How to Be Included in a Health System’s Preferred SNF Network
As health systems increase their focus on population health through risk-based coordination, they are looking to manage their postacute care more aggressively, especially through selection of a preferred group of skilled nursing facilities (SNFs) to work more closely with. The value of health system-preferred SNF networks was illustrated in a recent study in Health Affairs.1 In the article, researchers studied several hospitals that had developed formal SNF networks as part of their care management efforts. These hospitals saw a relative reduction from 2009 to 2013 in readmission rates for patients discharged to SNFs that was 4.5 percentage points greater than the reduction for hospitals without formal networks. Overall, researchers found that establishing preferred SNF provider networks is one approach hospital administrators are using to reduce excess 30-day readmissions and avoid Medicare penalties or to reduce beneficiaries’ costs as part of value-based payment models.
By appreciating the focus and execution plan of health systems in the process of choosing their preferred SNF networks, leaders at SNFs can better understand how to become a successful health system partner and subsequently improve care for their residents along the way.
Basis for Preferred SNF Selection
Figure 1 contains an adaptation of a letter sent by a health system, Meadow Creek Healthcare System, to an area SNF after they had evaluated the facility as a potential preferred SNF. This correspondence illustrates the basis of selection for a preferred provider and specific areas of opportunity for improvement. While all health systems will have their own individual process, most will concentrate on these same critical elements when choosing a preferred network. SNF leaders can proactively ready their facility in the key areas discussed in the letter.
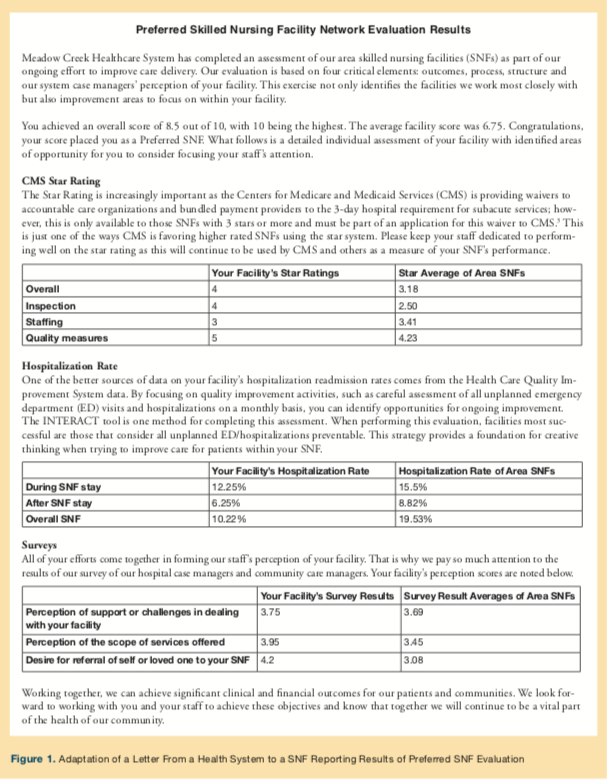
After Becoming a Preferred SNF
Once established, each health system’s preferred SNF network will be deemed successful on the basis of a panel of measurable outcomes. These accountability measures will likely be centered on the following:
Measures of Success
The measure of success of many health system’s SNF network is based on clinical and financial outcomes. These accountability measures focus primarily on keeping patients safe in the SNF and community. The measures considered include those in Table 1.
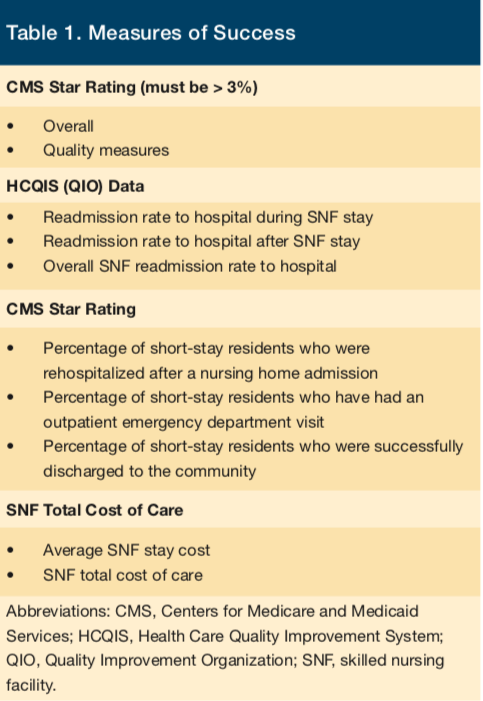
Note that these measures rely heavily on each SNF being able to successfully care for patients in their facility, which includes transitioning them to their homes in the community. These efforts depend on each SNF having the resources and skilled staff to provide the level of care needed to recognize and treat issues rather than allowing them to escalate to require a hospitalization. A central component of delivering this care is having a process in place to identify opportunities to prevent avoidable emergency department (ED)/hospital utilization—one such method is use of the INTERACT tool.2
Health systems often strongly recommend that all unplanned ED/hospitalizations undergo a thoughtful analysis to identify opportunities to prevent future occurrences. This activity typically reveals care improvement opportunities related to end-of-life planning or access to medical evaluation. Once an area is identified, a plan can then be put into place to address the perceived problem, such as maintaining physician orders for life-sustaining treatment forms for all residents, using virtual after-hour medical services, or having a dedicated advanced practical nurse available to care for all facility residents.
Also of note is the Centers for Medicare and Medicaid Services (CMS) Star Rating and total cost of care measures. These are a direct result of health systems increasingly taking on financial responsibility for care outside of the hospital through bundled payments, accountable care organizations (ACOs), and other risk arrangements. Thus, managing total cost of care is critical for success in these arrangements. The CMS Star Rating is important as CMS is allowing ACOs to apply for a waiver for the 3-day hospital requirement for Medicare Part A skilled services. This provides the opportunity for ACO patients to be directly admitted to a SNF or admitted to a SNF after an inpatient hospitalization of fewer than 3 days. As one can imagine, this can increase the use of SNFs while reducing the use of hospitals, providing an opportunity for improved clinical and financial outcomes, which, again, is the ultimate measure of success.
References
1. McHugh JP, Foster A, Mor V, et al. Reducing hospital readmissions through preferred networks of skilled nursing facilities. Health Aff. 2017;36(9):1591-1598.
2. Pathway Health Services. Quality improvement tool for review of acute care transfers-INTERACT version 4.0 tool. Pathway Health website. https://www.pathway-interact.com/wp-content/uploads/2017/04/148604-QI_Tool-for-Review-Acute-Care-Transf_AL.pdf. Access September 21, 2017.
3. Centers for Medicare and Medicaid Services (CMS). Skilled nursing facility 3-day rule waiver. CMS website. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-
Payment/sharedsavingsprogram/Downloads/SNF-Waiver-Guidance.pdf. August 2017. Accessed September 21, 2017.










