OPTIMISTIC Transition Visits: A Model to Improve Hospital to Nursing Facility Transfers
Transitions to and from hospitals and nursing facilities (NFs) expose patients to lapses in care due to miscommunication. Potential consequences of these breakdowns in communication include medication errors, poor follow-up care after transitions, and rehospitalization. In 2012, the Centers for Medicare & Medicaid Services decided to fund an initiative made up of seven projects to re- duce potentially avoidable hospital transfers. One of the these projects, the Op- timizing Patient Transfers, Impacting Medical Quality, and Improving Symptoms: Transforming Institutional Care (OPTIMISTIC) project, implements registered nurs- es and nurse practitioners to assist with and close gaps in transitions of care for NF patients. The authors provide an overview of the transition visit model and a preliminary analysis of the outcomes of their interventions.
Key words: transitional care, nursing home transfers, medication reconciliation, quality improvement
Nursing facility (NF) residents face many transitions, including transitions to and from hospitals.1 These transitions are high-risk windows for communication breakdown and for poor outcomes such as medication errors, inadequate follow-up care, family dissatisfaction with care, untreated pain, and hospitalizations.2,3 One report analyzed records of several hundred residents for the first 32 days after hospital-to-NF transfers and concluded that 33% of these residents faced harm due to care that was “poor” and “dangerous.”4 The report advocated for novel approaches to eliminate the potential harm faced by these residents.
In 2012, the Centers for Medicare & Medicaid Services (CMS) Center for Innovation funded seven, 4-year demonstration projects targeted to improve care for long-stay NF residents.5 The primary goal of the initiative is the reduction of potentially avoidable hospital transfers, but all projects are expected to include elements to improve the safety of transfers that do occur.
The OPTIMISTIC (Optimizing Patient Transfers, Impacting Medical Quality, and Improving Symptoms: Transforming Institutional Care) project, one of the seven funded projects, has embedded a registered nurse (RN) in each of 19 partnering facilities.6 This RN facilitates data collection, INTERACT implementation, quality improvement initiatives (eg, behavior management or advance care planning), and provides urgent care in collaboration with the facility staff. The project is also supported by six nurse practitioners (NPs) who assist in providing many evidence-based elements to improve care on multiple fronts including proactive chronic care management, urgent care, and robust transitional care services.
Visit processes were designed by the project medical core members, including the project medical director (AN), within the first 6 months of the project. Pilot testing by two NPs provided valuable feedback and led to the refinement of the visit templates. Subsequently, all OPTIMISTIC clinical staff were trained regarding these visits, who then educated the staff in the partnering NFs. Feedback from many of the medical providers in the partnering facilities was sought to further modify the processes.
In this paper, we provide an overview of the transition visit model and a preliminary analysis of the interventions with the objective to: (1) describe the sources and nature of actual and potential problems in hospital to nursing home care transitions; and (2) discuss OPTIMISTIC strategies for addressing these problems in a proactive manner.
Methods
Participants
All long-stay NF residents in the partnering facilities are passively enrolled in the demonstration project. Participants enrolled in a Medicare managed care program are considered ineligible. Eligible participants, or their representatives, were notified about the project by mail and provided with the option to opt-out of the program, per CMS guidelines. So far, less than 1% of residents have opted out. Long-stay was defined by CMS as greater than 100 days in the facility or an indication on the Minimum Data Set that there is no active or documented plan for discharge to the community. The analysis was approved by the Indiana University Institutional Review Board.
Study Design
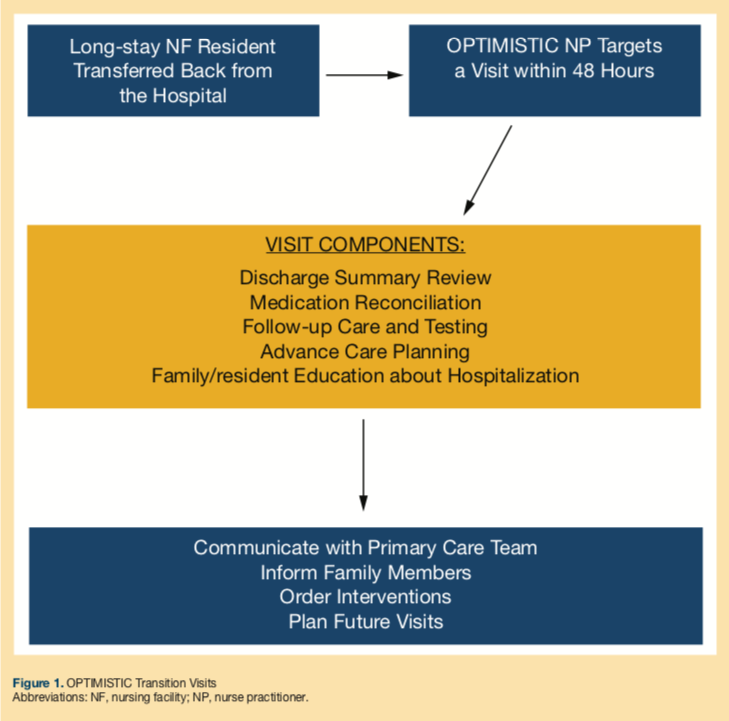
NP transition visits represent the core element of the transitional care services for the initiative and are depicted in Figure 1. These visits focus on high-risk aspects of hospital-to-facility transitions and facilitate availability of accurate discharge summaries, medication reconciliation, resident and family education, follow-up on appointments and tests, and advance care planning. NPs aim to perform a relevant and focused examination to address above-mentioned elements within 48 hours of hospital discharge. The NPs procure missing discharge summaries and, if needed, call the discharge team at the hospital to retrieve the missing information. Access to electronic health records (EHRs) for major hospitals assists in the retrieval of crucial information. Any new interventions or changes in the management plans are conveyed to the primary care teams for the NF resident. The visit notes summarize all the efforts as well as recommended and approved (by primary care teams) interventions and are placed in or scanned into the patient records. The project NPs then enter all the orders for approved interventions. The NPs sign-out pending care issues and ongoing resident monitoring to the OPTIMISTIC nurses. NP transition visits do not replace the primary care provider return visits.
Data Collection
The project team is utilizing REDCap, a secure web application for managing project data. The NPs log each transition visit as an encounter. Information captured for each transition visit includes patient demographics, primary and secondary diagnoses, and any ordered interventions. They label each intervention as medication-related or non-medication related and also categorize it as one of three categories: (1) treatment modification (eg, discontinuing a medicine due to duplication or dose adjustment due to renal dysfunction); (2) monitoring and follow-up; or (3) new treatment order (eg, adding a pain medication for a patient with uncontrolled pain). The project medical director (AN) did case-based training with all of the NPs on how to classify interventions using these categories. The RedCap database was populated with the most common interventions (using drop down menus) under these three categories for standardizing the selection of these interventions. During the pilot phase of the implementation of this database, the project medical director and the NPs modified these drop down menus. Unless an intervention addresses a new health need since readmission, the NPs attribute the need for each intervention to the discharging hospital, facility, primary care team, or facility staff based on clinical judgment and review of the medical record. The attributions are based on available medical records at the time of the visit.
Data Analysis
The analyses provided here are based on visits that occurred between January 2015 and July 2015. During that time frame, OPTIMISTIC had 2548 eligible residents. NP transition visits were initiated for OPTIMISTIC residents starting in September 2013, but more complete descriptive data regarding transfers was collected starting in January 2015.
Results
There were a total of 297 residents that had one transfer and 118 residents with multiple transfers, for a total of 597 transfers back to the 19 partnering facilities during the study period. NPs were able to complete transition visits for 515 (86%) of these transfers within a mean timeframe of 3.8 days. These transition visits accounted for 377 unique residents. Each NP completed an average of 27 transition visits per month, spending an average of 102 minutes per visit (Table 1). Discharge summaries were available for 70% of residents returning to the facility, and NPs were able to obtain summaries for an additional 21% of returning residents. NPs captured summaries by accessing hospital EHRs or calling hospitals and requesting them. A total of 279 visits (54.2%) required an intervention of some kind. A medication-related intervention was needed for 37% of visits. The NPs selected category 1 (treatment modification) for 31% of the visits, category 2 (monitoring and follow-up) for 27%, and category 3 (new treatment) for 23% of the visits.
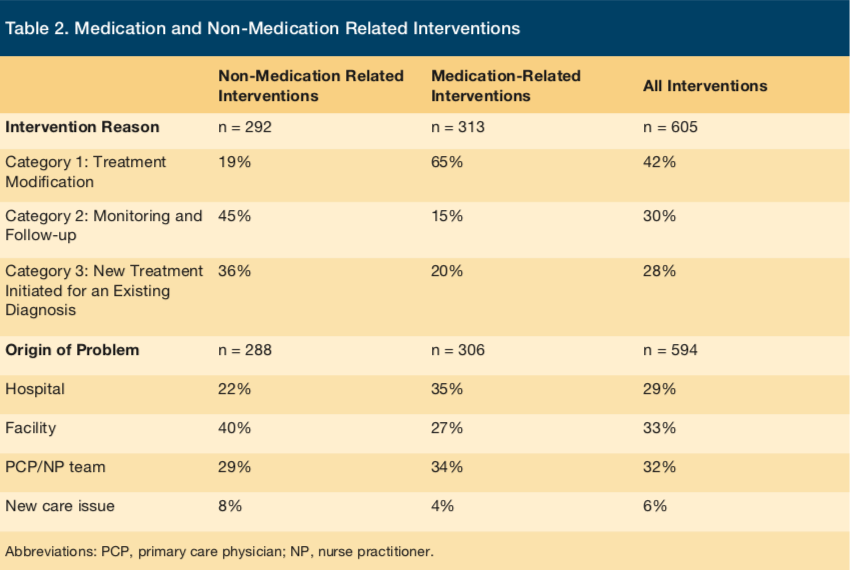
Forty-two percent of interventions recommended by the NPs were in category 1, 30% were in category 2, and 28% were in category 3 (Table 2). A majority of the medication-related interventions (65%) were needed to adjust medication class or dose due to patient comorbidities and 15% and 20% to address monitoring and untreated diagnoses, respectively.
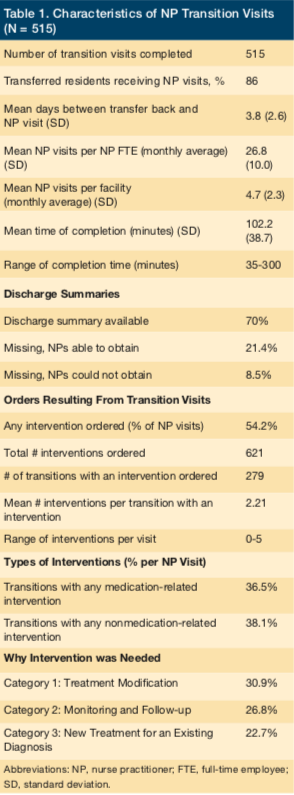
After the NPs had traced the source of care problems leading to the interventions, 29% were traced back to the hospital, 33% to the facility, and 32% to medical providers. Only 6% of the interventions were needed due to a new care issue that had emerged since the transfer. Among medication-related interventions (not reported in Table 2), the most frequent classes involved were pain medications (24%), antiplatelet/anticoagulation medications (13%), psychotropics (10%), and antihypertensives (9%). Thirty percent of all non-medication interventions were needed to plan physician follow-up care or to order a needed follow-up lab test.
Discussion
We describe a proactive and evidence-based approach led by NPs that enables key transitional care processes during hospital-to-facility transfers for long-stay NF residents. A unique reporting structure facilitated a better understanding of the nature and origin of potential problems during these transfers. Our results confirm that transition of residents with complex medical problems results in problems related to medications, follow-up care, and monitoring. A report from the Office of the Inspector General (OIG) explained that the majority of preventable harm faced by residents transferred to NFs belong to one of these three categories.4
A majority of the visits required an intervention, confirming previous findings that transitions of frail NF residents are far from perfect.7,8 Inadequate communication between hospitals and NFs is a known source of transitional care issues.9 Lack of availability of discharge summaries for almost one-third of the subjects is a clear illustration of communication breakdown. The intervention countered this barrier by retrieving missing discharge summaries and also by establishing verbal contact with medical teams at various hospitals, thus assuring that all parties were on the same page. This, however, is time-intensive and would be unnecessary if hospitals standardized the timely delivery of critical information with discharge.
Studies show that medication-related harm occurs during and after hospital transitions.8,10,11 Many factors contribute to such harm, including poor communication, imprecise documentation, and transcription errors as well as problems with prescribing, dispensing, and monitoring.7,11-13 In this analysis, more than half of the required interventions were medication-related, and 37% of the visits required a medication-related intervention. In a majority of these cases, an intervention was required to adjust prescribed medicine or dosage. Interventions requiring adjusting doses of anticoagulants—a high-risk medication class—were the most frequent in our analysis, which is similar to previous studies regarding transitions.11
Eighty percent of the 304 non-medication-related interventions addressed follow-up care or added new treatments to an existing but untreated diagnosis. This is similar to other studies that found many “loose ends” need to be addressed concerning transfers from hospitals to NFs.2,14 We theorize that, in the absence of these focused transition visits, many of the follow-up interventions may have been overlooked, resulting in possible harm to these residents. The OIG report on adverse events in skilled facilities calculated that more than 23% of the NF patients faced serious harm due to poor care within a few weeks after transfer to a NF, resulting in hospitalizations and mortality among these patients.4
Our results highlight that less-than-ideal transitions and ensuing outcomes are a result of communication issues across the continuum. Medication-related interventions were more often attributed to hospitals whereas non-medication interventions were more commonly attributed to the facilities. OPTIMISTIC NPs were able to identify potentially serious errors and omissions in care and address them proactively by establishing high-quality communication channels with the discharging teams, primary care teams, and facility staff. The project team is currently exploring mechanisms to establish relationships with the area hospitals in order to facilitate quality improvement regarding identified transitional care issues.
This analysis also highlights the need for hospital teams to invest in high-quality mechanisms for medication reconciliation and to assess quality of prescribing. A pharmacist with expertise in geriatric prescribing could take the lead in ensuring high-quality prescribing across settings. Such programs have already shown promise for hospital-to-home transitions.15,16 Facilities also need to ensure that medication reconciliation is a high-priority activity that occurs systematically after each admission or readmission to a facility. Medical directors who are trained and certified in quality improvement can help implement strategies for effective reconciliation approaches and also train personnel to facilitate these processes.
This analysis has some limitations. First, the sample includes residents from 19 NFs in the Indianapolis urban area and may not be generalizable to all NFs, particularly those in rural settings. Second, many of the hospital systems in Indianapolis are participating in shared-saving demonstration programs and have instituted systems to improve transitional care processes. Thus, our numbers may be an underrepresentation of the issues surrounding transfers in the broader population. But our approach to study the care these residents received during these transitions was unique. Project NPs were able to assess nearly 90% of the residents within 4 days of transfer and systematically collected data including categorization of interventions needed, and they put those interventions in place. This is in contrast to previous studies where retrospective chart reviews provided such information. This analysis does not include the impact of our approach on health outcomes including transfer back to hospitals or emergency department visits. In our subsequent analyses, we aim to address the potential impact of our approach on re-hospitalizations.
Conclusion
This analysis provides additional context for the myriad of transitional care issues faced by NF residents transferring back from the hospital. It highlights key areas of potential quality improvement around transitions, including medication management and follow-up care, which could be addressed by proactive systems. The analysis further underlines the need for better collaboration among health settings to improve care. The OPTIMISTIC transition visit approach, led by an NP well versed in the principles of geriatric and transitional care, is one possible strategy to improve resident care processes. Our future analyses of this model will address the estimation of potential cost-savings by preventing harm, including exploration of the business case for broader dissemination of this approach.
1. Callahan CM, Tu W, Unroe KT, LaMantia MA, Stump TE, Clark DO. Transitions in Care in a Nationally Representative Sample of Older Americans with Dementia. J Am Geriatr Soc. 2015;63(8):1495-1502.
2. Caruso LB, Thwin SS, Brandeis GH. Following up on clinical recommendations in transitions from hospital to nursing home [published online ahead of print February 9, 2014]. J Aging Res. doi:10.1155/2014/873043.
3. Eslami M, Tran HP. Transitions of care and rehabilitation after fragility fractures. Clin Geriatr Med. 2014;30(2):303-315.
4. Levinson D; US Department of Health and Human Services. Adverse Events in Skilled Nursing Facilities: National Incidence Among Medicare Beneficiaries. Rep. OEI-06-11-00370. http://oig.hhs.gov/oei/reports/oei-06-11-00370.pdf. Published February 2014. Accessed September 18, 2015.
5. Centers for Medicare & Medicaid Services. Initiative to Reduce Avoidable Hospitalization Among Nursing Facility Residents. CMS Web site. http://go.cms.gov/1QNwsfG. Updated March 24, 2016. Accessed September 18, 2015.
6. Unroe KT, Nazir A, Holtz LR, et al. The Optimizing Patient Transfers, Impacting Medical Quality, and Improving Symptoms: Transforming Institutional Care approach: preliminary data from the implementation of a Centers for Medicare and Medicaid Services nursing facility demonstration project. J Am Geriatr Soc. 2015;63(1):165-169.
7. Boockvar KS, Liu S, Goldstein N, Nebeker J, Siu A, Fried T. Prescribing discrepancies likely to cause adverse drug events after patient transfer. Qual Saf Health Care. 2009;18(1):32-36.
8. LaMantia MA, Scheunemann LP, Viera AJ, Busby-Whitehead J, Hanson LC. Interventions to improve transitional care between nursing homes and hospitals: a systematic review. J Am Geriatr Soc. 2010;58(4):777-782.
9. Shah F, Burack O, Boockvar KS. Perceived barriers to communication between hospital and nursing home at time of patient transfer. J Am Med Dir Assoc. 2010;11(4):239-245.
10. Boockvar K, Fishman E, Kyriacou CK, Monias A, Gavi S, Cortes T. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med. 2004;164(5):545-550.
11. Desai R, Williams CE, Greene SB, Pierson S, Hansen RA. Medication errors during patient transitions into nursing homes: characteristics and association with patient harm. Am J Geriatr Pharmacother. 2011;9(6):413-422.
12. Santell JP. Reconciliation failures lead to medication errors. Jt Comm J Qual Patient Saf. 2006;32(4):225-229.
13. Cua YM, Kripalani S. Medication use in the transition from hospital to home. Ann Acad Med Singapore. 2008;37(2):136-136.
14. Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311.
15. Holland DM. Interdisciplinary collaboration in the provision of a pharmacist-led discharge medication reconciliation service at an Irish teaching hospital. Int J Clin Pharm. 2015;37(2):310-319.
16. Bajorek BV, Krass I, Ogle SJ, Duguid MJ, Shenfield GM. Optimizing the use of antithrombotic therapy for atrial fibrillation in older people: a pharmacist-led multidisciplinary intervention. J Am Geriatr Soc. 2005;53(11):1912-1920.










