Post-Fall Assessment Reporting Methods in Canadian Long-Term Care Facilities
Falls are a significant problem among residents of long-term care facilities (LTCFs). Post-fall assessment (PFA) has an important role to play in recording potential risk factors so as to prevent future falls.The objective of the current study was to examine how fall incidents are recorded, the type of information gathered in the reporting forms, and how the information is used. To investigate various PFA tools and procedures for their use, telephone interviews were conducted with a staff member from 52 LTCFs in Nova Scotia, Canada. Interviewee information, facility information, fall reporting methods, and report template data were collected and analyzed. Findings showed that reporting forms mostly required information that was administrative in nature and failed to gather information on the risk factors surrounding the fall incident. Current reporting systems seem to be inadequate for identifying or addressing future fall risk. A more systematic and evidence-based approach is needed to address the issue of falls in LTCFs.
Key words: falls, seniors, long-term care, post-fall assessment, incident report
Falls, defined as “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position,” are a major cause of injury and mortality in persons aged 65 years and older.1-3 Up to one-third of seniors living in the community fall once per year; however, seniors in long-term care (LTC) settings fall more frequently, with an incidence rate up to three times higher than that of community-dwelling seniors.4-6 Studies show that over 50% of LTC residents experience at least one fall per year, with an incidence rate of approximately 1.5 falls per bed.7 Of these residents who fall, half are likely to fall multiple times.4,8,9 These falls have both physical and psychologic consequences and are costly from a personal and health systems perspective,10 accounting for billions of dollars per year in Canada.11
Consequences of falls can include minor injuries such as cuts, bruises, and sprains; major injuries requiring hospitalization, such as hip fractures; and fear of falling. Falls are responsible for 95% of all hip fractures, and 25% of individuals who suffer a hip fracture die within a 5-year period.12,13 Falls are considered to be the primary factor contributing to injury-related hospitalization of seniors in Canada.14,15 Falls are not random occurrences; many risk factors have been identified as being associated with these events. These include sex, age, medication (especially psychotropic drugs), cognitive impairment, comorbidities, environmental hazards, restraints, and previous falls.16 The risk of falling rises as the number of risk factors increase.3
Considering the ramifications of fall injuries, the need for post-fall assessments (PFAs) is evident. PFAs enable clinicians to identify the causes of falls and, more importantly, facilitate the development of prevention strategies. Currently, there is no standardized PFA tool used in LTC facilities (LTCFs). Facilities in Canada use a variety of reporting mechanisms, such as in-house report forms, charting systems, and incident reports, as well as a national system known as interRAI Minimum Data Set (MDS) 2.017 (based on an earlier version of the MDS used in the United States, which uses version 3.0), a comprehensive software suite used to chart all resident health issues, including falls. A majority of facilities still use the traditional incident report forms, however.15 It should be noted that use of the MDS is not required in Canada, although many provinces use it. In some jurisdictions, such as Nova Scotia, or at publically funded facilities, it is mandatory only at the time of intake, and follow-up MDS assessments are not required.
Studies comparing the effectiveness of assessment methods have come to conflicting conclusions. Some studies have found the accuracy of the MDS system data to be variable, being dependent on the health administration. As an illustration, studies conducted in the Veterans Health Administration found that when MDS data are consistently collected, they are reflective of medical records and are considered to be useful for administrative and research purposes.18,19 However, other studies have indicated that the MDS data used by some health districts may be underreporting falls20 and providing inadequate guidance for PFAs.21 Other reporting mechanisms have been found to be viable alternatives. For instance, Montero-Odasso and colleagues22 concluded that reporting forms with flowcharts dramatically improve falls data when compared to the incident reporting method. On the other hand, Kanten and colleagues23 found that the flowchart system may lead to some overestimation. In general, the lack of consistency and consensus among researchers in regard to a standard and reliable reporting mechanism calls into question the value of PFAs. A more systematic effort to identify effective PFA tools is necessary.
The objective of this study was to identify and evaluate existing fall reporting mechanisms in Nova Scotia LTCFs with particular emphasis on how fall incidents are recorded, the type of information gathered in the reporting forms, and how the information is used. Findings may then be used to identify or develop more effective PFA tools and reporting forms for more thorough assessments that may help to prevent future falls.
Methods
Participants and Study Design
In compliance with the Tri-Council Policy Statement concerning Ethical Conduct for Research Involving Humans, the Research Ethics Board at Acadia University approved the study design and protocol.
Nova Scotia directories for nursing homes (NHs), homes for the aged, and residential care facilities (RCFs) for older adults were obtained from the Nova Scotia Department of Health. There are a total of 136 NHs and RCFs in Nova Scotia (92 NHs and 44 RFCs). The Nova Scotia Department of Health confirmed that incident reporting protocols are developed at an individual facility level. Facilities are not required to submit incident reports to the Department of Health unless there is a major injury.
We obtained regional permission to contact 72 of the LTCFs by phone to ask if they would like to participate in the study. If given a positive response, the name of the director of care and/or nursing, another appropriate individual designated by the director of care and/or nursing, or the administrator was obtained. Given the descriptive nature of the study, no a priori sample size calculation was performed.
The telephone interview questionnaire was developed and reviewed by colleagues of the study authors (who were presently working in a LTCF or who had previous work experience in LTC) and revised accordingly before pilot testing commenced. A pilot test of the questionnaire was completed to determine the time required to complete the interview (approximately 30 minutes) and to identify questions that were potentially unclear. The pilot testing of the survey was completed with the director of care of a LTCF in another province (British Columbia). A letter of information and invitation regarding the survey and explaining the study was sent via email to prospective participants after the pilot test.
Follow-up calls were made regarding the letter of information to determine each individual’s willingness to participate in the project and to schedule a time and date that was convenient for the participant.
Interview Questionnaire
The telephone interview questionnaire was structured in the following format:
Interviewee Profiles. To obtain background information on the interviewee, a series of questions pertaining to date of birth, highest education level, specializations, current position title, and experience in the LTC field were asked of the participants.
Facility Information. Interviewees were asked to provide background information on the facility, such as ownership of the facility; length of time that the facility has been in operation; number of operational departments, units, staff, and residents; resident-staff ratios; and whether the facility has a residents’ council.
Reporting Methods. A blank incident report was requested from each facility. A literature review on any fall incident reporting protocols or forms used in LTCFs from the existing literature, as well as various risk factors for falls, was conducted using the PubMed database to develop questions on reporting fall-related incidents. Questions pertaining to the charting of the incident were also formulated for the purpose of comparing charting methods in incident reports for recording fall-related incidents. Information on auditing of charts and incident reports for the number of falls and the circumstances surrounding falls were included to help determine how many facilities are currently calculating statistics on falls.
Data analysis was performed using statistical software (SPSS 26 for Windows).24
Results
Participants from 52 LTCFs agreed to be interviewed for the study. Each interview was approximately 30 minutes long.
Interviewee Profiles
Of the individuals who completed the survey for their respective facilities (N = 52), all but one of the respondents were female (n = 51, 98%). The majority of interviewees (n = 43, 82.7%) had either a BSc in Nursing or a Diploma in Nursing, and more than half of participants (n = 29, 55.8%) had no other primary specialization; nine survey participants (17.3%) had a certificate in Gerontology, while six (11.6%) had credentials in Management or Healthcare Management and Leadership. An additional two respondents had a diploma in Long-Term Care Management. Regarding their position at the facility, the majority held the position of director of nursing (n = 12, 23.1%), director of care (n = 14, 26.9%), or director of resident care (n = 8, 15.4%). Several of the interviewees held another position at the facility, primarily as a staff registered nurse (RN; n = 18, 34.6%) or RN supervisor (n = 5, 9.6%).
Facility Information
As shown in Table 1, nearly 54% of the facilities (n = 28) were located in a rural setting, while 46% were based in urban centers (n = 24). Most facilities (n = 36, 69%) were municipally owned and not-for-profit, while only 31% (n = 16) were run privately and for profit. The amount of time that each facility had been in operation varied greatly, ranging from 0.25 to 60 years, with a mean of 22.7 years.
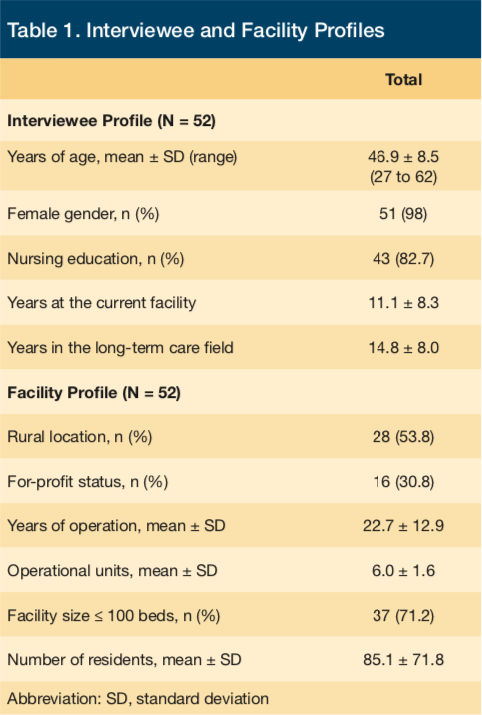
The facilities also varied in size and capacity, ranging from 1 to 11 departmental units with an average of 3 units (eg, nursing, therapies, dietary) and housing between 14 to 440 residents (mean 85 resident beds). It was reported that the average staff-resident ratio was 1:5 for day shifts, 1:7 for evenings, and 1:13 for nights. In addition, all but one facility (n = 51, 98%) had a resident council, with the size ranging from 1 to 18 members. The average number of admissions per year was 25.78 among the facilities that responded (N = 41 for these data as the other 11 cases reported a value of zero for their yearly admission rate).
Reporting Methods
The overwhelming majority (n = 48, 92.3%) of interviewees reported that falling was an issue at their facility, though the extent to which it was perceived as a problem varied greatly. When asked when and where falls were most likely to occur, the most frequently cited place for falls was the resident’s room (n =22, 42.2%), followed by the bathroom (n = 11, 21.1%), hallways (n = 2, 3.8%), dining areas (n = 1, 1.9%), and the outdoor courtyard (n = 1, 1.9%). Regarding time of day, 40.4% of respondents (n = 21) felt that evening or night time was the most high-risk period, followed by day time (n = 7, 13.5%) and early morning (n = 4, 7.7%). Only 11.5% reported that they had not observed any pattern (n = 6). It should be noted that the responses to these questions are not mutually exclusive (ie, some individuals reported both bedrooms and bathrooms to be high-risk areas).
All facilities used PFA reports; 98% of respondents (n = 51) stated that all falls require an incident report, with one facility using them only in cases requiring medical attention or hospitalization. Approximately 79% of respondents (n = 41) also indicated that the reports remain within the facility; while 11.5% said that they were distributed to pertinent parties if hospitalization was required (n = 6). In all cases, the report was completed by the witness to the event; in 94.2% of facilities (n = 49), the report was completed by an additional person as well, usually an RN.
Furthermore, 96.1% of respondents (n = 50) stated that reports were reviewed on a regular basis, most often by the director of care/nursing (n = 17, 32.7%). The frequency of the report review ranged from weekly (n = 1, 1.9% of cases) to quarterly (n = 9, 17.3% of cases), with 23 facilities (45.1%) reviewing them once a month. Approximately 4% of respondents (n = 2) stated that the reports were never reviewed, and 21.2% conducted reviews on an individual basis (n = 11).
Of all of the facilities recording falls in the resident’s chart, only 20 (38.5%) flagged the incidents. The person charting the incident was most often the witness to the event (n = 27, 51.9% of cases), with RNs, licensed practical nurses, and physiotherapists conducting the charting at the remaining facilities (n = 20, 38.5%). Lastly, 40 (76.9%) facilities completed a falls audit on a regular basis, although the frequency of the audit varied from once per month (n = 20, 38.5%) to once per year (n = 7, 13.5%). Of those 40 facilities that reported completing audits, 32 (80%) of them did so at least once every 3 months.
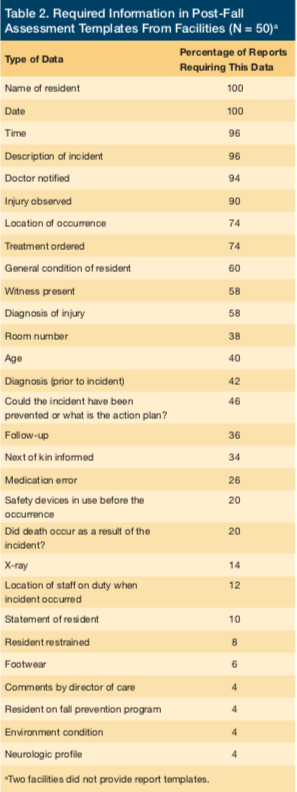
Only 50 of the 52 facilities sent examples of their PFA reporting forms when requested. The type of data included in the report templates is summarized in Table 2. Most commonly required information in report templates were administrative in nature, including the name of the resident, date and time, description of the incident, injury observed, doctor notified, and treatment ordered in 74% or more of the templates (n = 37). Very few report templates asked for information on the risk factors surrounding a fall incident. For example, only 4% of incident reports (n = 2) asked for information related to the environmental condition or neurologic profile, and only 6% included information on footwear (n = 3). None included information on mobility and balance issues or other well-known risk factors for falls.
Discussion
The data obtained show that, in general, PFA reporting forms in Nova Scotia LTCFs lack the systematic rigor necessary to provide consistent information about falls and their causes. This limits their effectiveness as a means of fall prevention. A more systematic and evidence-based approach is needed to address the significant issue of falls in LTCFs.
PFA tools have an important role to play, not only in providing documentation required for legal purposes, but also in recording information that may be critical in identifying risk factors. Current reporting systems, however, are widely varied and are often informal, capturing inconsistent data with no systematic approach to fall assessment. This type of unstandardized reporting, while perhaps sufficient from a legal standpoint, offers little-to-no insight to addressthe root causes of falls and to provide guidance or means of preventing such incidents in the future. Because falls continue to be an ongoing, costly, and often deadly issue in LTC, it is in everyone’s best interest to ensure that systematic, standardized PFA tools are being created and implemented to reach their full potential.
Furthermore, the disconnect between what data administrators believe their reports record and what is actually recorded suggests that more must be done to not only ensure risk factors are included, but to ensure that these reports become user-friendly, systematic, and standardized. For example, some administrators reported recording fall risk factors and environment surrounding a fall (eg, time). However, this information was not evident from the fall report template. While it is possible that the contextual information may be in the notes section, it may not be readily and easily identified in any follow-ups.
Two primary recommendations emerge from the findings of the present study for practical application. First, given the wide use of post-fall reports, it is important for facilities to consider maximizing their use to prevent future falls. For example, facilities would be well served to create processes to review and incorporate information from PFA reports into the care plan for the residents and to inform programs and policies at the institutional level (eg, restraint policy, falls prevention program). Although a wealth of data is available at facilities from post-fall reporting and system tools, such as the MDS, advantage is not taken of the data to influence resident-level care or the facility-level programs and policies.
The second recommendation is for facilities to consider the use of an evidence-based PFA tool that records an adequate level of information for action to emerge from the data. Specifically, the current systems often do not capture the risk factors surrounding the fall. It is recommended that facilities choose the most appropriate PFA for their facility, which will give meaningful information for action.
In the jurisdiction of Nova Scotia, interRAI MDS 2.0 is used for charting all resident health problems at including falls and injuries. (Again, we should note that mandatory use of MDS varies by jurisdiction in Canada.) Yet, the MDS 2.0 has several inadequacies as a stand-alone instrument regarding falls. Firstly, the MDS only reports whether an individual has fallen at any time within the past 30 to 180 days. Therefore, falls “prevalence” captured by the MDS only represents the number of people who fell within a specific time period (ie, the prevalence of fallers) rather than the prevalence, nor incidence, of falls. Moreover, there is no indication of the number of times a person has actually fallen. Thus, it is not possible to use the MDS by itself to identify clinically different populations, such as infrequent fallers and recurrent fallers.
Secondly, the MDS is also unable to provide clinically important information regarding the level of injury sustained by the fall and is also unable to identify environmental factors that contribute to the fall incident. Furthermore, falls are not specifically defined in the MDS support documentation, which is crucial for any falls prevalence/incidence instrument. Thus, specific types of falls reported by a facility in the MDS may or may not be reported across facilities.
Finally, while the information available from the MDS may provide information about the intrinsic or host factors associated with falls (ie, mobility, disease diagnosis, daily routine, medication groups), MDS data cannot provide a meaningful description of fall incidents themselves. This results primarily from the varying time frames found in the numerous sections of the MDS. There is no way to ascertain from MDS data whether the fall occurred in the same time period that one is attempting to correlate with some other dimension within the MDS (eg, the fall may have occurred prior to the 7-day period assessed for medication), which may lead to spurious correlations.
Using a menu-driven falls incident reporting system that is systematic rather than narrative has been shown to improve fall documentation in both traditional charting and in the MDS.25 This method results in significantly better documentation of fall characteristics, although there have been implementation issues in some studies.26 A 2007 study of a LTCF in Quebec suggests that the use of a flowchart system to classify all residents as occasional or recurrent fallers can significantly improve what is known about a resident’s fall history and where falls take place.22
Other PFA tools have also been investigated. These tools, such as the post-fall index, move beyond mere incident reporting and attempt to identify the etiology of the fall incident. One PFA tool, the post-fall index, has been shown to be comprehensive, reliable, and valid in LTC populations.21 PFA tools are believed to detect many remediable fall causes such as orthostatic hypotension, muscular weakness, environmental hazards, pharmacologic side effects, and gait issues.21 However, PFA tools are mostly unavailable to NH staff, as fall risk assessment tools are typically used instead.21
Conclusion
The PFAs currently in use in the surveyed Nova Scotia LTCFs are not used to maximize the tracking of the rates and risk factors in a systematic way and to prevent future falls. PFA has an important role to play in improving resident-level care as well as institution-level programs and policies in this area. The present study highlights the need for a more systematic and evidence-based approach to address the significant issue of falls in LTCFs. It is hoped that the present study will serve as a catalyst to promote dialogue and action related to PFA and the use of information to maximize resident care to prevent future falls.
References
1. American Geriatrics Society, British Geriatrics Society. Clinical practice guidelines: prevention of falls in older persons. https://www.medcats.com/FALLS/frameset.htm. New York, NY: American Geriatrics Society, 2010. Accessed July 21, 2017.
2. Barbosa FA, del Pozo-Cruz B, del Pozo-Cruz J, Alfonso-Rosa RM, Sanudo Corrales B, Rogers ME. Factors associated with the risk of falls of nursing home residents aged 80 years or older. Rehabil Nurs. 2016;41(1):16-25.
3. Public Health Agency of Canada. Seniors’ falls in Canada: second report. PHAC website. https://www.phac-aspc.gc.ca/seniors-aines/publications/public/injury-blessure/
seniors_falls-chutes_aines/index-eng.php. Updated 2014. Accessed July 21, 2017.
4. Becker C, Rapp K. Fall prevention in nursing homes. Clin Geriatr Med. 2010;26(4):693-704.
5. Pearson C, St-Arnaud J, Geran L. Understanding seniors’ risk of falling and their perception of risk. Statistics Canada website. https://www.statcan.gc.ca/pub/82-624-x/2014001/article/14010-eng.pdf. Published October 2014. Accessed July 28, 2017.
6. World Health Organization. Global Report on Falls Prevention in Older Age. WHO website. https://www.who.int/ageing/publications/Falls_prevention7March.pdf. Published 2008. Accessed July 24, 2017.
7. Bonner AF. Falling in to place: a practical approach to interdisciplinary educational falls prevention in long-term care. Annals of Long-Term Care: Clinical Care and Aging. 2006;14(6):21-29.
8. Kannus P, Parkkari J, Niemi S, Palvanen M. Fall-induced deaths among elderly people. Am J Public Health. 2005;95(3):422-424.
9. Scott V, Wagar B, Sum A, Metcalfe S, Wagar L. A public health approach to fall prevention among older persons in Canada. Clin Geriatr Med. 2010;26(4):705-718.
10. Centers for Disease Control and Prevention (CDC). Cost of falls among older adults. CDC website. https://www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html. Updated August 19, 2016. Accessed July 31, 2017.
11. Parachute. The cost of injury in Canada. Toronto, ON: Parachute, 2015. https://www.parachutecanada.org/downloads/research/reports/EBI2009-Eng-Final.pdf. Accessed July 31, 2017.
12. Ioannidis G, Papaioannou A, Hopman WM, et al. Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ. 2009;181(5):265-271.
13. Wolinsky FD, Bentler SE, Liu L, et al. Recent hospitalization and the risk of hip fracture among older Americans. J Gerontol A Biol Sci Med Sci. 2009;64(2):249-255.
14. Accreditation Canada, Canadian Institute for Health Information, Canadian Patient Safety Institute. Preventing falls: from evidence to improvement in Canadian health care. Accreditation Canada website. accreditation.cahttps://s3.amazonaws.com/HMP/hmp_ln/imported/falls-joint-report-2014-en.pdf. Published 2014. Accessed July 24, 2017.
15. Canadian Institute for Health Information. Injury, hospitalizations & socio-economic status. CIHI website. https://secure.cihi.ca/free_products/Injury_aib_vE4CCF_v3_en.pdf. Published June 2010. Accessed July 24, 2017.
16. Hill KD, Wee R. Psychotropic drug-induced falls in older people: a review of interventions aimed at reducing the problem. Drugs Aging. 2012;29(1):15-30.
17. interRAI Organization. Long-Term Care Facilities (LTCF) Assessment System. interRAI website. https://www.interrai.org/long-term-care-facilities.html. Accessed July 24, 2017.
18. Wolfsfeld L, Wang M, Pizer S. Validating MDS from VA nursing home care units: data appears to be internally consistent and reliable. Health Care Financing and Economics website. https://www.hcfe.research.va.gov/docs/db_2004_01.pdf. Published October 13, 2004. Accessed July 24, 2017.
19. Frakt A, Wang M, Pizer S. Validating MDS data from VA nursing home care units: comparing MDS data with PAF and NPCD sources. Health Care Financing and Economics website. https://www.hcfe.research.va.gov/docs/db_2004_02.pdf. Published October 13, 2004. Accessed July 24, 2017.
20. Hill-Westmoreland EE, Gruber-Baldini AA. Falls documentation in nursing homes: agreement between the Minimum Data Set and chart abstractions of medical and nursing documentation. J Am Geriatr Soc. 2005;53(2):268-273.
21. Gray-Miceli DL, Strumpf NE, Johnson J, Graganescu M, Ratcliffe SJ. Psychometric properties of the post-fall index. Clin Nurs Res. 2006;15(3):157-176.
22. Montero-Odasso M, Levinson P, Gore B, Tremblay L, Bergman H. A flowchart system to improve fall data documentation in a long-term care institution: a pilot study. J Am Med Dir Assoc. 2007;8(5):300-306.
23. Kanten DN, Mulrow CD, Gerety MB, Lichtenstein MJ, Aguilar C, Cornell JE. Falls: an examination of three reporting methods in nursing homes. J Am Geriatr Soc. 1993;41(6):662-666.
24. IBM developerWorks. IBM SPSS Statistics. IBM website. ibm.co/2whzCGx. Updated March 3, 2016. Accessed July 24, 2017.
25. Wagner LM, Capezuti E, Clark PC, Parmelee PA, Ouslander JG. Use of a falls incident reporting system to improve care process documentation in nursing homes. Qual Saf Health Care. 2008;17(2):104-108.
26. Wagner LM, Capezuti E, Taylor JA, Sattin RW, Ouslander JG. Impact of a falls menu-driven incident-reporting system on documentation and quality improvement in nursing homes. Gerontologist. 2005;45(6):835-842.










