Life at the Extreme: Characteristics of Veteran Centenarians in Long-term Care
Abstract
Centenarians have become an important part of the rapidly increasing oldest population. However, a paucity of knowledge exists about US veteran centenarians residing in the long-term care setting. To address this knowledge gap, an extensive review of the electronic health records was performed for all information on centenarians who resided in the Washington DC Veterans Health Medical Center between 2005 and 2015, in order to describe their basic demographic, mental, medical, and functional characteristics. A total of 8 centenarians, whose age at death ranged from 101 to 108 years, were identified as having resided at the facility during that period. While most of the veteran centenarians exhibited multiple clinical markers for frailty, they were generally socially engaged, with a low occurrence rate of anxiety and depression. The plan of care for individuals in the study was found to be person-centered and encouraged choice, purpose, and meaning. Treatment was targeted to lessen burden of disease and improve quality of life through social engagement and psychological support. Although death was not an unexpected outcome, the patients and their caregivers maintained realistic hope and were quite involved in their care plans.
Introduction
The remarkable improvement in longevity during the 20th century is considered to be one of humanity’s greatest achievements. While in the early 19th century only a small proportion of people lived to old age, in modern societies most people live well past middle age, and deaths are highly concentrated at older ages. Recent research shows a continuing increase in life expectancy among persons aged 80 and older worldwide.1,2
Although centenarians currently account for a small percentage of the population, the World Health Organization projects the global number of centenarians to increase 10-fold between 2010 and 2050.3 The US Census Bureau estimates that the number of centenarians in the United States will exceed 850,000 by 2050.4
Significant improvements in public health, prevention, and treatment of disease, as well as technologic advances such as the introduction of antibiotics in the early 20th century, have contributed to significant increases in health span and in life expectancy.5,6 Studies of the US centenarian population that have been initiated over the past few decades include the Georgia Centenarian Study; the New England Centenarian Study, which continues to recruit and enroll US and Canadian centenarians and their siblings; and the Longevity Genes Project at Albert Einstein College of Medicine in New York.7-9
The Veterans Health Administration, with its longstanding adoption of the electronic health record (EHR) system, provides an opportunity to add to the current knowledge about US veteran centenarians. To date, no study has described veteran centenarians residing in institutional long-term care (LTC) settings. Therefore, presented below is a case series of 8 veteran centenarians who between 2005 and 2015 resided at the Washington DC VA Medical Center, a 120-bed, 24-hour, hospital-based skilled nursing care facility that includes long-term, restorative and short-term rehabilitative services in addition to inpatient palliative and hospice services. The objective of the study was to describe the basic demographic, mental, medical, and functional characteristics in order to fill a knowledge gap about this population group.
Participants and Procedure
All patients were admitted and their cases followed by an interdisciplinary team comprising a full-time geriatrician, a nurse practitioner, a registered nurse, a social worker, a nutritionist, a pharmacist, a psychologist, speech therapists, recreation therapists, physical therapists/occupational therapists, and a chaplain. All consultative services were provided by specialists who visited veterans in their long-term settings and discussed treatment plans with the core team as appropriate. Advance care planning (ACP) was conducted at admission, when a significant change in a patient’s medical condition occurred, and when the patient or patient’s surrogate requested it.
Demographics and Care Model
Demographics of the participants are presented in Table 1. All participants were veterans of WWII (1939-1945). They were predominantly men, unlike the gender distribution outside the VA health care system, where centenarians living in nursing homes are 90.3% women.4 Furthermore, whereas centenarians in US community nursing homes are 82.5% white,4 these participants were predominantly African American, reflecting the local population. Six participants had served overseas in the European or Pacific theater. The men had served in combat, and the women in supportive services.
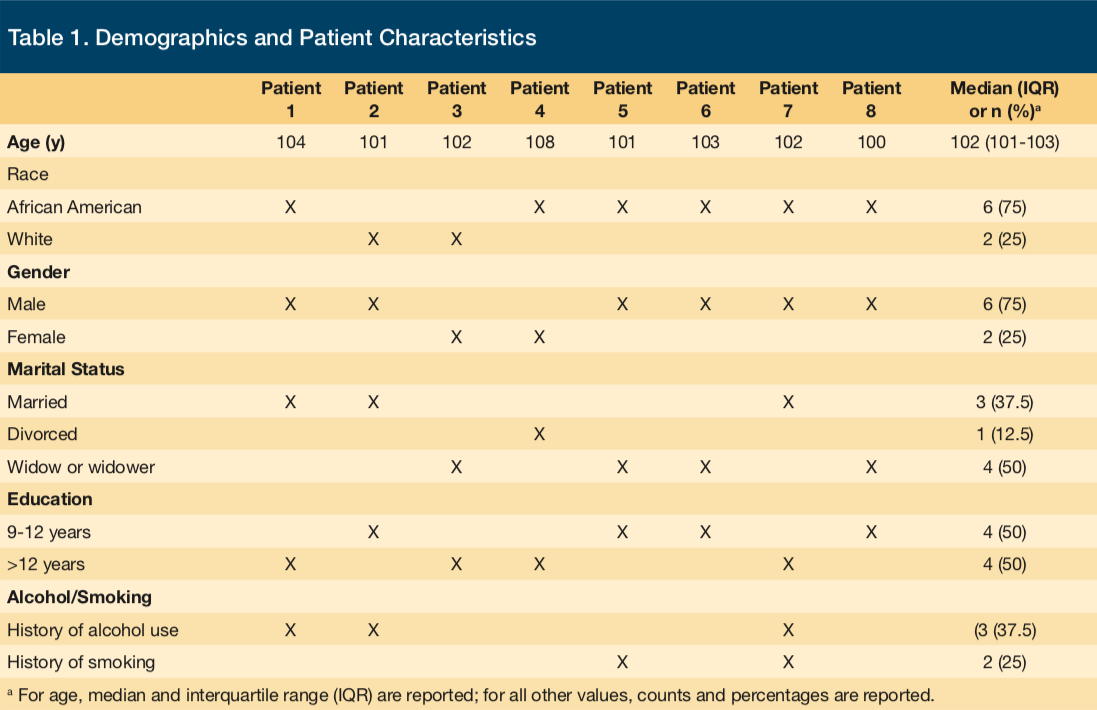
Their years of education varied widely (9 years to postgraduate), however, these centenarians did have a number of characteristics in common. They had adopted a healthy lifestyle; they were nearly always lean, and a substantial smoking and alcohol history was rare. Further studies are needed to evaluate the impact of the state of mental health on longevity in this population.
The most notable observation made during review was that goals of care were discussed and articulated during ACP discussions with the patients and/or their surrogates. The patients shared the goals of reducing disease burden and improving quality of life and survival. These goals were accomplished through conservative and closely monitored medical care provided by an involved interdisciplinary team. The team-based model is most helpful because the caregiver burden is significant. This is invaluable in the management of those patients and often involves disciplines such as nursing, dietary, physical and occupational therapy, social work, and palliative care. Four main strategies were utilized in optimally managing these medically complex patients in the LTC setting: person-centered shared decision-making, close clinical supervision, medication management, and specialist comanagement.
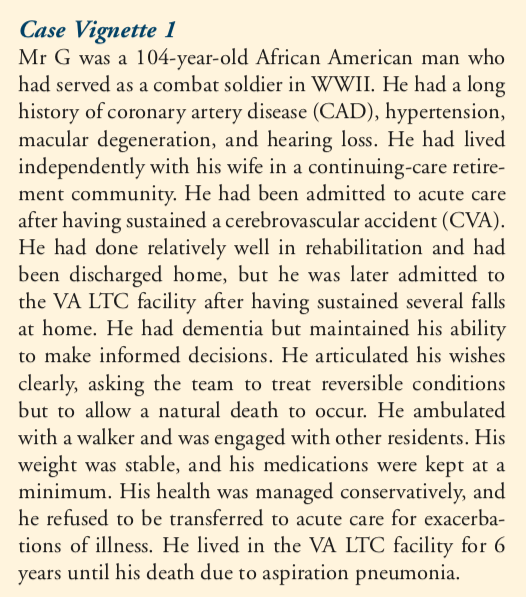
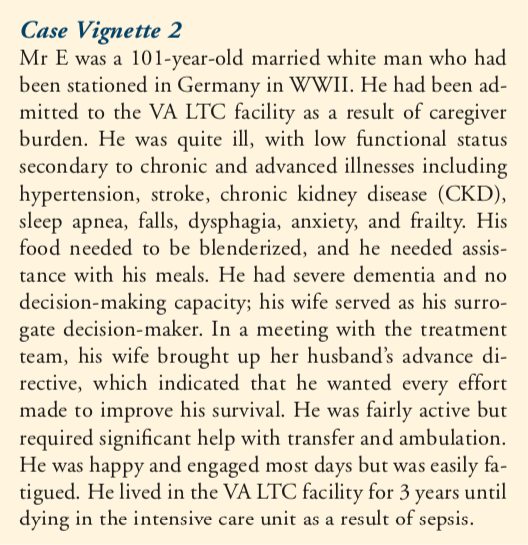
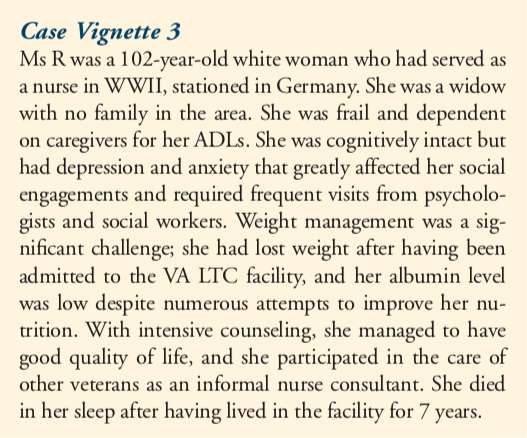
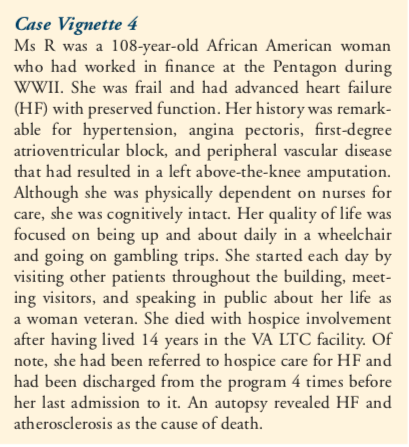
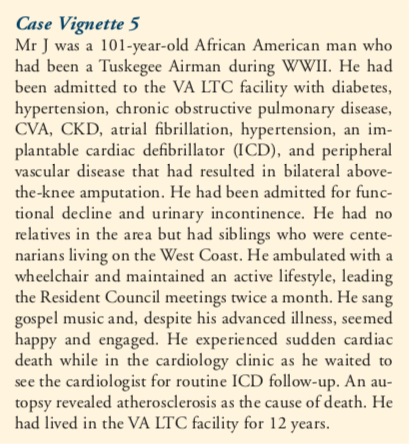
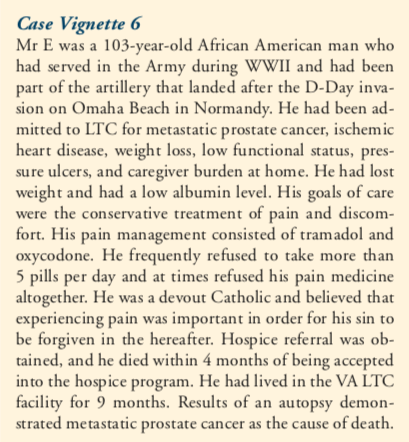
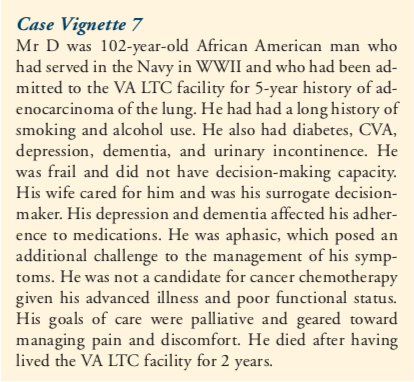
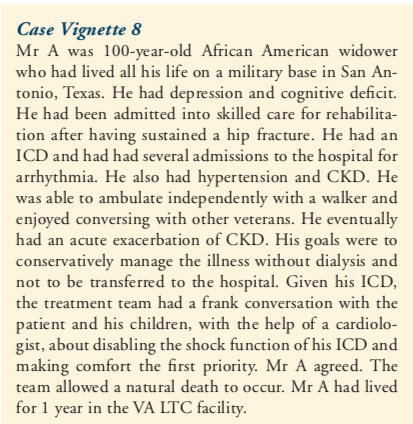
Individual patient information can be found in Case Vignettes 1-8, which include both medical and social history with some included anecdotal observations based on EHR notes from the interdisciplinary team.
Discussion
This case series of 8 veteran centenarians in LTC shows that, despite their advanced chronic illness and multiple clinical markers of frailty, they were socially engaged with low levels of anxiety, depression, and delirium. An examination of mental, medical, and functional characteristics and commonalities among this cohort of centenarians in a LTC setting are presented in the different sections below.
Mental Health and Psychosocial Wellbeing
At age 100, depression screens were negative in 5 participants. In reviewing neuropsychological assessments, 6 centenarians had mild to moderate dementia that had been diagnosed after age 80. Of the 6 patients with a diagnosis of dementia, 3 were deemed to have the capacity to make informed decisions.
The progress notes of the nursing staff, as well as the results of recreation and art therapy, revealed that the veteran centenarians in this cohort were socially engaged and participated in offered discussion groups, arts, and music programs. Five of the 8 centenarians were regular participants in an intergenerational program with an area university. Four attended day trips and local excursions that were offered weekly. One veteran was president of the Resident Council in the facility. They all attended chapel regularly and exhibited a robust personality and a desire to lead an autonomous life. When asked, 6 veterans self-rated their health as excellent; self-rated health correlates significantly with functioning and mortality in the oldest old.10,11 However, nurses documented that patients were noted to fatigue easily and to sleep long uninterrupted hours. Most started their day after 11 am. They were noted to be totally engaged while awake. Studies have demonstrated that centenarians generally have low levels of neuroticism but high levels of extraversion, conscientiousness, and agreeableness.12-15 On average, centenarians are responsible, easygoing, capable, relaxed, efficient, and not prone to anxiety.14,16 Specifically, openness to experience related positively with higher scores in mental well-being, but neuroticism and conscientiousness are negatively related to mental health.17
Article continues on page 2
All centenarians had ACP documents. The ACP discussion occurred, according to policy, once a year and whenever there was a change in the patient’s medical condition. It was conducted with the patients and/or their surrogates. Six patients reported consistent wishes to allow natural death to occur. All centenarians exhibited a desire for autonomous living to reduce illness burden and improve quality of life. Four of the 8 centenarians had living relatives in the area who visited. The parents of 3 of the centenarians had lived beyond age 75. One centenarian had a twin sister who was community-dwelling and independent in her ADLs at age 102.
Comorbidities
Patients’ morbidity profile was reviewed (Table 2), with the most common medical conditions being musculoskeletal (87.5%), CAD (87.5%), hypertension (75%), dementia (75%), hearing loss (62.5%), cataract (50%), glaucoma (37.5%), macular degeneration (25%), urinary incontinence (75%), stroke (50%), kidney injury (50%), diabetes (25%), depression (25%), delirium (25%), and anxiety (25%). Corresponding with previous research18 that more than 80% of centenarians either delay or avoid entirely diseases that normally are associated with significant mortality, 5 of the centenarians in the present study did not have chronic illness before age 80.
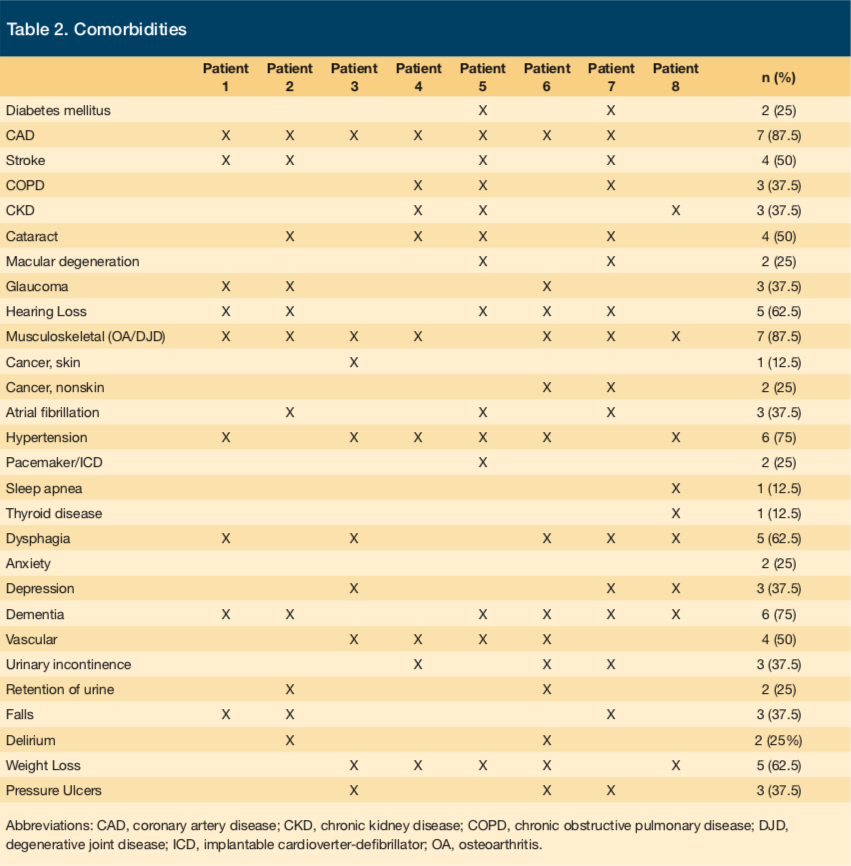
Four of the centenarians had war-related disabilities: 2 had hearing loss secondary to working in army field artillery, 1 had skin cancer secondary to sun exposure while in naval service on surface ships, and 1 had a musculoskeletal injury secondary to infantry work during basic training camp. The remaining 6 centenarians had musculoskeletal disorders that were not related to an injury acquired during service. Not surprisingly, more than 50% of the cohort had 12 or more years of education. The average highest grade attained was eighth grade during that period in the United States.19 Not until 1915 did states begin advocating for at least 12 years of education.20 Given that longevity has been associated with years of education,21 the change in years of required education, in combination with improved public health and medical interventions, will likely contribute to the increasingly higher prevalence of centenarians.22 Interestingly, the 2 women centenarians in this cohort had more than 12 years of education (1 was a nurse, and 1 had master’s degree in finance).
Six centenarians had never smoked, and 2 had smoked but had quit in their 70s. Three centenarians had history of alcohol use in their 50s. The adoption of a healthy lifestyle and the low rate of smoking and alcohol use in our study group is similar to that of the majority of community-dwelling centenarians and likely plays an important role in their longevity.23
The patients’ median systolic blood pressure was 127 mm Hg (interquartile range [IQR], 120-137 mm Hg), the median diastolic blood pressure was 66 m Hg (IQR, 60-78 mm Hg), and the median pulse rate was 76 beats/min (IQR, 73-79 beats/min), all of which were within normal ranges (Table 3).
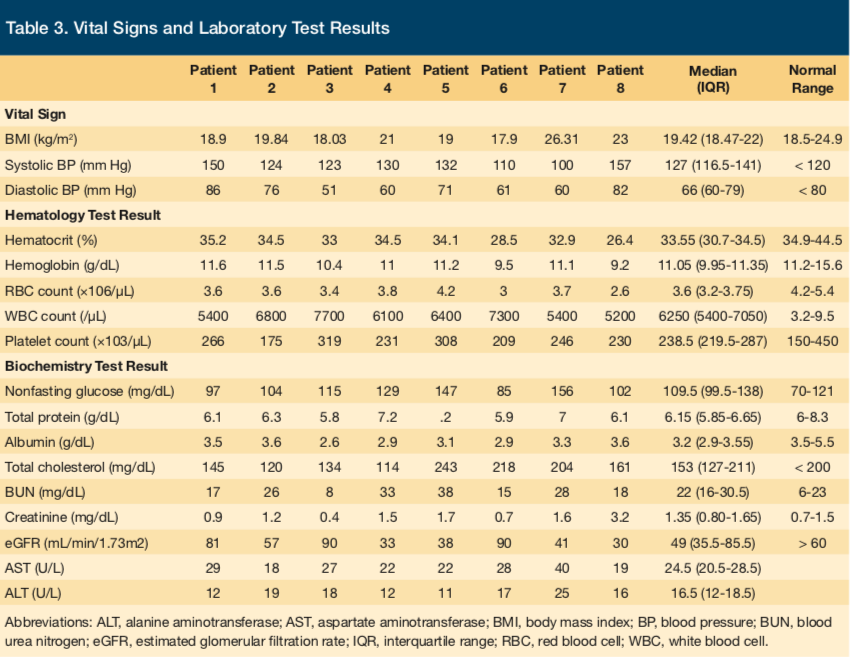
The results of complete blood cell counts were significant for anemia, with a median hematocrit level of 33.55% (IQR, 32%-35%). The results of basic metabolic panels were significant for elevated urea nitrogen levels, with a median of 22 mg/dL (IQR, 17-29 mg/dL), and reduced estimated glomerular filtration rates, with a median of 64.5 mL/min/1.73m2 (IQR, 40-83 mL/min/1.73m2). Liver function tests revealed borderline low albumin levels, with a median of 3.2 g/dL (IQR, 3-4 g/dL). Reference ranges can be found in Table 3.
Function and Frailty
All of the patients had had decreased physical function beginning at age 100 and had received assistance that ranged from help with walking to assistance in all ADLs. All patients had reduced grip strength, and the 3 patients who were able to walk unassisted by personnel took 3 to 5 minutes to walk 15 feet. Three patients had had documented falls. No fractures or adverse events related to the falls were noted. All participants needed assistive devices to ambulate ranging from canes to wheelchairs.
While the study group demonstrated clinical markers for frailty that appeared to have contributed to admission into LTC, reviewing their EHRs revealed that they had independent functional status into their early 90s. Several reports found the centenarians to have exhibited marked delays in functional decline and, in most cases, age-related lethal diseases such as heart disease, cancer, and stroke. Compression of functional decline toward the relative end of their lives might be a prerequisite for or at least a marker of the ability to live to 100.18 In a sample of 37 centenarians, 88% were functionally independent at a mean age of 92.23 It has been reported that the time in which centenarians experience frailty is compressed toward the end of their lives, in part because frailty in old age is likely a potent predictor of mortality.23 Such a compression is even more pronounced in male centenarians. Male centenarians tend to be healthier and more functional with fewer comorbid medical conditions.24 It is critical for patients in LTC facilities to be provided with a continuum of rehabilitation services that are patient-centered, ranging from subacute to restorative care, in order to prevent further functional decline and to promote their safety.
Weight and Nutrition
The centenarians in the study had low to normal body mass index (BMI) on admission and at age 100 (Table 3). The median BMI was 19.42 kg/m2 (IQR, 18.47-22 kg/m2). Reviewing nutrition progress notes revealed that all of the patients had partial or full dentures and received varying degrees of assistance during meals. The residents’ weight was being monitored monthly; all had a liberal diet, ie, frequent offerings of snacks between meals, and received most of their nourishment from foods with modified consistency (eg, emulsified or mechanically altered) based on individual food tolerance. While 5 patients stabilized and had an acceptable intake, only 1 gained weight, and 3 had moderate weight loss after being admitted to LTC despite several conservative interventions by staff.
The evidence from the literature demonstrates an inverse relationship between body weight and longevity;25 however, living situations may contribute significantly to food patterns, and residing in LTC may have helped the veterans’ nutrition. Community-dwelling centenarians may not have access to wholesome foods. Contributory factors include physical or mental health conditions that lead to difficulty with biting, chewing, and swallowing; an impaired ability to shop or cook; and a lack of knowledge about the food and nutritional needs of older adults.26
Medication Management
The medication profiles starting from age 100 until time of death were reviewed for safety and appropriateness with respect to drug duplications, indications, omissions, interactions, and Beers criteria for potentially inappropriate medication use in older adults.
The clinical review revealed that patients were taking very few long-term medications and had minimal medication errors. Given the extensiveness of the Beers criteria, it is impressive that only half of patients were taking 1 or 2 medications included on that list. It is also interesting that none had been prescribed nonsteroidal anti-inflammatory drugs (NSAIDs). Several patients had musculoskeletal disorder including osteoarthritis and degenerative joint disease among their morbidities, but their condition was managed mainly with diclofenac gel and acetaminophen. NSAID use is riskier in older adults given declining kidney function, an increased risk of bleeding, and an increased risk of cardiac problems. It was also surprising that only 1 of the 8 patients had been prescribed a statin medication, despite that half of them had compelling indications such as CAD, CVA, type 2 diabetes, and atrial fibrillation. This may be due to age, since many medications that are considered preventive are stopped when patients reach the age of 90 to 100, depending on their physical condition. This would not explain why many were continued on low-dose aspirin, however. The 1 patient who had been taking a statin had a history of cardiac bypass after a myocardial infarction. The patients on average were taking 5 chronic daily nonvitamin medications (range, 0-10). One duplication was identified: 2 different opiates (tramadol and oxycodone-acetaminophen) had been prescribed with no indication of when to give which medication (ie, tramadol for pain rated from 1 to 4 on a 10-point scale, and oxycodone-acetaminophen for pain rated from 5 to 10). There were a number of medications prescribed with no indication, and a number of treatment omissions. Half of the patients had at least 1 medication on the Beers list—3 had been taking a proton-pump inhibitor, 1 had had a ketorolac injection, and 1 with a documented diagnosis of psychosis was on quetiapine.
Advancing age leads to impairment in the function of several processes that provide functional integration between cells and organs. As a result, a failure to maintain homeostasis may occur under conditions of physiologic stress. Age-related physiologic alterations might also affect pharmacokinetics and pharmacodynamics and influence patients’ responses to medications. Minimizing high-risk medication use in the LTC setting is an important goal for health care providers. Having a pharmacist working with the treatment team to review and reconcile medication lists for appropriateness and effectiveness is crucial. It is also important to remember that treatment for this age group is not evidence-based but rather is extrapolated from data from younger groups.27
Conclusion
Although the evidence to support various treatments in centenarians is lacking, plans of care should always be person-centered and encourage choice, purpose, and meaning. Furthermore, treatment should be targeted to lessen burden of disease and improve quality of life but realistic hope should be maintained. Improved care outcomes are typically accomplished through shared decision-making between a knowledgeable, well-coordinated, interdisciplinary team and an informed patient and family. Improved knowledge of centenarians’ characteristics and health status in the LTC setting may inform and assist clinicians in enhancing the quality of care delivered to this population.
Affiliations, Disclosures, & Correspondence
Authors:
Raya Elfadel Kheirbek, MD, MPH1,2; Ali Fokar, MPH2; Leakie Wilson- Bell, RN2; Shannon DeGrote, PharmD, BCPS2
Affiliations:
1 George Washington University School of Medicine and Health Sciences, Washington, DC
2 Washington DC VA Medical Center, Washington, DC
Disclosures:
Dr Kheirbek received funds from the Veterans Affairs Capitol Health Care Network (VISN 5) to establish the Center for Health and Aging at the Washington DC VA Medical Center.
Address correspondence to:
Raya Elfadel Kheirbek, MD, MPH
50 Irving Street, NW Washington, DC, 20422
Phone: (301) 412-5529 Fax: (202) 745-8605
Email: rekheirbek@gwu.edu
References
1. Ismail K, Nussbaum L, Sebastiani P, et al. Compression of morbidity is observed across cohorts with exceptional longevity. J Am Geriatr Soc. 2016;64(8):1583-1591.
2. Sebastiani P, Sun FX, Andersen SL, et al. Families enriched for exceptional longevity also have increased health-span: findings from the Long Life Family Study. Front Public Health. 2013;1:38.
3. Global Health and Aging. World Health Organization; National Institute on Aging. October 2011. https://www.who.int/ageing/publications/global_health.pdf. Accessed
December 13, 2017.
4. Meyer J. Centenarians: 2010. Washington, DC: US Census Bureau; 2012. Publication C2010SR-03. https://www.census.gov/prod/cen2010/reports/c2010sr-03.pdf. Accessed December 13, 2017.
5. Fries JF. Measuring and monitoring success in compressing morbidity. Ann Intern Med. 2003;139(5 pt 2):455-459.
6. Willcox BJ, Willcox DC, Ferrucci L. Secrets of healthy aging and longevity from exceptional survivors around the globe: lessons from octogenarians to supercentenarians. J Gerontol A Biol Sci Med Sci. 2008;63(11):1181-1185.
7. Poon LW, Clayton GM, Martin P, et al. The Georgia centenarian study. Int J Aging Hum Dev. 1992;34(1):1-17.
8. Sebastiani P, Perls TT. The genetics of extreme longevity: lessons from the New England centenarian study. Front Genet. 2012;3:277.
9. Ismail K, Nussbaum L, Sebastiani P, et al. Compression of morbidity is observed across cohorts with exceptional longevity. J Am Geriatr Soc. 2016;64(8):1583-1591.
10. Liu G, Zhang Z. Sociodemographic differentials of the self-rated health of the oldest-old Chinese. Popul Res Policy Rev. 2004;23(2):117-133.
11. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21-37.
12. Jopp DS, Park M-KS, Lehrfeld J, Paggi ME. Physical, cognitive, social and mental health in near-centenarians and centenarians living in New York City: findings from the Fordham Centenarian Study. BMC Geriatr. 2016;16:1. doi:10.1186/s12877-015-0167-0
13. Poon LW, Jazwinski M, Green RC, et al; Georgia Centenarian Study. Methodological considerations in studying centenarians: lessons learned from the Georgia Centenarian Studies. Annu Rev Gerontol Geriatr. 2007;27(1):231-264.
14. Silver MH, Jilinskaia E, Perls TT. Cognitive functional status of age-confirmed centenarians in a population-based study. J Gerontol B Psychol Sci Soc Sci. 2001;56(3):P134-P140.
15. Jopp D, Rott C. Adaptation in very old age: exploring the role of resources, beliefs, and attitudes for centenarians’ happiness. Psychol Aging. 2006;21(2):266-280.
16. Martin P, Poon LW, Clayton GM, Lee HS, Fulks JS, Johnson MA. Personality, life events and coping in the oldest-old. Int J Aging Hum Dev. 1992;34(1):19-30.
17. Poon LW, Martin P, Bishop A, et al. Understanding centenarians’ psychosocial dynamics and their contributions to health and quality of life. Curr Gerontol Geriatr Res. 2010;2010: 680657. doi:10.1155/2010/680657
18. Evert J, Lawler E, Bogan H, Perls T. Morbidity profiles of centenarians: survivors, delayers, and escapers. J Gerontol A Biol Sci Med Sci. 2003;58(3):232-237.
19. Graham PA. Community and class in American education, 1865-1918. New York, NY: Wiley;1974.
20. Clifford GJ. 6: Education; its history and historiography. Rev Res Education. 1976;4(1):210-267.
21. Hummer RA, Hernandez EM. The effect of educational attainment on adult mortality in the United States. Popul Bull. 2013;68(1):1-16.
22. Diehr P, Derleth A, Cai L, Newman AB. The effect of different public health interventions on longevity, morbidity, and years of healthy life. 2007;7:52.
23. Hitt R, Young-Xu Y, Silver M, Perls T. Centenarians: the older you get, the healthier you have been. Lancet. 1999;354(9179):652.
24. Franceschi C, Motta L, Valensin S, et al. Do men and women follow different trajectories to reach extreme longevity? Italian Multicenter Study on Centenarians (IMUSCE). Aging (Milano). 2000;12(2):77-84.
25. Samaras TT, Storms LH, Elrick H. Longevity, mortality and body weight. Ageing Res Rev. 2002;1(4):673-691.
26. Kuczmarski MF, Weddle DO; American Dietetic Association. Position paper of the American Dietetic Association: nutrition across the spectrum of aging. J Am Diet Assoc. 2005;105(4):616-633.
27. Kropf NP, Cummings SM. Evidence-Based Treatment With Older Adults: Theory, Practice, and Research. New York, NY: Oxford UP;2017.










