Improving the Quality of Specimen Collection in Long-Term Care
More than a decade has passed since the publication of To Err Is Human: Building A Safer Health System,1 a report that brought major public attention to patient safety in healthcare. In the past 10 years, tremendous attention has been paid to reducing medical errors in healthcare, but relatively little focus has been on laboratory medicine, despite specimen collection and testing being a routine part of healthcare practice used to diagnose and monitor patients’ conditions.2 Approximately 60% to 70% of diagnostic and therapeutic monitoring relies on laboratory test results.3
In the United States, more than 160,000 medical events per year result from errors in specimen collection,4 and 19% of patients who are not adversely affected by specimen collection errors go on to receive unnecessary follow-up tests.5 A laboratory or specimen collection error is defined as “a defect occurring at any part of the laboratory cycle, from ordering tests to reporting results and appropriately interpreting and reacting on these.”1 Approximately 46% to 68.2% of these errors occur before the specimens reach the laboratory for analysis, and these are referred to as preanalytic errors.3 Physician reports indicate that 27% of specimen collection errors affect patient care5 and could potentially have devastating consequences for patients.6
Less is known about specimen collection processes in long-term care (LTC) settings, but it is clear that improper specimen collection threatens patient safety, and relevant processes of care need to be examined to prevent significant adverse events. After a specimen collection error occurred at Baycrest, we reviewed the institution’s entire process of specimen collection, from the time of ordering until the specimen is received by the laboratory, to identify shortcomings and develop recommendations for improvement.
Background
Baycrest is an academically affiliated teaching site that comprises a 472-bed nursing home, a 300-bed hospital providing LTC services for complex chronic or subacute conditions, various community care programs, and several ambulatory care clinics that, as a whole, serve approximately 2500 elderly patients. One day in 2008, a laboratory received 12 specimens that had been collected from Baycrest patients 5 days earlier. The delay in submitting the specimens made them inadmissible for testing, and the event was reported to Baycrest’s Quality and Safety Coordinating Committee. Although no patients were adversely affected by the event, it triggered a rigorous quality improvement initiative at Baycrest, with the goal of enhancing the institution’s specimen collection process.
Methodology
This project received approval from the Baycrest Research Ethics Board. The multistep analysis was limited to Baycrest’s LTC complex continuing care program for patients with chronic or subacute conditions. We selected this setting because, compared with the other LTC units at Baycrest that use the specimen collection process, the complex continuing care program includes patients with higher patient acuity, submits the most laboratory specimens, and has reported the highest percentage of laboratory incidents.
We reviewed the specimen collection process using continuous quality improvement (CQI) methodology. This holistic approach to resolving complex issues brings together staff and leadership, who rely on its selective mechanisms to assess, plan, and implement improvements.7
Since no policy was available detailing the steps in the specimen collection process, we had the team and various stakeholders gather different types of information to develop an initial understanding of how specimen collection is conducted.8 This was followed by process mapping to provide a full picture of the actual specimen collection process used at Baycrest. Process maps, also referred to as flowcharts, are powerful tools in defining, describing, and communicating clinical, administrative, and operational processes.9
To help us create the process map, coauthor Robert Fraser, who is trained in quality improvement theory, interviewed four nurses, a porter, and the director of laboratory services. The scope of the analysis focused only on specimen collection, so physicians—who are not actively involved in this process—were excluded from the process map evaluation. Taking a systematic approach, Mr. Fraser asked each subject a series of questions about procedures for transferring the specimens from one location or individual to another and the documentation process used during handoffs, such as when samples are picked up. He also asked about variations in how the collection process is performed and sought to clarify discrepancies in descriptions of the process between personnel. In addition to informing development of the process map, answers were clustered into categories and incorporated into a fishbone diagram to help identify patterns in the specimen collection process (Figure 1).8
The final part of the assessment involved analyzing data from electronic incident reports10 filed between April 2009 and March 2010 to determine the origin and nature of specimen collection errors at Baycrest. These rates were compared with those in the published literature.

Summary of Results
Based on this multistep evaluation, we identified several breakdowns in the specimen collection process. First, during the review, it became clear that handoffs of the sample between the individual roles created opportunities for errors. Second, the evaluation revealed Baycrest’s lack of an organizational policy governing specimen collection. Third, a retrospective data analysis identified errors in physician ordering and a marked increase in errors for specimens delivered to the off-site laboratory.
The Specimen Collection Process
We used the information obtained during the interviews to map the perceived steps of the specimen collection process, starting with the requisition order for the specimen through its collection and delivery to the laboratory (Figure 2). The map showed that the specimen collection process at Baycrest involves multiple steps and requires many handoffs of the specimen between various members of the hospital staff.
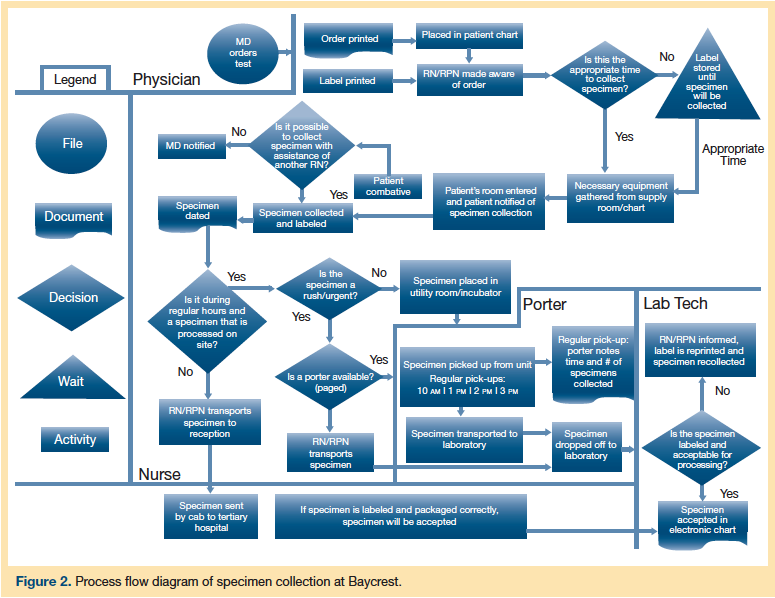
The physician initiates the process by creating the order, which is printed along with a label for the specimen. The nurse acknowledges receipt of the order and prioritizes all orders received. Next, he or she gathers the necessary equipment and collects the specimen, which may involve dealing with a challenging patient, such as someone who is cognitively impaired. Once the specimen has been obtained, the nurse affixes the label, dates the sample, and decides how to store and/or deliver the specimen to the appropriate laboratory, based on when the sample was collected. During regular hours, the porter retrieves the specimen and transports it to the onsite laboratory technician; during off-hours, the nurse takes the specimen to the reception desk and it is sent via courier to an off-site laboratory at a remote tertiary care hospital.
On arrival at the Baycrest laboratory, the specimen is inspected for proper labeling and matched to the corresponding order. If the information is deemed accurate, it is entered into the computer and processed. The remote hospital’s laboratory generally uses the same procedures and pathways, except when there is a problem with the specimen (eg, it is improperly labeled). The Baycrest laboratory knows which unit the specimen comes from and will notify the responsible nurse if possible, triggering reprinting of the label and collection of a fresh specimen from the patient. The remote hospital, however, receives samples from many institutions and therefore has elected not to acknowledge improperly labeled specimens. It also does not contact relevant personnel or enter data on the specimen into the system. The nurse learns there is a problem when no results become available.
Subjects were questioned further to explore expected and unexpected interruptions or deviations in the specimen collection process that might cause it to fail.9 Based on responses, we identified several categories with the potential for errors: training, environmental/equipment, policies/procedures, communications, fatigue/scheduling, and other barriers. The fishbone diagram (Figure 1) we developed using these categories reinforced the potential for labeling errors and the lack of documentation with the collection process.
Retrospective Data Analysis
From April 2009 through March 2010, the LTC hospital collected 72,918 specimens. Our analysis of incident reports revealed 183 errors in this 12-month period, for an error rate of 0.25%. The unit with the greatest volume of specimens collected also had the highest error rate, at 0.46% (56/12,229). The Baycrest laboratory closes at 4 pm, requiring some specimens to be sent to the tertiary care hospital for analysis. Of the 183 total errors that occurred, 40% involved specimens sent to the tertiary care hospital. Most errors related to a collection issue (eg, incorrect tube) or incorrect requisition (27% and 27%, respectively). Other causes for errors were unlabeled specimens (14%), a delay in transporting the specimen (8%), a missed test (7%), an incomplete physician order (6%), and other (11%). These error rates were consistent with those we observed in the literature, with the majority of errors arising in the preanalytic phase of the collection process and lower proportions of errors occurring during the analytic and postanalytic phases.11
Discussion
After the 2008 incident in which 12 specimens collected at Baycrest were unable to be tested, we set out to identify areas of concern and potential improvements related to the facility’s specimen collection process with the goal of enhancing patient safety. This involved a review of the literature for evidence-based recommendations on addressing patient safety issues associated with specimen collection errors. Evidence-based recommendations we adopted were conducting a review of the specimen collection process and designing recommendations tailored to the practice setting.12
One of our first steps was to interview the staff, which generated rich data about Baycrest’s specimen collection process. It was clear that Baycrest had no formal policy on specimen collecting for the staff to follow or that they could refer to when concerns arose. Other potential pitfalls that were immediately apparent included problems with handoffs, inadequate supplies, and the lack of documentation. It also quickly became evident that variation existed between staff members as to how specimens were collected and delivered and that this extended to the nursing staff.
The process review led to a best practices–based action plan consisting of four components. We recommended writing a new policy on the specimen collection process, because creating a policy increases standardization and reduces variability in execution of a process.13 Since the majority of errors were human-related, we advised conducting tests of the ordering and collection procedures and reorganizing education and staff training based on the new policy.6 Up to 40% of off-site specimens resulted in errors, so we suggested collaborating with physicians to identify those tests that need to be collected after hours and working with the nursing staff to improve order entry and handoff processes.4 We proposed enhancing the computer order entry system to reduce errors14 and changing the label printing process to minimize mislabeling of specimens.
The plan was implemented as a pilot project in the unit with the greatest volume of specimen collecting, and the pilot ran from May 9, 2011, to June 17, 2011. Following CQI methodology,7 key components that contributed to the pilot’s success were engagement of frontline staff (eg, nurses, porters) in developing the pilot; rapid-cycle, weekly evaluations with immediate implementation of improvements and sharing results with staff (posting graphs of errors and collection times) each week; and using Plan-Do-Study-Act cycles until the new process became standardized.7 During the 6-week pilot, the unit submitted 973 specimens and reported only three specimen collection errors, for an error rate of 0.31%—a reduction from the baseline error rate of 0.46%.
We surmise that the pilot project successfully reduced errors because it was based on developing consistent and systematic processes that changed clinical practice on the unit and eliminated unnecessary steps, while ensuring that all staff members were educated on the new process. Having frontline staff, including nurses and porters, engaged in the process as key stakeholders was a positive experience. The weekly evaluation of error occurrences was imperative in allowing us to make small but useful adjustments to the processes and for addressing educational needs. Plans for rollout across the organization are under way, with significant support from administration.
Conclusion
Specimen collection is a highly complex process that relies on the effective participation of multiple healthcare providers and staff. Changes in our understanding of the laboratory errors helped us recognize the human factors that contributed to significant variation in how the collection process was carried out.2 Using the CQI process offers LTC organizations such as Baycrest an opportunity to address the root cause of these errors by providing a systematic, transparent, nonpunitive approach to understanding the problem.
The authors report no relevant financial relationships.
Dr. Wagner is assistant professor, New York University College of Nursing, New York, NY. Mr. Fraser is a recent graduate of the Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, and is principal consultant, Rob D. Fraser & Associates, Inc. Dr. Huijbregts is director of clinical performance and accreditation, Baycrest Geriatric Health Care System, and assistant professor, Department of Physical Therapy, University of Toronto. Ms. Sokoloff is professional practice chief, Baycrest Geriatric Health Care System, and lecturer, Department of Speech-Language Pathology, University of Toronto. Ms. Chang is patient safety coordinator, Rouge Valley Health System, Toronto, Ontario, Canada.
References
1. Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building A Safer Health System. Washington, DC: National Academy Press; 2000.
2. Plebani M, Lippi G. To err is human. To misdiagnose might be deadly. Clin Biochem. 2010;43(1-2):1-3.
3. Plebani M. Errors in clinical laboratories or errors in laboratory medicine. Clin Chem Lab Med. 2006;45(6):750-759.
4. Shortell SM, Singer SJ. Improving patient safety by taking systems seriously. JAMA. 2008;299(4):445-447.
5. Lippi G, Blanckaert N, Bonini, P, et al. Causes, consequences, detection and prevention of identification errors in laboratory diagnostics. Clin Chem Lab Med. 2009;47(2):143-153.
6. Wagar EA, Tamashiro L, Yasin B, et al. Patient safety in the clinical laboratory: a longitudinal analysis of specimen identification errors. Arch Pathol Lab Med. 2006;130(11):1662-1668.
7. McLaughlin CP, Kaluzny AD. Defining quality improvement. In: McLaughlin CP, Kaluzny AD, eds. Continuous Quality Improvement in Healthcare Theory, Implementation, and Applications. 3rd ed. Boston, MA: Jones and Bartlett; 2006:3-40.
8. Hoffman C, Beard P, Greenal J, U D, White J. Canadian Root Cause Analysis Framework: a tool for identifying and addressing the root causes of critical incidents in healthcare. www.patientsafetyinstitute.ca/English/toolsResources/rca/Documents/March%202006%20RCA%20Workbook.pdf. Published March 2006. Accessed September 23, 2011.
9. Kelly DL, Johnson SP. Measurement and statistical analysis in CQI. In: McLaughlin CP, Kaluzny AD, eds. Continuous Quality Improvement in Healthcare Theory, Implementation, and Applications. 3rd ed. Boston, MA: Jones and Bartlett; 2006:95-130.
10. Wagner LM, Capezuti E, Taylor JA, et al. Impact of a falls menu-driven incident reporting system on documentation and quality improvement in nursing homes. Gerontologist. 2005;45(6):835-842.
11. Plebani M. Exploring the iceberg of errors in laboratory medicine. Clin Chim Acta. 2009;404(1):16-23.
12. Plebani M. Errors in laboratory medicine and patient safety: the road ahead. Clin Chem Lab Med. 2007;45(6):700-707.
13. Watson DS, Crum BG. Improving specimen practice to reduce errors. AORN J. 2005;82(6):1051-1054.
14. Wallin O. Preanalytical errors in hospitals. Implications for quality improvement of blood sample collection [dissertation]. Sweden: Umeå University; 2008.










