Maintaining Oral Health in Palliative Care Patients
Palliative care dentistry has been defined as the evaluation and management of patients with active, progressive, advanced disease in whom the oral cavity has been compromised either by the disease directly or by its treatment. The focus of care in these patients is on quality of life. Palliative care dentistry may play an important role in the general healthcare of terminally ill patients. These patients are susceptible to oral problems that lead to oral dysfunction, which can cause unnecessary pain and discomfort, affecting the patient’s quality of life. The literature suggests that physicians and nurses generally tend to direct less attention to the patient’s mouth than to other parts of his or her body. The purpose of this manuscript is to summarize the current information about the most common oral problems of patients receiving palliative care and to discuss their prevalence, etiology, and management recommendations.
Key words: Quality of life, palliative care, dental care, terminal care, hospice care.
The World Health Organization has defined palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”1 According to the National Hospice and Palliative Care Organization,2 the number of US patients receiving hospice care increased from ~1.3 million in 2009 to ~1.5 million in 2013. The trend toward increasing numbers is expected to continue.2 Palliative care dentistry has been defined as the evaluation and management of patients with active, progressive, advanced disease in whom the oral cavity has been compromised either by the disease directly or by its treatment, with a focus on quality of life.3 Care therefore involves tending to not only the patient’s physical needs, but also his or her emotional and spiritual needs as well as those of the family. Palliative care dentistry may play an important role in the general healthcare of terminally ill patients. These patients are susceptible to oral problems that may lead to oral dysfunction, which can cause unnecessary pain and discomfort, thereby affecting their quality of life.4
Literature suggests that physicians and nurses generally tend to direct less attention to a patient’s mouth than to other parts of his or her body.5,6 These studies also show that hospice patients often do not report oral problems to their physicians and perceive treatment options as being limited. Even a new telephone hotline for healthcare professionals to assist in answering their palliative care–related clinical questions is focused only on medical questions and not dental questions.7
Knowledgeable general dentists are likely to be well suited to provide the appropriate care. General dental practitioners have important roles in managing the palliative patients. Through a careful dental screening, oro-dental conditions (teeth and gingival pathology) that might generate acute complications and compromise the medical care should be eliminated. During the hospitalization periods, professional advise about providing oral care for these patients should help minimize the complications associated with treatment; this is an area situated outside the sphere of expertise for most of the dentists.8 Following general treatments, the patients will return to their dentists, who will provide continuous assessments and dental care in order to maintain their oral health and prevent the long-term complications of medical treatment.
The purpose of this manuscript is to summarize the current information regarding the most common oral problems of patients receiving palliative care, their prevalence and etiology, and recommendations for their management. We conducted a literature review consisting of electronic MEDLINE® and PubMed® database searches using the following key words: quality of life, palliative care, dental care for chronically ill, terminal care, and hospice care. Reference lists in articles initially selected were searched for relevant additional sources. The overall effort was to identify references that reported on studies with larger study samples or reported consensus about relevant issues.
Oral Health Problems
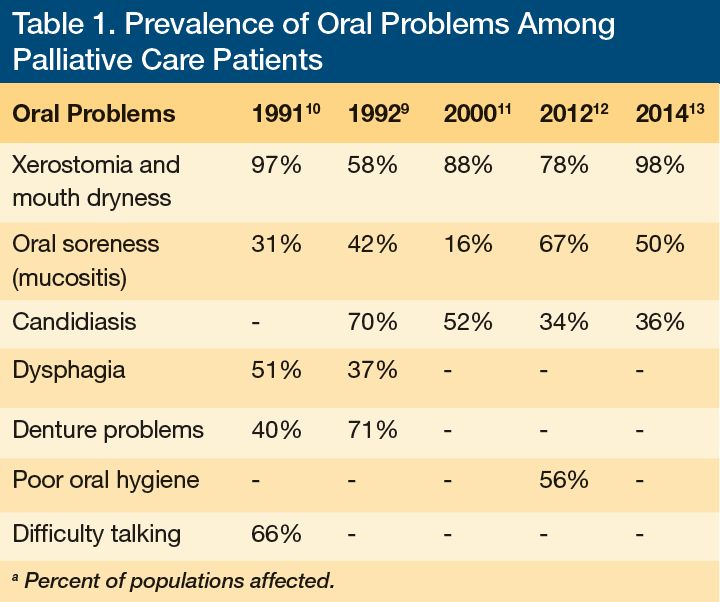
Our literature review resulted in five studies that reported on the prevalence of oral problems among palliative care (end-of-life, terminally ill) patients. The identified problems (ie, xerostomia and mouth dryness, mucositis, candidiasis, dysphagia, difficulty talking, denture problems, poor oral hygiene) and their prevalences among palliative care patients are displayed in Table 19-13 and will be described in some detail.
Xerostomia and Mouth Dryness
Xerostomia is defined as “the subjective sensation of dryness of the mouth.”14 Studies on the prevalence of xerostomia in the general population and in palliative care patients, such as those with advanced cancer, report rates between 22% and 26%15,16 and between 58% to 98%, respectively.9-13 Although xerostomia is a relatively common symptom in patients with cancer, there is little research on the condition among those with or without cancer who are receiving palliative care. It has been described as “the orphan topic in supportive care.”17
An evaluation for xerostomia can include simply asking the patient, “Does your mouth feel dry?”18 In the authors’ experience, adding the qualifier “…a lot of the time?” to this question can help to differentiate those with occasional symptoms with expected etiologies, such as the feeling of dryness on waking, from those with more chronic symptoms. The term mouth dryness is more properly used for an actual, measurable decrease in salivary flow. The most frequently cited causes of mouth dryness are anxiety, dehydration, hyposalivatory medications, certain disease conditions (eg, diarrhea, hemorrhage, vomiting), radiotherapy, and chemotherapy.19 A screening test for actual mouth dryness involves gently holding a dental mouth mirror against the inside of the patient’s cheek; mouth dryness is likely if the mirror sticks instead of sliding.20 Efforts to detect a relationship between xerostomia and mouth dryness have been elusive. Dawes20 found that healthy individuals report the sensation of dry mouth (xerostomia) when their unstimulated salivary flow rate falls by 40–50%.
The primary goals for the management of xerostomia and mouth dryness are to relieve the symptoms and, in the case of actual dryness, to address the underlying causes.21 The most common and simplest recommendation for treating these conditions is to drink or take sips of water or to suck on ice chips. An old-fashioned atomizer can be used to spray tap water into the patient’s mouth; the volume of water carried in the mist can be titrated to avoid pooling and noisy aspiration or water overload.22
Additional recommendations that can be employed by palliative care patients are presented in Table 2.19,20,22-27 These can be used individually or in combination as needed.

Generalized Oral Soreness (Mucositis)
Several studies report that between 16% and 67% of individuals receiving palliative care report mouth pain.9-13 Mucositis is a frequent cause of mouth soreness, particularly among patients undergoing cancer treatment. If present, symptoms typically start approximately 5–10 days after the initiation of treatment.8 The regions most affected are the mobile parakeratinized mucosal tissues (buccal mucosa, labial mucosa, soft palate, lateral tongue, and floor of the mouth), which have a high cell turnover rate. Conversely, the orthokeratinized epithelium (gingiva and hard palate) has lower cell turnover rates.8
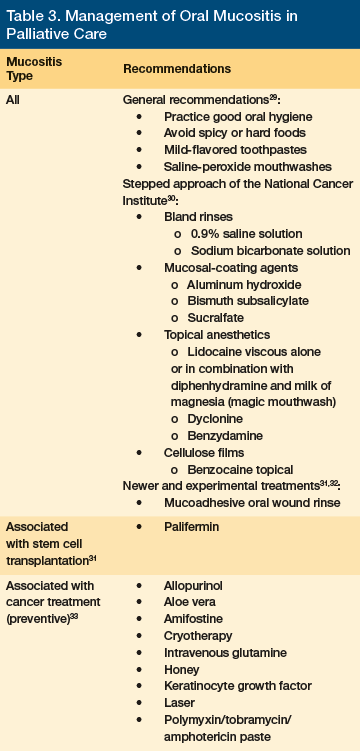
It has been suggested that Staphylococcus aureus may be responsible for a type of oral mucositis among elderly patients who are dehydrated and receiving intravenous fluids and parenteral nutrition.8 Clinical assessment reveals areas of erythema and atrophy on the mobile mucosa that extend into ulcers covered by a yellow or white fibrin layer. The sensitivity may keep patients from fully opening their mouths, which is uncomfortable and can interfere with eating and mouth care.6 Treatment methods for mucositis are aimed primarily at relieving pain (Table 3).28-32 Before initiating any of the therapeutic measures, however, it is important to identify and modify local traumatic factors, such as broken restorations or teeth or an impinging removable denture. Patients should be advised to avoid eating spicy foods and using tobacco and alcohol.22
Candidiasis
Candidiasis is infection with a fungus of the genus Candida that usually occurs in the skin and mucous membranes of the mouth, respiratory tract, or vagina; it may also invade the bloodstream, especially in immunocompromised individuals. Candidiasis is also referred to as candidosis, moniliasis, or thrush.33 Approximately 40% of healthy adults harbor yeasts in their mouth as commensals with no evidence of mucosal disease.34 If the burden of Candida becomes too great, such as for some palliative care patients who may be immunocompromised, candidiasis may then develop. The prevalence of candidiasis in palliative care patients has been estimated to be 34% to 70%.9,11-13
Candida albicans is one of many Candida species found in the oral cavity and it is responsible for most oral candidiasis. A minority of infections are caused by one or more of at least 12 other species, including C. glabrata, C. tropicalis, C. parapsilosis, and C. krusei.35 Several of the predisposing factors for fungal infections are consistent with conditions commonly observed in palliative care patients, such as mouth dryness, poor oral hygiene, use of dentures, use of broad-spectrum antibiotics, poor nutrition, and frailty, which includes being immunocompromised.36
Oral candidiasis may manifest itself clinically in different
ways according to its severity and location. Every effort should be made to confirm the diagnosis prior to treatment initiation. Palliative care patients often have heavy white coatings of the tongue and/or other tissues that can mimic pseudomembranous candidiasis.37 In the authors’ experience, a simple swab culture (available at microbiology laboratories for an estimated cost of $60) can help to determine its etiology; this can avoid improperly placing patients on antifungal medications. Rapid commercial systems (Microstix-Candida, Oricult-N) may also be helpful if access to a laboratory is not conveniently available.38
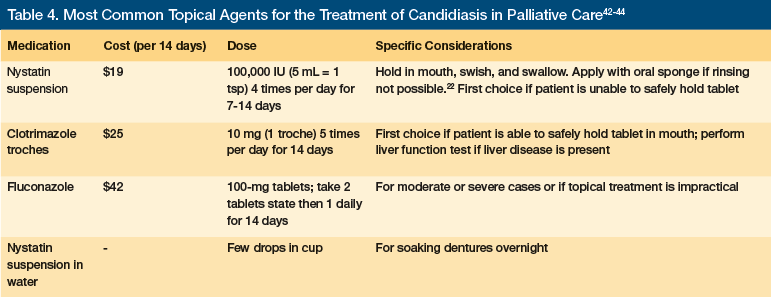
Candidiasis may be treated according to severity by one or more of the topical agents listed in Table 4.39–41 Dentures must be removed during medication application to oral tissues, and topical agents may be used on the dentures themselves. Sponge swabs can be used to apply the medications for palliative care patients who may be unable to rinse liquid suspensions.22 Systemic agents including ketoconazole, fluconazole, itraconazole, and/or amphotericin B may be required for especially severe or intractable candidiasis. For a detailed description of use of these agents, a guideline on the management of candidiasis should be consulted.39
Dysphagia
Dysphagia is defined as difficulty swallowing. It may be an acute or chronic condition that affects oral intake, and it is usually indicative of some disease process.40 Because this condition is common with a patient’s deconditioning near the end of life, many healthcare providers consider it relatively trivial and it is therefore unreported or underestimated. It is also frequently overlooked due to the presence of more prominent symptoms, such as pain or shortness of breath.41
Difficulty swallowing liquids can indicate poor muscular control; difficulty swallowing solids may indicate a physiologic abnormality such as a tumor. Gradual onset may indicate a neoplastic or neuromuscular etiology. Sudden onset may be indicative of a psychogenic etiology.42,43 Dysphagia has been detected in approximately 30% of patients with stroke, in 40% to 60% of patients with neurodegenerative disease, and in approximately 20% of patients with cancer, all of which may be treated with palliative care.44 It can cause or exacerbate other problems, such as weight loss, debility, and aspiration pneumonia, and in some cases it even hasten death.44
Other routes of food administration (intravenous nutrition or gastrostomy feeding tubes) may be used in patients who are unable to eat. However, there is increased evidence showing that feeding tubes for patients with dementia neither improve the quality of their lives nor prolong them.45
Difficulty Talking
Specific causes of this impairment have been identified in some cases, but it appears most commonly to be the result of the general disease progression that would affect intellectual capacity, memory, mood, concentration, and state of alertness. A study of 336 hospice patients, however, found that 27% had a physical impediment affecting communication.46
An evaluation by a dentist may be helpful for assessing the presence of low saliva flow or a defective dental prosthesis, which could interfere with talking. A speech therapist may be consulted if transient ischemic attacks, a stroke, or other neurologic damage is present, or if there has been injury to the throat or vocal apparatus. Further, other forms of communication such as signing and enlisting the assistance of the family members close to the patient can be valuable when verbalizing becomes difficult for the patient.
Denture Problems
The use of dentures is common in the current population of patients undergoing long-term care and palliative care. Numerous studies involving long-term care facility residents show that, while many individuals have dentures, only a limited proportion of these dentures are comfortable and functional.22,47 The proportion is likely higher among palliative care patients because of comorbidities including mouth dryness, candidiasis, and general physiologic losses.
Atrophy of facial muscles in advanced cancer patients contributes to the lack of support for dentures.9 Various treatments being administered for palliative care patients can induce nausea or various forms of sore mouth, conditions that reduce the comfortable use of dentures. Feeling as though the dentures are loose is common if significant weight loss has occurred. Denture problems that may appear frequently in palliative care patients include poor denture hygiene, loose dentures, nausea, and dentures with grossly poor fit.
Poor denture hygiene. Palliative care caregivers, who often have little or no training in oral healthcare, should be alerted to the presence of any dentures and should receive instructions for basic daily care. They can help to ensure that a denture brush, storage cup, and possibly effervescent cleaner are available.
Loose dentures. Relining the denture with a functional liner or tissue conditioner may be possible in a home or hospital room. This is one of a limited number of services that dentists can perform away from their offices that may yield significant benefits to function and quality of life for palliative care patients. Patients can also be encouraged to try any or all types of denture adhesives, including pastes, powders, and seaweed-based absorbent flexible plates.
Nausea. Nausea is common in this population, and trimming the distal extension of the upper denture away from the vibrating line at the junction of hard and soft palate for a patient experiencing nausea can help to better control this symptom.21
Dentures with grossly poor fit. Consider replacing the patient’s dentures using a denture copying technique to duplicate the shape, size, and interarch relationships of the old dentures but improving the fit and the retention. This method allows the dentist to restore basic function and aesthetics within a short period of time, with the goal of contributing to a palliative care patient’s function, dignity, and self-respect.3
Poor Oral Hygiene
An additional significant problem among palliative care patients is poor oral hygiene.3,22,47 This is likely due to a number of factors, including the patient’s cognitive and physical disabilities, the lack of optimal preventive devices and supplies, and the caregiver’s inadequate knowledge, attitudes, and experience regarding provision of oral care to people other than themselves.48,49 Finding particles of food, established plaque, and dried mucous saliva on the palliative care patient’s teeth, palatal and buccal mucosa, tongue, and dentures is common.
Preventive care protocols should be established early and maintained throughout the palliative care process as integral components of the patient’s treatment plan. This is important, as some palliative care patients recover to realize improved functional status (eg, patients assigned to hospice care, which typically occurs when life expectancy is reduced to 6 months, can unexpectedly realize remission and live longer).50,51 A number of preventive protocols that are appropriate for these patients are presented in Table 5.3,22,49

Conclusion
The number of patients undergoing palliative care is growing, and additional studies to help better define appropriate oral care are needed.52,53 It is likely that general dentists and those with training and experience with special care will increasingly be called upon to help ensure optimal oral health for this population. Attention to the issues included in this review and others may provide a helpful background for understanding the palliative care patient’s oral health needs and their management. The palliative care that dentists provide can play an important role, along with that of other healthcare providers, in managing patients with advanced illness; they must assess all of the oral problems that may lead to oral dysfunction, unnecessary pain, discomfort and other issues that compromise a patient’s quality of life.
1. World Health Organization. WHO Definition of Palliative Care. WHO website. http://www.who.int/cancer/palliative/definition/en/. Accessed August 19, 2015.
2. NHPCO Facts and Figures: Hospice Care in America 2014 Edition; page 4. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2014_Facts_Figures.pdf. Accessed July 20, 2015.
3. Wiseman MA. Palliative care dentistry. Gerodontology. 2000;17(1):49-51.
4. Parikh RB, Kirch RA, Smith TJ, Temel JS. Early Specialty Palliative Care - Translating Data in Oncology into Practice. N Engl J Med. 2013;369:2347-2351. www.nejm.org/doi/full/10.1056/NEJMsb1305469. Accessed July 19, 2015.
5. Fontaine A, Larue F, Lassaunière JM. Physicians’ recognition of the symptoms experienced by HIV patients: how reliable? J Pain Symptom Manage. 1999;18(4):263-270.
6. Walls AW, Murray ID. Dental care of patients in a hospice. Palliat Med. 1993;7(4):313-321.
7. Carr CH, McNeal H, Regalado E, Nelesen RA, Lloyd LS. PAL-MED CONNECT: a telephone consultation hotline for palliative medicine questions. J Palliat Med. 2013;16(3):263-267.
8. Walsh LJ. Clinical assessment and management of the oral environment in the oncology patient. Aust Dent J. 2010;55(Suppl 1):66-77.
9. Jobbins J, Bagg J, Finlay IG, Addy M, Newcombe RG. Oral and dental disease in terminally ill cancer patients. BMJ. 1992;304(6842):1612. www.ncbi.nlm.nih.gov/pmc/articles/PMC1881994/. Accessed July 19, 2015.
10. Aldred MJ, Addy M, Bagg J, Finlay I. Oral health in the terminally ill: a cross-sectional pilot survey. Spec Care Dentist. 1991;11(2):59-62.
11. Oneschuk D, Hanson J, Bruera E. A survey of mouth pain and dryness in patients with advanced cancer. Support Care Cancer. 2000;8(5):372-376.
12. Wilberg P, Hjermstad MJ, Ottesen S, Herlofson BB. Oral health is an important issue in end-of-life cancer care. Support Care Cancer. 2012;20(12):3115-3122.
13. Fischer DJ, Epstein JB, Yao Y, Wilkie DJ. Oral health conditions affect functional and social activities of terminally ill cancer patients. Support Care Cancer. 2014;22(3):803-810.
14. Sreebny LM. Xerostomia: diagnosis, management and clinical complications. In Edgar WM, O’Mullane DM (ed.) Saliva and Oral Health, 2nd edn. pp. 43-46. London: British Dental Association; 1996.
15. Billings RJ, Proskin HM, Moss ME. Xerostomia and associated factors in a community-dwelling adult population. Community Dent Oral Epidemiol. 1996;24(5):312-316.
16. Nederfors T, Isaksson R, Mörnstad H, Dahlöf C. Prevalence of perceived symptoms of dry mouth in an adult Swedish population--relation to age, sex and pharmacotherapy. Community Dent Oral Epidemiol. 1997;25(3):211-216.
17. Senn H. Orphan topics in supportive care: how about xerostomia? Support Care Cancer. 1997;5(4):261-262.
18. Cooke C, Ahmedzai S, Mayberry J. Xerostomia--a review. Palliat Med. 1996;10(4):284-292.
19. Plemons JM, Al-Hashimi I, Marek CL, American Dental Association Council on Scientific Affairs. Managing xerostomia and salivary gland hypofunction: executive summary of a report from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2014;145(8):867-873.
20. Dawes C. Physiological factors affecting salivary flow rate, oral sugar clearance, and the sensation of dry mouth in man. J Dent Res.1987;66 Spec No:648-653.
21. Sweeney MP, Bagg J. The mouth and palliative care. Am J Hosp Palliat Care. 2000;17(2):118-124.
22. Ettinger RL. The role of the dentist in geriatric palliative care. J Am Geriatr Soc. 2012;60(2):367-368.
23. Dry Mouth. National Institute for Dental and Craniofacial Research Website. www.nidcr.nih.gov/oralhealth/Topics/DryMouth/DryMouth.htm. Published August 2014; accessed July 19, 2015.
24. Vivino FB, Al-Hashimi I, Khan Z, et al. Pilocarpine tablets for the treatment of dry mouth and dry eye symptoms in patients with Sjögren syndrome: a randomized, placebo-controlled, fixed-dose, multicenter trial. P92-01 Study Group. Arch Intern Med. 1999;159(2):174-181.
25. Petrone D, Condemi JJ, Fife R, Gluck O, Cohen S, Dalgin P. A double-blind, randomized, placebo-controlled study of cevimeline in Sjögren’s syndrome patients with xerostomia and keratoconjunctivitis sicca. Arthritis Rheum. 2002;46(3):748-754.
26. Visch LL, Gravenmade EJ, Schaub RM, Van Putten WL, Vissink A. A double-blind crossover trial of CMC- and mucin-containing saliva substitutes. Int J Oral Maxillofac Surg. 1986;15(4):395-400.
27. Epstein JB, Emerton S, Le ND, Stevenson-Moore P. A double-blind crossover trial of Oral Balance gel and Biotene toothpaste versus placebo in patients with xerostomia following radiation therapy. Oral Oncol.1999;35(2):132-137.
28. Keefe DM, Schubert MM, Elting LS, et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007;109(5):820-831.
29. National Cancer Institute. Oral complications of chemotherapy and head/neck radiation – for health professionals (PDQ®). www.cancer.gov/about-cancer/treatment/side-effects/mouth-throat/oral-complications-hp-pdq#link/_746_toc. Accessed August 20, 2014.
30. MuGard Clinical Data. www.mugard.com/wp-content/uploads/2013/12/MuGard_Nurse_brochure.pdf. Accessed August 20, 2014.
31. Hadjieva T, Cavallin-Stahl E, Linden M, Tiberg F. Treatment of oral mucositis pain following radiation therapy for head-and-neck cancer using a bioadhesive barrier-forming lipid solution. Support Cancer Care. 2014;22(6):1557-1562.
32. Worthington HV, Clarkson JE, Bryan G, et al. Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2010;(12):CD000978. doi:10.1002/14651858.CD000978.pub3.
33. Arendorf TM, Walker DM. Oral candidal populations in health and disease. Br Dent J. 1979;147(10):267-272.
34. Scully C. Mucosal Candidiasis Workup. Medscape Website. http://emedicine.medscape.com/article/1075227-workup. Updated February 21, 2014; accessed July 20, 2014.
35. Samaranayake LP, Lamey PJ. Oral candidosis: 1. Clinicopathological aspects. Dent Update. 1988;15(6):227-228, 230-231.
36. Alt-Epping B, Nejad RK, Jung K, Gross U, Nauck F. Symptoms of the oral cavity and their association with local microbiological and clinical findings-- a prospective survey in palliative care. Support Care Cancer. 2012;20(3):531-537.
37. Shay K, Truhlar MR, Renner RP. Oropharyngeal candidosis in the older patient. J Am Geriatr Soc. 1997;45(7):863-870.
38. Scully C, el-Kabir M, Samaranayake LP. Candida and oral candidosis: a review. Crit Rev Oral Biol Med. 1994;5(2):125-157.
39. Pappas PG, Kauffman CA, Andes D, et al. Clinical Practice Guidelines for the Management of Candidiasis: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009:48:503–535.
40. Dahlin C, Cohen A. Dysphagia, xerostomia and hiccups. In: Ferrell BR, Coyle N, Paice J, eds. Oxford Textbook of Palliative Nursing: 4th Edition. New York, NY: Oxford University Press; 2015:191-216.
41. Miller RM. Clinical Examination for Dysphagia. In: Groher ME. Dysphagia: Diagnosis and Management, 3rd Edition. Newton, MA: Butterworth-Heinemann; 1997:169-189.
42. Bass NH. The neurology of swallowing. In: Groher M. Dysphagia: Diagnosis and Management. 3rd Edition. Newton, MA: Butterworth-Heinemann; 1997:7-35.
43. Schechter GL. Systemic causes of dysphagia in adults. Otolaryngol Clin North Am. 1998;31(3):525-535.
44. Sykes NP, Baines M, Carter RL. Clinical and pathological study of dysphagia conservatively managed in patients with advanced malignant disease. Lancet. 1988;2(8613):726-728.
45. Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: a review of the evidence. JAMA.1999;282(14):1365-1370.
46. Jackson P, Robbins M and Frankel S. Communication impediments in a group of hospice patients. J Palliat Med. 1996;10:79-80.
47. Wiseman M. The treatment of oral problems in the palliative patient. J Can Dent Assoc. 2006;72(5):453-458.
48. Bellior MN, Riou F. [Nursing staff’s knowledge and attitudes concerning preventive oral hygiene in palliative care]. Article in French. Rech Soins Infirm. 2014;(117):75-84.
49. Chalmers J, Johnson V, Tang JH, Titler MG. Evidence-based protocol: oral hygiene for functionally dependent and cognitively impaired older adults. J Gerontol Nurs. 2004;30(11):5-12.
50. Hospice website. www.hospice.net. Accessed September 6, 2014.
51. Dotinga R. Close-Up: When Hospice Patients Live Too Long. MedPageToday. January 18, 2013. www.medpagetoday.com/PublicHealthPolicy/GeneralProfessionalIssues/36898. Accessed September 6, 2014.
52. Chen X, Chen H, Douglas C, Preisser JS, Shuman SK. Dental treatment intensity in frail older adults in the last year of life. J Am Dent Assoc. 2013;144(11):1234-1242.
53. Chen X, Clark JJ, Naorungroj S. Oral health in nursing home residents with different cognitive statuses. Gerodontology. 2013;30(1):49-60.










