Bipolar Disorder in Long-Term Care
Bipolar disorder (BD) is a chronic illness characterized by periods of mania and depression. As many as 10% of skilled nursing facility (SNF) residents suffer from BD. In the elderly, BD is associated with significant comorbidity—often cardiovascular and metabolic disorders—and increased mortality. Treatment of BD is complex and is generally managed by a psychiatrist, but geriatricians and the entire SNF treatment team play important roles in managing these patients. While there are few controlled studies of treatment of BD specifically in the elderly, mood stabilizers (lithium, valproate, carbamazepine, lamotrigine) remain the cornerstone of treatment. Atypical neuroleptics may also be used. Antidepressants should be used with great caution due to risks of destabilization.
Key words: bipolar illness, mania, depression, mood disorders, mood stabilizers
Bipolar disorder (BD) is a relatively common and potentially debilitating mental illness characterized by discrete periods of mania or hypomania and periods of depression. BD is a complex disorder with manifold presentations and frequent comorbidity. It is generally a challenge to manage BD at any age but particularly in older adults. Because these patients are often cared for in long-term care facilities (LTCFs), this presents a unique set of difficulties for the geriatrician, as well as for the entire treatment team.
Up to one-quarter of all patients with BD are over 60 years of age.1 The prevalence of BD in the elderly is conservatively estimated at 0.5% to 1% in the community setting2 and possibly as high as 10% among those living in skilled nursing facilities (SNFs).3 BD is likely to become more prevalent in SNFs as there is a trend toward more SNF placements for patients with serious psychiatric illness.4 Furthermore, BD itself is a risk factor for SNF placement.5
Older patients with BD have greater medical comorbidity than their peers, with age-adjusted life expectancy reduced by about 10 years.2 Patients with BD have an increased prevalence of obesity, cardiovascular, and metabolic disorders,6,7 cerebrovascular disease,6 substance abuse (although less so than younger patients with BD8), and have often suffered prolonged periods of depression with their attendant complications of immobility and poor nutrition. Indeed, current literature suggests that the majority of the morbidity seen in BD can be attributed to the depressive episodes.2,8 Also, patients with BD often have poor access to health care, may be poorly compliant, and are often offered inadequate evaluation and treatment.9 Finally, older patients with BD are at increased risk for suicide, although their risk is lower than that of younger patients with BD; this is likely a survivor cohort effect.2
As is the case with most illnesses in the elderly, geriatric BD often presents with atypical or inconspicuous symptomatology and may mimic other conditions, notably delirium, dementia, or unipolar depression. Conversely, numerous medical and iatrogenic conditions may mimic BD. Invariably, treatment of BD in older adults in LTCFs should be individualized based on the patient’s medical conditions, functional status, and level of compliance.
Diagnosis of BD in Older Adults
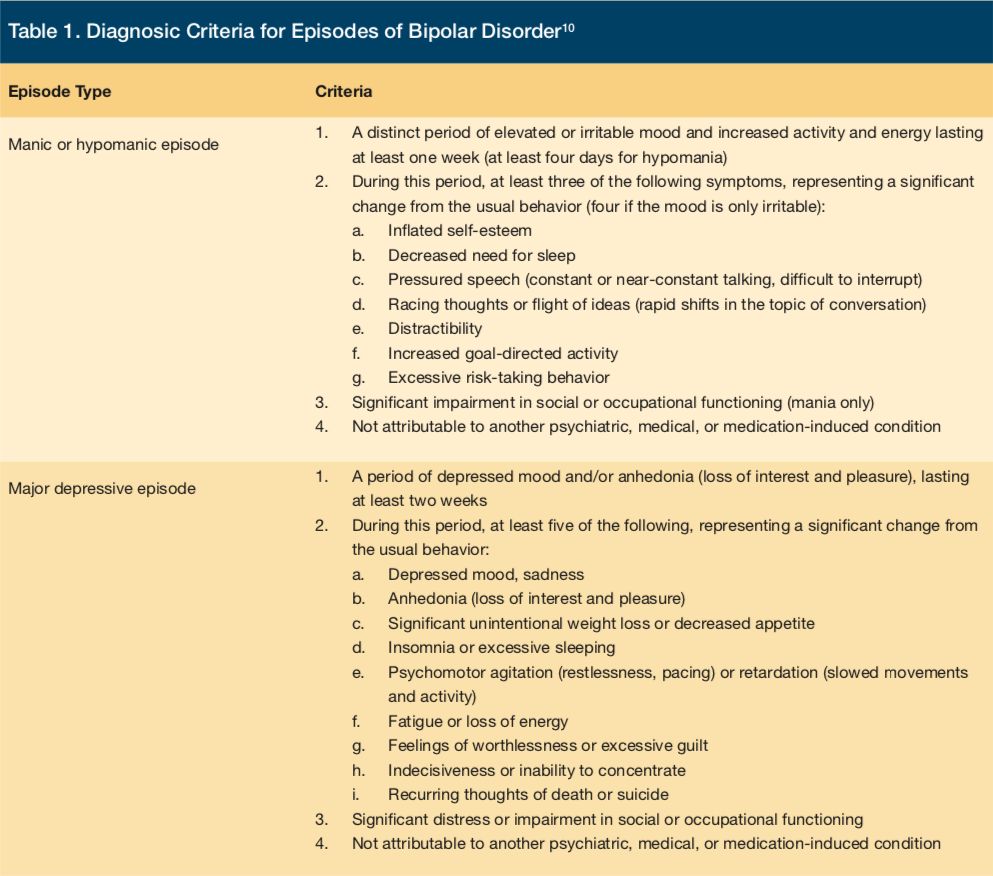
Criteria for manic/hypomanic episodes and for major depressive episodes associated with BD, adapted from the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5),10 are listed in Table 1. Patients with only periods of serious depression suffer from unipolar major depression and are treated differently than patients with BD; it is this history of periods of mania or hypomania that distinguishes BD from unipolar major depression. The term “bipolar depression” refers to the depressive episodes in BD. In both mania and depression, the symptoms are to be of such severity as to significantly impair social or occupational functioning or to necessitate hospitalization. They cannot be attributable to prescribed or illicit substances or a medical condition, and they are not better explained by a different psychiatric illness.
A challenge to diagnosis is that patients and family members often fail to remember prior episodes of mania, especially in the midst of a depressive episode. This can lead to an incorrect diagnosis of unipolar depression. Because BD is treated differently than unipolar depression, and treatment of BD with an antidepressant carries risks of destabilization and precipitation of a manic episode, the distinction between these two diagnoses is essential.
Differental Diagnoses
While the diagnosis of BD is often obvious from clinical presentation, and especially from longitudinal history, a cautious diagnostic approach is necessary in older adults due to the increased likelihood of comorbid medical, neurologic, or iatrogenic conditions that may either cause so-called “secondary mania” or mimic BD.
The concept of secondary mania was first introduced in 1978 by Krauthammer and Klerman11 to describe patients with a variety of medical conditions but no previous personal or family history of BD whose presentations were indistinguishable from mania observed in patients with primary BD. Important neurologic causes of secondary mania include seizure disorder, stroke, head trauma, and central nervous system tumors, especially involving the right hemisphere.12 Depression is also commonly seen following stroke—more often following left hemispheric stroke—whereas post-stroke mania is rarer and almost exclusively due to right hemispheric stroke.12,13 As an additional confound, strokes involving the frontal lobes and associated subcortical structures can cause disinhibition and impaired judgment, mimicking mania.13 Other medical problems may occasionally cause secondary mania, notably hyperthyroidism;12 however, some older hyperthyroid patients will paradoxically develop depression, so-called “apathetic hyperthyroidism.”14
Iatrogenic, or treatment-induced, mania is often encountered as well. Corticosteroids are a common cause of such mania; up to 10% of patients on steroids (generally in doses equivalent to > 20 mg/d prednisone) will develop serious psychiatric symptoms, most often mood symptoms.12,15 Mania generally occurs early in the course of treatment; after about 6 weeks, depression becomes more common.15 Other potential iatrogenic causes of mania include psychostimulants, levodopa and dopamine agonists, and various commonly abused substances (most notably cocaine and amphetamines).12 All antidepressants have the potential to precipitate mania in bipolar patients;7,8,12,16,17 sometimes the first evidence of BD is a manic episode in a patient being treated for what appeared to be unipolar depression.
Several neurologic and psychiatric conditions may mimic BD and must be considered in the differential diagnosis. Borderline personality disorder, schizophrenia, and a variety of anxiety disorders are probably the most common psychiatric conditions confused with BD.12,18 Neurologic conditions that mimic BD include most dementias—especially those that affect the frontal/subcortical system and can cause disinhibition—and agitated delirium. Occasionally, Wernicke’s aphasia or other fluent aphasia will be mistaken for pressured speech, leading to an erroneous diagnosis of mania.19
Atypical Presentations of BD
As is typical in geriatric practice, atypical presentations of BD are more the rule than the exception. During depressive episodes, older patients often deny sadness or low mood.20 During manic episodes, irritability rather than grandiosity is seen more often in elderly patients.16,21 Some manic symptoms, such as exaggerated spending and increased activity, may be difficult to accomplish for an institutionalized patient. Also, in older patients, mania may convincingly mimic delirium, so-called “pseudodelirious mania.”22 On the other hand, agitated or lethargic delirium due to an acute medical problem is sometimes incorrectly attributed to the patient’s BD history.9 Mixed mood episodes, with concurrent manic and depressive symptoms, are more commonly seen in older patients with BD16 and can be very difficult to diagnose. Older patients with BD, especially those with early-onset disease, may present a confusing, rapid-cycling picture (defined as four or more mood episodes per year), which may be difficult to treat.7,8,16
Early- vs Late-Onset BD
Onset of BD is typically in early adulthood, but the illness may begin at any age; ~10% of BD is late-onset BD, which is generally, but not universally, defined by the first manic episode occurring after age 50 years.2,8 Full remission is very rare or nonexistent; the myth that BD “burns out” in old age has clearly been disproven,12 and patients with BD require lifelong management.
The clinical presentation of late-onset patients is generally indistinguishable from that of early-onset geriatric patients,2,12 but there are some key differences in risk factors and longitudinal course between the two groups. Early-onset geriatric patients have had a BD diagnosis for longer than late-onset patients and have usually had more mood episodes and more time spent in depressive episodes. These patients tend to have a more chronic and persistent course of illness, higher risk for refractoriness, and more psychiatric comorbidity than late-onset patients.23 As mentioned above, early-onset patients are more likely to manifest a rapid-cycling pattern; this may be a reflection of long-duration illness.7,8,16 In addition, early-onset patients are more likely to have a family history of mood disorders than late-onset patients,2,8 although many late-onset patients also have a family history.8
In contrast, patients with late-onset BD tend to have a more fragile recovery than early-onset patients,16 and their depressive episodes may be less responsive to mood stabilizers.24 Late-onset patients have a higher prevalence of cognitive dysfunction and a higher risk for rapid cognitive decline than early-onset patients.2,8 Also, late-onset patients are more likely to manifest “secondary mania” related to medical, neurologic, or iatrogenic illness.11 Finally, late-onset patients with BD have a higher prevalence of cerebrovascular pathology—notably, white matter hyperintensities—than early-onset patients or age-matched controls.2,6 In addition, older patients with BD have an excess of vascular risk factors6,7 and double the risk for stroke of age-matched controls.25
Management of BD
Spontaneous remission or “cure” of BD is extremely rare and probably nonexistent;12 all patients require lifelong treatment. Management of BD is a team effort. BD should almost always be managed by a psychiatrist, but the geriatrician or advanced registered nurse practitioner will need to be familiar with signs and symptoms of decompensation and with maintenance treatment. On-site mental health personnel will have a crucial role in monitoring the patient, providing psychotherapy as well as patient, family, and staff education. The social worker can be of tremendous help in providing family support and education and in gathering past history. All staff, especially front-line nursing staff, should be well versed in signs and symptoms of emerging mania or depression. In those instances, it will first be essential to rule out covert medical problems and the BD “mimics” (notably delirium) mentioned above. Compliance with psychotropic medications should be verified and serum levels of mood stabilizers checked. It is of paramount importance to ask about suicidal ideation. Most patients in an acute mood episode will be promptly referred to and managed by a psychiatrist.
A basic principle in the management of BD is the avoidance of the use of antidepressants when possible. The preponderance of evidence suggests that antidepressants, especially the older tricyclic antidepressants, can destabilize bipolar patients by precipitating manic episodes or rapid cycling.7,8,12,16,17 This “switch phenomenon,” whereby prescription of an antidepressant to a depressed patient with BD rapidly (often in a matter of days) leads to a manic or hypomanic episode, is probably not as common as was once believed and may be less common in older patients with BD but must always be considered.7,8 Overall, antidepressants will have a limited role in the management of BD, especially in long-term management. Again, the use of antidepressants is best left to the discretion of a psychiatrist.
BD Treatment
To date, there are very few randomized controlled trials of pharmacologic treatment of BD in the elderly, and most data is extrapolated from studies of younger patients. That being said, mood stabilizers remain the cornerstone of treatment and maintenance. Lithium has been a mainstay of treatment of bipolar illness for over 40 years, although it may be difficult to use in older patients, especially in those with renal impairment.8 A single as-yet unpublished prospective study of mood stabilizers in the elderly showed that lithium and valproate were both effective, with lithium slightly more effective for the reduction of mania scores.26 The target serum level for treatment and maintenance is generally in the 0.6–1.2 mEq/L range. Lithium is eliminated by the kidney and should be used with extreme caution in patients with chronic kidney disease. Lithium can also cause nephrogenic diabetes insipidus and, with long-term use, tubulointerstitial nephritis, although this rarely progresses to dialysis dependence.27 The most important drug-drug interactions with lithium are those that decrease renal clearance and lead to toxicity; the most important offenders are thiazide diuretics, nonsteroidal anti-inflammatory drugs, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers.28 Perhaps the most common precipitant of lithium toxicity, though, is dehydration. Symptoms of lithium toxicity include coarse tremor, ataxia, weakness, vomiting, and diarrhea; however, in older patients, it is common for symptoms to be limited to weakness and confusion.28 Other important adverse effects of lithium include mild tremor, hypothyroidism or euthyroid goiter, hypercalcemia, mild peripheral edema, and benign leukocytosis.28 There is compelling evidence that lithium can lose its efficacy when stopped and restarted;29 this has not been reported with other mood stabilizers but is obviously of concern. Thus, drug holidays should never be considered in any patient with BD, and institutionalized patients should be educated about the danger of refractoriness after a period of noncompliance.
Currently, valproic acid and divalproex are probably more commonly used than lithium and are easier to manage in elderly patients. Target serum level is generally 50-100 mcg/ml. Common adverse effects include tremor, weight gain, nausea, and dose-related thrombocytopenia or pancytopenia.28 Transaminitis may occur with valproate but is rare in adults;29 hyperammonemia, on the other hand, is very common and is related to inhibition of the urea cycle, not to hepatotoxicity.28,30 Hyperammonemia is usually benign and asymptomatic but occasionally leads to hyperammonemic encephalopathy and is therefore part of the differential diagnosis of delirium in patients taking valproate.30
There has been ample evidence of the efficacy of carbamazepine in BD for at least 35 years, although, to date, only one form of extended-release carbamazepine (Equetro®; Validus Pharmaceuticals) has received US Food and Drug Administration (FDA) approval for this indication.28 Target serum level is 7-12 mcg/ml. Carbamazepine has not specifically been studied in elderly patients with BD and can be difficult to use due to its numerous, serious drug-drug interactions.28 Moreover, carbamazepine can affect its own metabolism, leading to the phenomenon of autoinduction whereby serum levels decrease significantly during the first few weeks of treatment, necessitating dosage increases.28 Other significant adverse effects include ataxia and sedation, hyponatremia due to the syndrome of inappropriate antidiuretic hormone, and rare agranulocytosis.28
Lamotrigine has been FDA-approved for treatment of BD since 2003 and seems particularly effective for prevention of depressive relapse; this was borne out by a secondary analysis of older patients with BD taken from two clinical trials.31 Target dose is generally around 200 mg/d; serum levels are not followed. Lamotrigine is generally well-tolerated. The greatest concern with lamotrigine is the potential for development of Stevens-Johnson syndrome or toxic epidermal necrolysis.28,32 These are serious desquamating dermatitides, characterized by a rash progressing to epidermal detatchment, ulceration of mucus membranes, and fever. Mortality can be as high as 5% in Stevens-Johnson syndrome and as high as 25% to 30% in toxic epidermal necrolysis; treatment involves immediate discontinuation of the drug and supportive care, generally in a burn unit. The incidence of serious rash is around 0.1% to 0.3% in adults and can be minimized with slow dose titration as per guidelines.32
Atypical neuroleptics have been used for many years in BD mostly as adjunctive agents, and there have been a few promising controlled trials in the elderly.33,34 Typical adverse effects include extrapyramidal side effects, sedation, anticholinergic effects, and metabolic syndrome.28 The increase in stroke risk and all-cause mortality reported in elderly patients with dementia has not been reported in BD.
The role of psychotherapy has not been studied extensively in older patients with BD and has mostly been extrapolated from studies of younger patients. Psychotherapy does seem to improve a variety of clinical outcomes; cognitive behavioral therapy, family therapy, psychoeducation, and interpersonal therapy have all shown benefit.8,28 Interventions aimed at improving medication compliance seem particularly effective and have been studied in a few small samples of elderly patients with BD.2,8
Conclusion
As the population of patients with serious chronic mental illness ages, and as more patients with serious mental illness are placed in SNFs, the LTC practitioner will be increasingly likely to be a front-line provider for patients with BD. It is essential to be aware of a patient’s BD diagnosis and to consider the possiblilty of BD in patients for whom only a history of depression has been reported. The clinician will need to be aware of the various conditions that can mimic either mania or depression (delirium being the most important of these) and will often need to monitor mood stabilizer blood levels and medication compliance. At the same time, all LTC staff should be vigilant for behavioral changes suggestive of decompensation. With these steps and the assistance of a psychiatrist, most patients can do well and maintain an optimal level of function and quality of life.
1. Sajatovic M, Blow FC, Ignacio RV, Kales HC. Age-related modifiers of clinical presentation and health service use among veterans with bipolar disorder. Psychiatr Serv. 2004;55(9):1014-1021.
2. Sajatovic M, Strejilevich SA, Gildengers AG, et al. A report on older-age bipolar disorder from the International Society for Bipolar Disorders Task Force. Bipolar Disord. 2015;17(7):689-704.
3. Sajatovic M. Aging-related issues in bipolar disorder: a health services perspective. J Geriatr Psychiatry Neurol. 2002;15(3):128-133.
4. Fullerton CA, McGuire TG, Feng Z, Mor V, Grabowski DC. Trends in mental health admissions to nursing homes, 1999-2005. Psychiatr Serv. 2009;60(7):965-971.
5. Miller EA, Rosenheck RA. Risk of nursing home admission in association with mental illness nationally in the Department of Veterans Affairs. Med Care. 2006;44(4):343-351.
6. Tamashiro JH, Zung S, Zanetti MV, et al. Increased rates of white matter hyperintensities in late-onset bipolar disorder. Bipolar Disord. 2008;10(7):765-775.
7. Forester BP, Ajilore O, Spino C, Lehmann SW. Clinical characteristics of patients with late life bipolar disorder in the community: data from the NNDC registry. Am J Geriatr Psychiatry. 2015;23(9):977-984.
8. Sajatovic M, Chen P. Geriatric bipolar disorder. Psychiatr Clin North Am. 2011;34(2):319-333.
9. Kilbourne AM. Bipolar disorder in late life: future directions in efficacy and effectiveness research. Curr Psychiatry Rep. 2005;7(1):10-17.
10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Publishing, 2013.
11. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
12. Van Gerpen MW, Johnson JE, Winstead DK. Mania in the geriatric population: a review of the literature. Am J Geriatr Psychiatry. 1999;7(3):188-202.
13. Stewart JT. Behavioral and emotional complications of neurologic disorders. In: Noseworthy JH, ed. Neurological Therapeutics: Principles and Practice. 2nd ed. Abingdon, UK: Informa Healthcare; 2006:3207-3222.
14. Brenner I. Apathetic hyperthyroidism. J Clin Psychiatry. 1978;39(5):470-480.
15. Fietta P, Fietta P, Delsante G. Central nervous system effects of natural and synthetic glucocorticoids. Psychiatry Clin Neurosci. 2009;63(5):613-622.
16. Oostervink F, Boomsma MM, Nolen WA, EMBLEM Advisory Board. Bipolar disorder in the elderly: different effects of age and of age of onset. J Affect Disord. 2009;116(3):176-183.
17. Young RC, Jain H, Kiosses DN, Meyers BS. Antidepressant-associated mania in late life. Int J Geriatr Psychiatry. 2003;18(5):421-424.
18. Zimmerman M, Ruggero CJ, Chelminski I, Young D. Clinical characteristics of depressed outpatients previously overdiagnosed with bipolar disorder. Compr Psychiatry. 2010;51(2):99-105.
19. Butler C, Zeman AZJ. Neurological syndromes which can be mistaken for psychiatric conditions. J Neurol Neurosurg Psychiatry. 2005;76(suppl 1):i31-i38.
20. Stewart JT. Why don’t physicians consider depression in the elderly? Postgrad Med. 2004;115(6):57-59.
21. Depp CA, Jeste DV. Bipolar disorder in older adults: a critical review. Bipolar Disord. 2004;6(5):343-367.
22. Weintraub D, Lippmann S. Delirious mania in the elderly. Int J Geriatr Psychiatry. 2001;16(4):374-377.
23. Peters A, Sylvia LG, Magalhaes PV, et al. Age at onset, course of illness and response to psychotherapy in bipolar disorder: results from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Psychol Med. 2014;44(16):3455-3467.
24. Dell’Osso B, Buoli M, Riundi R, et al. Clinical characteristics and long-term response to mood stabilizers in patients with bipolar disorder and different age at onset. Neuropsychiatr Dis Treat. 2009;5:399-404.
25. Vasudev A, Thomas A. ‘Bipolar disorder’ in the elderly: what’s in a name? Maturitas. 2010;66(3):231-235.
26. Young RC, Mulsant BH, Sajatovic M, et al. GERI-BD: a randomized, double-blind controlled trial of lithium and divalproex in the treatment of mania in older patients with bipolar disorder. Paper presented at: American Association for Geriatric Psychiatry Annual Meeting; March 2012; San Antonio, TX.
27. Azab AN, Shnaider A, Osher Y, Wang D, Bersudsky Y, Belmaker RH. Lithium nephrotoxicity. Int J Bipolar Disord. 2015;3(1):28.
28. Aziz R, Lorberg B, Tampi RR. Treatment of late-life bipolar disorder. Am J Geriatr Pharmacother. 2006;4(4):347-364.
29. Post RM. Acquired lithium resistance revisited: discontinuation-induced refractoriness versus tolerance. J Affect Disord. 2012;140(1):6-13.
30. Murphy JV, Marquardt K. Asymptomatic hyperammonemia in patients receiving valproic acid. Arch Neurol. 1982;39(9):591-592.
31. Sajatovic M, Gyulai L, Calabrese JR, et al. Maintenance treatment outcomes in older patients with bipolar I disorder. Am J Geriatr Psychiatry. 2005;13(4):305-311.
32. Calabrese JR, Sullivan JR, Bowden CL, et al. Rash in multicenter trials of lamotrigine in mood disorders: clinical relevance and management. J Clin Psychiatry. 2002;63(11):1012-1019.
33. Beyer JL, Siegal A, Kennedy JS, et al. Olanzapine, divalproex, and placebo treatment non-head-to-head comparisons of older adult acute mania. Paper presented at: 10th International Psychogeriatric Association Annual Meeting; September 2001; Nice, France.
34. Sajatovic M, Dines P, Fuentes-Casiano E, et al. Asenapine in the treatment of older adults with bipolar disorder. Int J Geriatr Psychiatry. 2015;30(7):710-719.










