Incorporating INTERACT II Clinical Decision Support Tools into Nursing Home Health Information Technology
Hospitalizations and rehospitalizations for ambulatory-sensitive conditions (ie, conditions that can often be managed in a nonacute setting) among nursing home (NH) residents are common and costly, and can result in numerous iatrogenic complications.1-4 Many of these hospitalizations are potentially avoidable.1-6 Interventions to Reduce Acute Care Transfers (INTERACT) is an example of a quality improvement intervention designed to facilitate the identification, evaluation, documentation, and communication about changes in resident status and support clinical decision-making. This is accomplished by collecting information about baseline care plan goals and condition-specific medical information when a change in status occurs. A set of clinical practice tools (ie, INTERACT II), including care paths and a variety of related educational materials, have been developed for dehydration, fever, mental status changes, congestive heart failure, lower respiratory infections, and urinary tract infections; these are six of the most common medical conditions that cause potentially avoidable hospitalizations. The INTERACT II care paths and other tools incorporate information from various sources, including best practices, clinical practice guidelines, and input from frontline NH providers and national experts in long-term care. An overview of the INTERACT intervention and downloadable tools are available at https://interact2.net.
Paper-based INTERACT II tools have been pilot tested in three NHs with high hospitalization rates in Georgia, and refined and evaluated in a quality improvement project completed by 25 NHs in Florida, New York, and Massachusetts. Implementation of the INTERACT quality improvement intervention was associated with a substantial reduction in hospitalization rates in both projects.5,6 Although use of the INTERACT II paper-based tools was successful, there is significant promise to further increase their potential impact. This can be accomplished by developing, implementing, and using INTERACT II tools through health information technology (HIT), such as standalone or integrated clinical decision support systems (CDS). This article highlights the process of translating INTERACT II tools from paper to NH HIT by addressing the following: (1) why these tools should be incorporated into HIT; (2) which currently available tools lend themselves to integration into HIT systems as CDS tools; (3) which design and implementation lessons from research and industry experience should be taken into account when integrating these CDS tools; and (4) how administration and providers can implement these CDS tools.
Why Incorporate INTERACT II CDS Tools into NH HIT?
Some of the reported challenges associated with using paper-based INTERACT II tools may be improved when these tools are incorporated into NH HIT. Use of an electronic format will enable staff to spend less time updating static data, provide greater access to automated information, reduce the time needed to track down information from disparate sources, minimize the time spent on performing manual calculations, and keep tasks on track through reminders or prompts
noting when specific actions should be taken.
Automating a core set of INTERACT II tools as a CDS system integrated into NH HIT will likely result in a higher likelihood of sustainable improvement in resident and/or clinician process or outcome measures, which may include:
• Improved communication among members of the multidisciplinary team, increasing the likelihood of identifying high-risk residents and improving clinical decision-making.
• Improved resident, staff, and physician satisfaction, resulting from enhanced communication.
• Decreased number of potentially avoidable emergency department evaluations and/or hospitalizations of NH residents with acute changes in condition or ambulatory-sensitive conditions.
• Reduced costs from a societal perspective if unplanned transfers can be avoided or better care is provided in the acute care setting because of enhanced communication.
INTERACT II Tools That Lend Themselves to NH HIT Integration
Based on previous experience and feedback from sites participating in INTERACT projects, five CDS tools should be considered for integration into NH HIT:
1. Stop and Watch: This tool can be used by certified nurse
assistants (CNAs) to note observed acute changes in resident condition and to document these changes. It also provides guidance on reporting these changes to a nurse or nurse practitioner for further evaluation and management.
2. Care Paths: These tools enable nursing staff to assess residents who have common conditions that may result in a potential transfer to a hospital and notify the appropriate primary care provider regarding a resident’s condition.
3. Situation, Background, Assessment, Recommendation (SBAR): This structured communication framework and progress note enables nursing staff to document and facilitate communication with primary care providers about their assessments based on the Care Paths and other tools.
4. Resident Transfer Form: This form is to be completed by nursing staff to ensure that a standardized set of resident-specific data accompany all transfers to the emergency department.
5. Quality Improvement Review: This tool is used to examine transfer situations and provide opportunities to discuss interventions that may have resulted in a different outcome.
Lessons Learned From Others’ CDS Design and Implementation
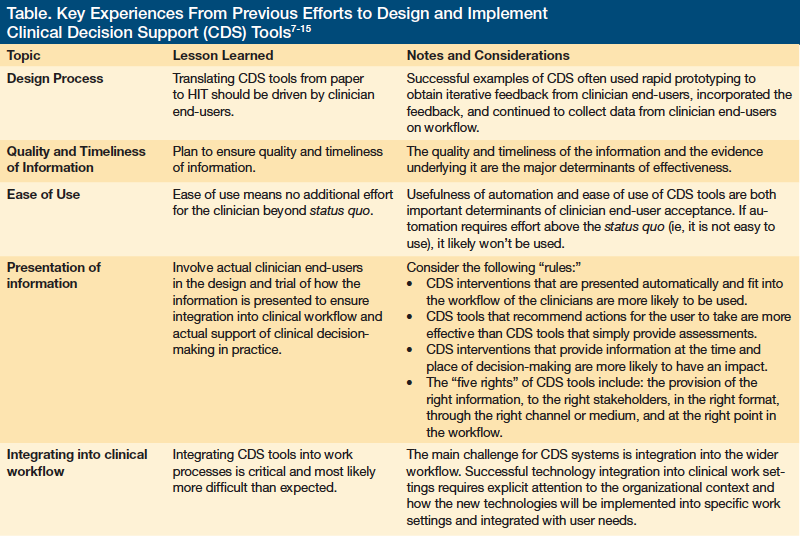
Several key experiences from previous efforts to design and implement CDS tools provide guidelines to automate existing paper tools, offering insights into the design process, quality and timeliness of information, ease of use, presentation of information, and integration into clinical workflow.7-15 Lessons from these experiences are outlined in detail in the Table. Before proceeding to integrate INTERACT II tools into NH HIT systems, these lessons should be carefully considered to ensure success.
Roadmap for Integrating INTERACT II Paper Tools Into NH HIT
Several major design steps are required when translating paper-based INTERACT II tools for use in HIT. These steps include establishing goals of the CDS design phase, assembling an integrated team, confirming data elements, translating clinical decision tools from paper to HIT, integrating CDS into the workflow, and pilot testing the tools before implementation.
Establishing CDS Design Phase Goals
The result of the design phase will be software requirements for HIT software developers. The software requirements specification document will describe the seamless integration of best practice guidelines into caregiver day-to-day workflow, communications, and documentation. It will also specify requirements of CDS. The goals of integrating INTERACT II CDS tools into NH HIT software include:
• Facilitating earlier identification of residents at risk for
hospitalization or rehospitalization.
• Ensuring timelier follow-up on recommended care path interventions for residents identified as being at risk for acute care transfer.
• Delivering workflow efficiencies by autogenerating forms and communication tools prefilled with previously recorded resident information, such as resident name, identification, diagnosis codes, allergies, vital signs, and medications.
• Supporting quality improvement efforts by providing summarized information in the form of reports to understand root cause patterns and trends.
Assembling an Integrated Team
The team responsible for the design process includes a facilitator, frontline staff, and software developer. The facilitator serves as a liaison between frontline staff and the software developer. He or she also works with clinicians to translate paper tools into software development requirements. Clinical staff members are key stakeholders who provide clinical expertise and working knowledge of clinical operations and workflow.
Confirming Data Elements
In this step, paper tools to be automated are analyzed at the data-element level to gain understanding of each element’s use and to compare each element against same or similar elements already available in the facility’s system. Redundancies and inconsistencies are highlighted during this process. The goal is to minimize additional documentation burden and to leverage existing documentation to the extent possible.
Translating CDS Tools From Paper to NH HIT
After the data elements from paper tools are defined and confirmed, the next step is to translate the CDS tools from paper to NH HIT for use in actual practice. This includes developing the content, formatting the information, and establishing the algorithms or rules that will produce the alert, reminder, or report.
Integrating CDS into Workflow
The final step in the design stage is to confirm how each CDS tool will be integrated into the daily workflow of the clinician end-user. Processes should be outlined to show who will be using CDS tools and describe how often they will be used. Use cases (defined as a description of steps or actions between a clinician and a software system that leads the user towards something useful) are helpful to describe the process to the system’s clinician end-users to ensure feasibility and integration into workflow.
Pilot Testing and Implementation
Once the design is completed, the requirements have been integrated into NH HIT, and an implementation plan has been established, it is helpful for the facility to conduct a pilot test on at least one nursing unit. This is done to confirm usability by clinicians in the real-world setting and identify changes to design or workflow that may be required before facility-wide implementation is undertaken. Establishing a full implementation rollout plan requires designating resources for training and information technology support, changing management plans to handle anticipated and unanticipated barriers to implementation, providing feedback mechanisms for ongoing refinement and management, and establishing a process to monitor impact.
Conclusion
The INTERACT quality improvement intervention and related paper-based tools have demonstrated the potential to enhance the detection, management, and communication of acute change in condition among NH residents, and to reduce the incidence of potentially avoidable hospitalizations.
Developing INTERACT II CDS tools in an interoperable format that would enable widespread dissemination and integration into various NH HIT products could lead to sustainable improvement in resident and clinician process and outcome measures, including a reduction in unplanned transfers and potentially avoidable hospital admissions. Possible next steps include the development of HIT specifications for INTERACT II CDS tools, embedding and testing the CDS into various NH HIT products, and formally evaluating the impact of the CDS on various resident and clinician process and outcome measures.
Work on this paper was supported in part by a grant from the Commonwealth Fund (to Dr. Ouslander), and grants from the Agency for Healthcare Research and Quality, R01HS018721 and the National Institute on Aging, K07AG033174 (to Dr. Handler).
Dr. Handler is from the Department of Biomedical Informatics and Division of Geriatric Medicine, University of Pittsburgh School of Medicine, the Geriatric Research Education and Clinical Center, the Veterans Affairs Pittsburgh Healthcare System; Geriatric Pharmaceutical Outcomes and Geroinformatics Research and Training Program, University of Pittsburgh; and is Medical Director, Long-Term Care Health Information Technology, University of Pittsburgh Medical Center Senior Communities, Pittsburgh, PA. Ms. Sharkey and Ms. Hudak are from Health Management Strategies Inc., Austin, TX. Dr. Ouslander is from the Charles E. Schmidt College of Medicine and Christine E. Lynn College of Nursing Florida Atlantic University, Boca Raton, FL.
Acknowledgment
We thank the nursing home staff who participated in The Commonwealth Fund–supported quality improvement project on INTERACT and provided comments that helped form the basis of this paper.
References
1. Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc. 2010;58(4):627-635.
2. Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of hospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57-64.
3. Saliba D, Kington R, Buchanan J, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48(2):154-163.
4. Grabowski DC, O’Malley AJ, Barhydt NR. The costs and potential savings associated with nursing home hospitalizations. Health Aff (Millwood). 2007;26(6):1753-1761.
5. Ouslander JG, Perloe M, Givens J, et al. Reducing potentially avoidable hospitalizations of nursing home residents: results of a pilot quality improvement project. J Am Med Dir Assoc. 2009;10(9):644-652.
6. Ouslander JG, Lamb G, Tappen R, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Amer Geriatr Soc. 2011;59(4):745-753.
7. Karsh B. Clinical practice improvement and redesign: how change in workflow can be supported by clinical decision support. Rockville, MD: Agency for Healthcare Research and Quality; 2009. AHRQ Publication No. 09-0054-EF. https://healthit.ahrq.gov/images/jun09cdsworkflow/09_0054_ef.html. Published June 2009. Accessed August 17, 2011.
8. Berner ES. Clinical Decision Support Systems: State of the Art. Rockville, MD: Agency for Healthcare Research and Quality; 2009. AHRQ Publication No. 09-0069-EF. https://healthit.ahrq.gov/images/jun09cdsreview/09_0069_ef.html. Published June 2009. Accessed August 17, 2011.
9. Eichner J, Das M; AHRQ National Resource Center for Health Information Technology. Challenges and Barriers to Clinical Decision Support (CDS) Design and Implementation Experienced in the Agency for Healthcare Research and Quality CDS Demonstrations. Rockville, MD: Agency for Healthcare Research and Quality; 2010. AHRQ Publication No. 10-0064-EF. https://healthit.ahrq.gov/portal/server.../CDS_challenges_and_barriers.pdf. Published March 2010. Accessed August 17, 2011.
10. Waitman LR, Miller RA. Pragmatics of implementing guidelines on the front lines.
J Am Med Inform Assoc. 2004;11(5):436-438.
11. Shiffman RN, Michel G, Essaihi A, Thornquist E. Bridging the guideline implementation gap: a systematic, document-centered approach to guideline implementation. J Am Med Inform Assoc. 2004;11(5):418-426.
12. Goldstein MK, Coleman RW, Tu SW, et al. Translating research into practice: organizational issues in implementing automated decision support for hypertension in three medical centers. J Am Med Inform Assoc. 2004;11(5):368-376.
13. Osheroff JA, Pifer EA, Teich JM, et al. Improving Outcomes with Clinical Decision Support: An Implementer’s Guide. Chicago, IL: Healthcare Information Management and Management Systems Society; 2005.
14. Au M, Felt-Lisk S, Anglin G, Clarkwest A; Mathematic Policy Research. Nursing Home Health IT Reduces Pressure Ulcers and Increases Staff’s Job Satisfaction. Rockville, MD: Agency for Healthcare Research and Quality; 2010. Using Health IT: Eight Quality Improvement Stories. AHRQ Publication No. 10-0102. https://healthit.ahrq.gov/portal/server.pt/.../EightSuccessStories_092810.pdf. Published September 2010. Accessed August 17, 2011.
15. Horn SD, Sharkey SS, Hudak S, et al. Pressure ulcer prevention in long-term-care facilities: a pilot study implementing standardized nurse aide documentation and feedback reports. Adv Skin Wound Care. 2010;23(3):120-131.










