Diagnosing a Cutaneous Horn on an Elderly Woman`s Face - Answer and Discussion
Answer: Actinic keratosis (C)
Actinic keratosis, also known as solar keratosis, is a premalignant skin lesion that may occasionally progress to invasive squamous cell carcinoma. Up to 60% of squamous cell carcinomas develop from actinic keratosis.1 The prevalence of actinic keratosis increases with age, and men are more likely than women to develop these lesions. The incidence is highest in Australia and in the geographic southern United States (ie, the “Sun Belt”).2 Long-term sun exposure is a major risk factor for the development of actinic keratosis, and lesions typically arise on areas of the body with the most exposure to the sun, such as the face, bald scalp, ears, forearms, and dorsal surfaces of the hands.3 Actinic keratosis is generally asymptomatic and can develop as solitary or multiple lesions that vary in size, from small rough spots to elevated, hyperkeratotic plaques several centimeters in diameter.4 Sometimes actinic keratosis can be associated with an overlying cutaneous horn as a clinical variant.2 The mound of compact keratin often resembles a spicule or cone.

Cutaneous horns are conical, dense projections of keratin, occurring most commonly in light-skinned patients older than 50 years. They usually appear on sun-exposed areas, particularly the upper face and scalp. No rates of incidence or prevalence have been reported.3 Most cutaneous horns are yellow-white; they can be straight or curved; and they vary in size, from a few millimeters to many centimeters long. Patients typically present with an irregular mass that has enlarged over years. Cutaneous horns can be derived from various types of benign lesions (eg, seborrheic keratosis, keratoacanthoma, viral warts, molluscum contagiosum), premalignant lesions (eg, actinic keratosis, Bowen’s disease), or malignant skin lesions (eg, squamous cell carcinoma, basal cell carcinoma, Kaposi’s sarcoma).5,6 Most histopathological studies show the majority of cutaneous horns are associated with premalignancy or malignancy, and the most common finding is actinic keratosis.7 The presence of erythema around the base, inflammation, or tenderness is an indication of malignancy.3
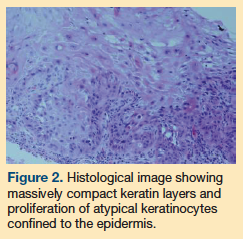
The primary histologic feature of actinic keratosis is atypia or dysplasia of keratinocytes typically confined to the basal layers of the epidermis (Figure 2).
Case Patient Outcome
In our patient, pathohistology was reported as actinic keratosis. Because the cutaneous horn was completely excised with safety margins, no further treatment was done. On follow-up, no clinical relapses were detected after 2 years.
Differential Diagnosis
Even though more than half of cutaneous horns are benign,8 it is important to determine the underlying cause and rule out malignancy. The differential diagnosis of actinic keratosis includes acrochordons, basal cell carcinoma, seborrheic keratosis, and nongenital warts. It is essential for clinicians to recognize these lesions to ensure correct diagnosis and therapeutic interventions.
Acrochordons. Commonly known as skin tags, acrochordons are often seen in areas where the skin forms creases, such as on the neck, the axillae, and the eyelids. The risk of developing skin tags increases with age, affecting as many as 59% of people by the age of 70 years.9 They are typically brown or flesh-colored and range in size from 1 mm to 1 cm. The lesions are pedunculated (ie, attached to the skin by a thin stalk), but they may also be sessile.10 Skin tags pose no malignant potential in adults, but may be removed with excision or cryotherapy for cosmetic reasons.
Basal cell carcinoma. Basal cell carcinoma is common in white men and woman and appears to be increasing due to the rise in sun exposure and ultraviolet radiation from artificial tanning.11 Most cases of basal cell carcinoma occur on the face and present as a slow-growing pink or flesh-colored nodule with a waxy, pearly quality. The presence of telangiectasias is also common, leading to friability, poor healing, and frequent bleeding. Central ulceration with a pale, raised border can be found frequently.2,11 Clinicians who suspect basal cell carcinoma based on these hallmark physical characteristics should perform a biopsy or refer the patient to a specialist as needed, as treatment is based on tissue diagnosis.11
Seborrheic keratosis. Seborrheic keratosis is the most common benign tumor in the elderly. Risk factors include age older than 40 years and a family history.12 They represent a benign proliferation of immature keratinocytes. The lesion usually arises on the trunk, scalp, and face, particularly along the frontal hairline. The typical seborrheic keratosis has a characteristic wart-like “stuck-on” appearance and ranges in color from tan to dark brown to black.2 Most lesions have a rough, dry, and crumbly surface with a well-circumscribed border.10 Seborrheic keratosis eventually progresses from an initial hyperpigmented macule to the typical plaque. Treatment is indicated for cosmetic reasons, to decrease irritation, or to rule out malignancy.
Nongenital warts. Nongenital warts are caused by human papillomavirus (HPV) infection. They are more frequently seen in school-aged children, with a peak incidence in the teenage years. Nongenital warts are rarely seen in older adults and the elderly; however, it has been shown that risk of reactivation of the HPV virus may increase around age 50 years.13 Nongenital warts vary widely in shape, size, and appearance.2 Filiform warts, for example, may present as horns on the face, but the horn is slender and usually occurs around the lips, eyelids, or around the nose.2,14
Approaches to Treatment
The recommended treatment of cutaneous horn is surgical excision followed by histologic examination to confirm the specific diagnosis and to guide further management.3,5 If actinic keratosis is diagnosed, treatment is usually chosen by the number of lesions present, age of the patient, history of skin cancer, and tolerability of the treatment modality (eg, topical agents, photodynamic therapy, surgical therapy).15
References
1. Marks R, Rennie G, Selwood TS. Malignant transformation of solar keratoses to squamous cell carcinoma. Lancet. 1988;1(8589):795-797.
2. Goodheart HP. Goodheart’s Photoguide of Common Skin Disorders: Diagnosis and Management. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003.
3. Fernandes NF, Sinha S, Lambert WC, Schwartz RA. Cutaneous horn: a potentially malignant entity. Acta Dermatovenerol Alp Panonica Adriat. 2009;18(4):189-193.
4. Schmitt JV, Miot HA. Actinic keratosis: a clinical and epidemiological revision. An Bras Dermatol. 2012;87(3):425-434.
5. Sathyanarayana SA, Deutsch GB, Edelman M, Cohen-Kashi KJ. Cutaneous horn: a malignant lesions? A brief review of the literature. Dermatol Surg. 2012;38(2):285-287.
6. Gil-Mosquera M, Vano-Galvan S, Gómez-Guerra R, Jaén P. A cutaneous horn on the ear. Aust Fam Physician. 2009;38(3):118.
7. Mantese SA, Diogo PM, Rocha A, Berbert AL, Ferreira AK, Ferreira TC. Cutaneous horn: a retrospective histopathological study of 222 cases. An Bras Dermatol. 2010;85(2):157-163.
8. Larsen F. Cutaneous horn pathophysiology. Medscape. https://emedicine.medscape.com/article/1056568-overview#a0104. Updated January 12, 2012. Accessed August 20, 2014.
9. Schwartz RA. Acrochordon epidemiology. Medscape. https://emedicine.medscape.com/article/1060373-overview#a0199. Updated September 4, 2013. Accessed August 20, 2014.
10. Luba MC, Bangs SA, Mohler AM, Stulberg DL. Common benign skin tumors. Am Fam Physician. 2003;67(4):729-738.
11. Stulberg DL, Crandell B, Fawcett RS. Diagnosis and treatment of basal cell and squamous cell carcinomas. Am Fam Physician. 2004;70(8):1481-1488.
12. Scheinberg D. Seborrheic keratosis. New York University Department of Medicine website. Updated June 2013. Accessed August 1, 2014.
13. Brown DR, Weaver B. Human papillomavirus in older women: new infection or reactivation? J Infect Dis. 2012. Published online December 12, 2012.
14. Vañó-Galván S, Marqués A, Muñoz-Zato E, Jaén P. A facial cutaneous horn. Cleve Clin J Med. 2009;76(2):92-95.
15. Spencer JM. Actinic keratosis treatment and management. Medscape. https://emedicine.medscape.com/article/1099775-treatment#a1128. Updated March 12, 2014. Accessed August 19, 2014.
Disclosures: The authors report no relevant financial relationships.
Address correspondence to:
I-Chiang Shy, MD, MA
Attending Physician
Department of Family Medicine
Kuang-Tien General Hospital
117 Shatian Road
Shalu District, Taichung City
Taiwan
shyichiang@gmail.com










