provide practical support and resources to assist in preparing for death.
Citation: Ann Longterm Care. 2019;27(2):25-31.
DOI: 10.25270/altc.2018.12.00052
Received December 8, 2016; accepted January 15, 2018.
Published online February 8, 2019.
Introduction
Family members of long-term care (LTC) residents at the end of life often feel unprepared for the death of a loved one. In 1 study, almost half of family members reported that the death was unexpected.1 Even among family members who recognize that death is expected, confusion about prognosis, symptoms, and decision-making have been reported.2,3 In addition to the immediate emotional distress accompanying the death, family unpreparedness can lead to increased health costs and an increased risk of poor health outcomes such as complicated or prolonged grief, mood disturbances, sleep disorders, and poor quality of life.
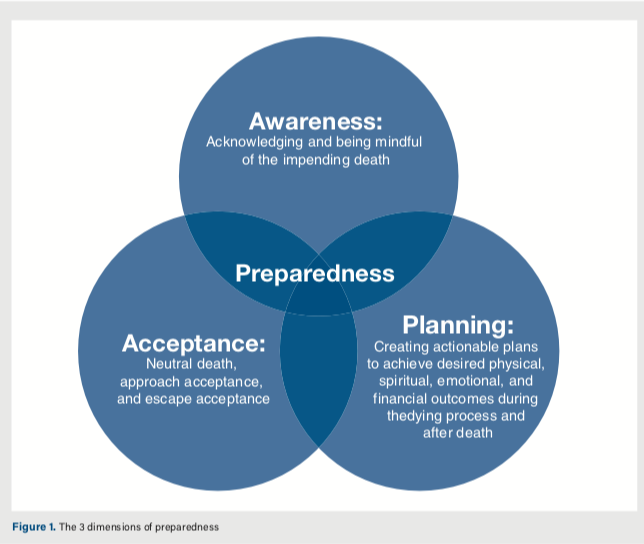
In her concept analysis of death preparedness, McLeod-Sordjan4 characterized preparedness by 3 key concepts: awareness, acceptance, and planning for the end of life (Figure 1). Awareness indicates that the family caregiver acknowledges and is mindful of the impending death of his or her loved one.4 Awareness is necessary for acceptance, although awareness does not guarantee acceptance. Acceptance of death can come in several forms, including neutral death (facing death rationally as an inevitable end of every life), approach acceptance (accepting death as a gateway to a better afterlife), and escape acceptance (viewing death as a better alternative to a painful existence).4 Along with awareness and acceptance, family members may engage in planning for the end of life—creating actionable plans to achieve desired physical, spiritual, emotional, and financial outcomes during the dying process and after death.4
Article continues below Figure.
The purpose of this article is to review the literature on preparedness for death, the assessment of preparedness, and evidence-based interventions to improve preparedness of family members in the LTC setting.
Methodology
The search engines CINAHL and PubMed were used to search for the terms preparedness, family members, death, death of a loved one, end of life, healthcare providers, bereavement, and long-term care to identify research articles written in English. The search was initially limited to 2012 through 2017 for the most recent findings and was specific to the LTC setting, but these search parameters resulted in a very limited set of articles. The search was then expanded to the last 15 years (2002-2017) and to family member preparedness in the context of end of life.
Results
After eliminating duplicates, 49 articles were retrieved. After reviewing the abstracts and articles, we eliminated the ones that were not relevant to the topic (n=18), were focused on the pediatric population (n=10) or were not related to preparedness of family members (n=6). Review of article reference lists led to the identification of 6 additional articles.
The search process ended with a total of 22 articles representing 20 studies (Hebert 2008, Hebert 2008, and Hebert 2009 all used the same study in their articles).
Eleven of the studies were conducted in the United States,1-3,5-15 while 9 were conducted internationally in Australia (n=2),16,17 Japan (n=3),18-20 Sweden (n=3),21-23 and Taiwan (n=1).24
Six of the studies were qualitative and descriptive,2,5,9,11, 13,19,23 while 6 used cross-sectional survey data to provide quantitative descriptive information.1,3,10,18,20,21 Three used a longitudinal approach using repeated surveys.6,22,24 Five examined the impact of interventions, mainly psychoeducational interventions.7,8,13,16,17
Among the studies, 14 examined family members of deceased persons with specific diagnoses such as Parkinson disease (n=1),10 dementia (n=2),2,13 and cancer (n=11),6,9,16-24 while 6 were not disease-specific.1,3,5,7,8,11,13,14
With the exception of 2 studies done in Japan and Sweden,18,20 the majority of the family caregivers studied were women. Of the studies done in the United States, the caregivers studied were primarily white, with some African American representation. Racial or ethnic composition was not reported in the international studies.
Discussion
Preparedness was not always well-defined across the literature. Family members interpreted the concept of preparedness in different ways, including being aware that the loved one’s prognosis was poor (awareness), having emotionally adjusted to the approaching loss (acceptance), and/or being prepared for the tasks of caregiving at the end of life (planning).4,9 Family members noted that there was a difference between the more-cognitive awareness of the prognosis and the emotional acceptance of impending death.15,23 They were more likely to address the practical issues such as wills and funeral arrangements than to prepare emotionally.23
Although all studies involved family members of patients with poor prognoses, and 9 studies took place in the context of hospice and palliative care,5,9,11,13-17,19,22 10% to 67% of family members reported being unprepared.2,8,10,21,22 Two studies involving family members of persons with neurodegenerative diseases (Parkinson disease10 and dementia2), a high percentage of whom were placed in LTC, had high rates of unpreparedness (53%10 and 67%2). However, another study focused specifically on bereaved family members of persons placed in LTC had a very low rate of unpreparedness (less than 10%).8
These findings appear to indicate that neither diagnosis nor setting necessarily ensures preparedness.
Family members described being unprepared for both the physical and emotional aspects of caregiving.2 They had a deep uncertainty about what symptoms to expect and what death would look like.9,23 Interestingly, Cagle and Kovacs9 found that family members acknowledged that the emotional defense mechanisms of denial and avoidance may have prevented them from processing the information fully when it was presented.
Health care provider behaviors that increased family member preparedness included a clear disclosure of prognosis to the family and to the patient,19 while avoiding saying that they “can no longer do anything for the patient.”18 Other positive health care provider behaviors included coordinating a discussion about priorities of care early on, while the patient can still participate, and pacing explanations according to family emotional preparedness.18 Similarly, Kehl5 describes how repetition and tailoring information to family questions and desires are 2 key aspects of the clinician’s role in preparing family members for the death of a loved one.
Importantly, the literature included a range of health care providers and those involved in care, including nurses,5,16,17 physicians,18,20 chaplains,5 social workers,2,5,9 and nursing assistants.5 We have followed the literature and use the term health care provider to include all professions, although we recognize that some roles (such as prognosis disclosure) are more suited to certain professions than others. Spouses of a terminally ill patient are less likely than adult children to feel prepared for death.8
Family members with depression,8 those who do not participate in advance care planning (ACP),8 and those who are not the primary caregiver or decision-maker10 are also at higher risk for unpreparedness. In particular, family members who were communicating long-distance via telephone found it hard to obtain desired information to prepare and to trust the information provided emotionally.9 This aspect is particularly relevant to the LTC setting.
Feeling unprepared was anxiety-provoking and distressing for family members both before and after the patient’s death.2,9,23 Unpreparedness was also associated with poor short- and long-term consequences, including prolonged and complicated grief,6,8,24 depression,6,21,22 anxiety,6,21,22 lower satisfaction with life,6 chronic pain,21 and sleep disorders.21,22
Formal interventions to assist in preparedness have demonstrated usefulness. Caregiving at Life’s End (CGLE), a psychoeducational intervention that can be delivered either individually or in a group setting and that aims to provide family members with information on what to expect and with coping skills, has shown a positive impact in improving caregivers’ sense of closure.7 Another psychoeducational intervention tested in Australia and involving a combination of home visits and telephone calls to provide family members with information and support similarly improved caregiver’s preparedness.16,17
Clinical Implications
In considering how to best address preparedness in the LTC setting, health care providers should first recognize how important it is to ask the simple question, “If your loved one were to die soon, how prepared would you be for his or her death?”8 LTC facilities should consider which health care provider roles are most appropriate for this assessment (such as nurse, social worker, or physician) and should include information and training on preparedness in job orientation and in-services. Because family members may ask questions of any health care provider (including nursing assistants and aides), all should be prepared to respond.
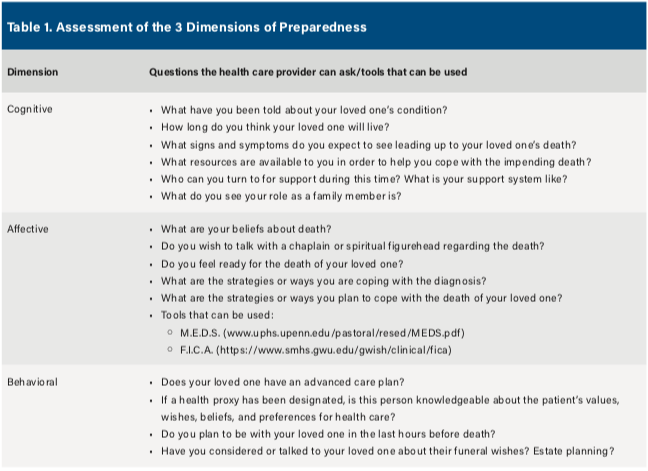
In moving forward with assessments and implementation, it is important to keep in mind the 3 dimensions of preparedness: cognitive, affective, and behavioral (Figure 1).15 The cognitive dimension relates to the knowledge of medical, practical, psychosocial, or religious/spiritual information related to their loved one’s death.15 This can be best assessed by asking family caregivers what they know about their loved one’s condition, prognosis, and the expected signs and symptoms leading up to death.7 It can also consist of asking family caregivers if they are aware of community resources available to them (such as support groups) and if the they have a support system to help them through the bereavement process. Furthermore, the health care provider can ask family caregivers about their role and responsibilities in caring for their loved one.7 Assistance in identifying a support group may be obtained from the local Agency on Aging or from a hospice/palliative care organization.
The affective dimension consists of mentally and emotionally preparing for the death of their loved one, which can be assessed by asking about family caregivers’ beliefs about death, readiness for the death, and how they will cope with and accept the death.15 The behavioral dimension refers to tasks such as making funeral arrangements, rearranging work schedules, and estate planning.15 Assessing behavioral preparedness may involve asking questions about these plans and whether family caregivers have accepted the transfer of responsibility from care receiver to caregiver (or others) for financial, legal, and health care matters.7 Specific questions and tools to assess the 3 dimensions of preparedness are listed in Table 1.
Article continues below Table.
Another resource is the CGLE program, which health care providers can use as a reference during their assessments.7 In addition, a flow sheet for assessing family caregiver preparedness and intervening to prepare these family caregivers can be found in Figure 2.
Article continues below Figure.

Cognitive. To address the cognitive dimension of preparedness, health care providers need to educate family caregivers about the dying process, death, and bereavement. This preparatory material must be individualized in its content, delivery, and timing to ensure that the education is relevant and all-encompassing for that particular family caregiver.5,14,25 Education on the dying process should include signs and symptoms of impending death and instructions for what caregivers can do to alleviate symptoms.5,26 For example, health care providers should review expected respiratory changes, restlessness, and anorexia with family caregivers. It is also important for family caregivers to know the implications of these signs and symptoms in terms of the dying process as well as an estimation of how long it will be until death occurs.5
In order to provide this sensitive information, it is important that health care providers build trust and develop relationships with family caregivers. Strategies that health care providers can use include active listening, repetition, demonstration or hands-on teaching, and collaboration with other clinicians. All disciplines of the interdisciplinary team should participate and have a role in preparing family caregivers.5 It can be beneficial to develop a checklist to document preparation among all disciplines, in order to allow for each health care provider to reinforce or clarify what has previously been taught.5
Affective. To address the affective dimension of preparedness, health care providers can support the feelings and emotions of family caregivers as they face the impending death of their loved one. Health care providers can recommend and encourage family caregivers to attend support groups for soon-to-be bereaved persons dealing with a death. This provides a space to listen to and talk with others who are in a similar situation, which may increase feelings of preparedness.3
Health care providers can also provide coping skills-training to provide techniques for managing the emotions associated with impending death, which can incorporate a meaning-based component.6 Health care providers can initiate or recommend a specialist to initiate music therapy as a measure of comfort as well as to ease communication and sharing between family caregivers and their loved one.25 Art therapy is another coping method that allows family caregivers to express emotions about death, increase emotional awareness of death, promote a reflection on the possibility of death, and foster meaning behind the death.27-29 Specific music and art therapy interventions have been described in the literature.25,27-29
Health care providers can also encourage family caregivers to do a life review with their loved one, providing questions for the caregiver to ask their loved one. The life review facilitates the telling of the patients’ story, including significant events from their life, expressions of meaning in their life, and important relationships,7 which allows family caregivers the opportunity to talk about and reflect on their loved one’s life. The life review can also include photographs, music, objects, and possessions. Health care providers also can recommend and incorporate spiritual leaders into their care plan so that family caregivers can attend to the spiritual elements of coping and peace.7
Behavioral. To address the behavioral dimension of preparedness, health care providers can work with family caregivers to create specific plans and actions. ACP is strongly associated with preparedness.8 Health care providers should talk with family caregivers about and explain ACP, as well as encourage them to create an advanced directive. ACP allows family caregivers to know and respect their loved one’s wishes about health care at the end of life, which limits the number of conflicts that can arise as the individual goes through the stages of dying.
In addition, health care providers should encourage family discussions and decisions on financial, legal, and social affairs that will arise with the death.7 This will help them to organize logistics surrounding the death, including estate planning and funeral arrangements.12 A social worker or legal expert in estate planning may be particularly useful in assisting family caregivers with the practicalities of planning for death.
It is important that these cognitive, affective, and behavioral dimensions of preparedness are addressed by a collaborative, interdisciplinary team.5,15 Each member of the health care team should be involved in the preparation. Each brings a different area of expertise and relationship with family caregivers, which together will allow for maximal positive outcomes for preparedness.5 Discussions between the health care team and family caregivers should occur frequently and be paced in stages, instead of occurring all at once.18,25
It is also important to note that the content and timing of these conversations addressing the cognitive, affective, and behavioral domains of preparedness should be individualized to the particular family caregiver.24 Factors such as culture, religion, and long-term family dynamics may play a large role in family caregivers’ perception of death and ability to prepare for death.
Limitations and Future Research
We acknowledge that there are many gaps in the literature on preparedness, and some of the literature we used was dated. We must also point out that most research has been done in the United States, and significant populations have been overlooked, including the Hispanic/Latino community. More research is needed on cultural aspects of caregiver preparedness. Most of the prospective, longitudinal studies only examined a single question of preparedness. More prospective, longitudinal studies examining multidimensional assessments of preparedness are needed, along with studies examining specific preparedness interventions.
Future studies could examine how to separate preparedness from depression, grief, and anxiety. During the end-of-life period, these conditions frequently occur concurrently and may inhibit feelings of preparedness in family caregivers. In addition, it is unclear when to start preparing family caregivers for the death of their loved one. More research is required in order to distinguish what stages of a patient’s illness necessitate the initiation and implementation of the preparation processes.
Conclusion
Preparing family caregivers for the death of a love one is important in order to promote quality of life and prevent adverse health effects such as complicated or prolonged grief, mood disturbances, and sleep disorders. Preparedness involves awareness, acceptance, and planning for death across the domains of cognition, affect, and behavior. Health care providers should assess and support family caregivers across these domains. By working as part of a collaborative, interdisciplinary team to prepare family caregivers for the death of a loved one, health care providers can improve family caregivers’ end-of-life experiences and decrease emotional distress in a difficult time of their lives.
Affiliations, Disclosures, & Correspondence
Authors:
Kristina Terzakis, BSN, RN • Meredith A MacKenzie, PhD, RN, CRNP, CNE
Affiliations:
Villanova University College of Nursing,
Villanova, PA
Disclosures:
The authors report no relevant financial relationships.
Address correspondence to:
Kristina Terzakis, BSN, RN
800 E. Lancaster Avenue
314 Driscoll Hall
Villanova, PA 19085
Email: kterzaki@villanova.edu
References
1. Williams SW, Zimmerman S, Williams CS. Family caregiver involvement for long-term care residents at the end of life. J Gerontol B Psychol Sci Soc Sci. 2012;67(5):595-604.
2. Hovland-Scafe CA, Kramer BJ. Preparedness for death: how caregivers of elders with dementia define and perceive its value. Gerontologist. 2017;57(6):1093-1102.
3. Barry LC, Prigerson HG. Perspectives on preparedness for a death among bereaved persons. Conn Med. 2002;66(11):691-696.
4. McLeod-Sordjan R. Death preparedness: a concept analysis. J Adv Nurs. 2014;70(5):1008-1019.
5. Kehl KA. How hospice staff members prepare family caregivers for the patient’s final days of life: an exploratory study. Palliat Med. 2015;29(2):128-137.
6. Kim Y, Carver CS, Spiegel D, Mitchell H-R, Cannady RS. Role of family caregivers’ self-perceived preparedness for the death of the cancer patient in long-term adjustment to bereavement. Psychooncology. 2017;26(4):484-492.
7. Kwak J, Salmon JR, Acquaviva KD, Brandt K, Egan KA. Benefits of training family caregivers on experiences of closure during end-of-life care. J Pain Symptom Manage. 2007;33(4):434-445.
8. Schulz R, Boerner K, Klinger J, Rosen J. Preparedness for death and adjustment to bereavement among caregivers of recently placed nursing home residents. J Palliat Med. 2015;18(2):127-133.
9. Cagle JG, Kovacs PJ. Informal caregivers of cancer patients: perceptions about preparedness and support during hospice care. J Gerontol Soc Work. 2011;54(1):92-115.
10. Goy ER, Carter JH, Ganzini L. Needs and experiences of caregivers for family members dying with Parkinson disease. J Palliat Care. 2008;24(2):69-75.
11. Hebert RS, Copeland VC, Schulz R, Amato CA, Arnold RM. Preparing family caregivers for the death of a loved one: implications for hospital social workers. J Soc Work End Life Palliat Care. 2008;4(4):269-285.
12. Hebert RS, Dang Q, Schulz R. Preparedness for the death of a loved one and mental health in bereaved caregivers of patients with dementia: findings from the REACH study. J Palliat Med. 2006;9(3):683-693.
13. Hebert RS, Schulz R, Copeland V, Arnold RM. What questions do family caregivers want to discuss with health care providers in order to prepare for the death of a loved one? An ethnographic study of caregivers of patients at end of life. J Palliat Med. 2008;11(3):476-483.
14. Hebert RS, Schulz R, Copeland VC, Arnold RM. Preparing family caregivers for death and bereavement: insights from caregivers of terminally ill patients. J Pain Symptom Manage. 2009;37(1):3-12.
15. Hudson P, Trauer T, Kelly B, et al. Reducing the psychological distress of family caregivers of home based palliative care patients: longer term effects from a randomised controlled trial. Psychooncology. 2015;24(1):19-24.
16. Hudson PL, Aranda S, Hayman-White K. A psycho-educational intervention for family caregivers of patients receiving palliative care: a randomized controlled trial.
J Pain Symptom Manage. 2005;30(4):329-341.
17. Shirado A, Morita T, Akazawa T, et al. Both maintaining hope and preparing for death: effects of physicians’ and nurses’ behaviors from bereaved family members’ perspectives. J Pain Symptom Manage. 2013;45(5):848-858.
18. Yoshida S, Shiozaki M, Sanjo M, et al. Pros and cons of prognostic disclosure to Japanese cancer patients and their families from the family’s point of view. J Palliat Med. 2012;15(12):1342-1349.
19. Yamashita R, Arao H, Takao A, et al. Unfinished business in families of terminally ill with cancer patients. J Pain Symptom Manage. 2017;54(6):861-869.
20. Ásgeirsdóttir HG, Valdimarsdóttir U, Fürst CJ, Steineck G, Hauksdóttir A. Low preparedness before the loss of a wife to cancer and the widower’s chronic pain 4–5 years later—a population-based study. Psychooncology. 2013;22(12):2763-2770.
21. Hauksdóttir A, Steineck G, Fürst CJ, Valdimarsdóttir U. Long-term harm of low preparedness for a wife’s death from cancer—a population-based study of widowers 4–5 years after the loss. Am J Epidemiol. 2010;172(4):389-396.
22. Janze A, Henriksson A. Preparing for palliative caregiving as a transition in the awareness of death: family carer experiences. Int J Palliat Nurs. 2014;20(10):494-501.
23. Tsai W-I, Prigerson HG, Li C-Y, Chou W-C, Kuo S-C, Tang ST. Longitudinal changes and predictors of prolonged grief for bereaved family caregivers over the first 2 years after the terminally ill cancer patient’s death. Palliat Med. 2016;30(5):495-503.
24. Hebert RS, Prigerson HG, Schulz R, Arnold RM. Preparing caregivers for the death of a loved one: a theoretical framework and suggestions for future research. J Palliat Med. 2006;9(5):1164-1171.
25. Krout RE. Music therapy with imminently dying hospice patients and their families: facilitating release near the time of death. Am J Hosp Palliat Care. 2003;20(2):129-134.
26. Angelo JK, Egan R, Reid K. Essential knowledge for family caregivers: a qualitative study. Int J Palliat Nurs. 2013;19(8):383-388.
27. Fugate J. Art therapy with family caregivers of patients with cancer. Ky Nurse. 2004;53(4):14.
28. Safrai MB. Art therapy in hospice: a catalyst for insight and healing. Art Ther. 2013;30(3):122-129.
29. Potash JS, Ho AHY, Chan F, Wang XL, Cheng C. Can art therapy reduce death anxiety and burnout in end-of-life care workers? A quasi-experimental study.
Int J Palliat Nurs. 2014;20(5):233-240.









