Aquatic Therapy and Alzheimer’s Disease
Key words:Aquatic therapy, Alzheimer’s disease, dementia, activities of daily living.
_______________________________________________________________________________________________________________________________
It is estimated that 5.2 million Americans have Alzheimer’s disease (AD), and one in three older adults dies with AD or another dementia.1 In the absence of a cure for AD, there are numerous physical and cognitive interventions that attempt to slow further cognitive decline and improve quality of life, particularly in achieving greater independence in activities of daily living (ADLs). Exercise therapy is one of these modalities that has shown the potential to improve physical and cognitive functioning in persons of all ages. To maintain health in older adults, the American College of Sports Medicine and the American Heart Association recommend a variety of land-based exercises that involve aerobic activity, muscular strengthening, flexibility, and balance2; however, nonambulatory patients with advanced AD are generally incapable of performing the same activities as their ambulatory peers. Therefore, it may be questionable whether land-based exercise could provide these nonambulatory patients with any measurable benefits.
The aquatic environment provides buoyancy, which confers an enhanced ability for nonambulatory patients to practice ambulatory and balancing skills. As a result, aquatic therapy (AT) has been used for a variety of neurological and musculoskeletal conditions, including balance disorders, post-stroke effects, Parkinson’s disease, total brain injuries, and lower extremity arthritis, but has not been used specifically for dementia. In this article, we present a case report of a nonambulatory patient with advanced AD who underwent AT using the Halliwick concept (Table 1).3-7 This form of AT was originally developed in the 1930s to help patients with physical disabilities to become independent in the water, and it is based on a 10-point program that focuses on skills such as mental adjustment, postural control, balance, ambulation in the water, and, ultimately, basic swimming movements.3 Our case report suggests that AT may possibly enhance the cognitive and motor skills in patients with advanced AD.

Case Report
Our case patient was an 89-year-old man with advanced AD who resided in a dementia unit for about 1 year. He had received a dementia diagnosis 5 years prior to being admitted to the dementia unit. His medical history included controlled hypertension, asymptomatic paroxysmal atrial fibrillation, treated dyslipidemia, and asymptomatic prostate cancer. His regular medications included aspirin, ramipril, amlodipine, hydrochlorothiazide, digoxin, simvastatin, donezepil, and memantine. Upon admission to the dementia unit, a cranial computed tomography scan showed no abnormalities except for periventricular age-related white matter changes. He was nonambulatory and incapable of any basic ADLs, except for the ability to self-feed.
Using the Minimum Data Set 3.0, we conducted an assessment of his cognition, mood, and functional status (Table 2).8,9 The findings of these assessments were consistent with a diagnosis of advanced dementia, and he remained poorly communicative and expressionless. After failing to progress after 6 weeks of conventional physical therapy, which included twice weekly sessions that consisted of range of motion exercises, balance training, and lower extremity strengthening exercises, AT was initiated twice weekly for 30 minutes over a period of 3 months. A baseline fall risk assessment,10 a Mini-Mental State Examination (MMSE), and an Apraxia Screen of TULIA11 were performed after 1 month of AT and followed serially over the next 2 months (Table 2). MMSE and AST testing were also administered on several occasions in the water by his aquatic therapist. His MMSE and AST scores were noticeably improved in the water, and his MMSE score on land improved from 2/30 at baseline to 4/30 at the follow-up evaluation after 3 months. The examiner noted that he was clearly more expressive and talkative than he was during his baseline MMSE examination.
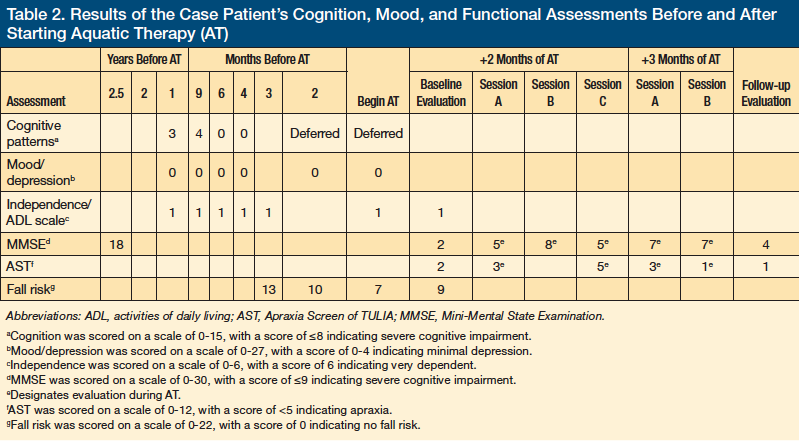
The objective evidence of improvement is limited by the floor effect of these scales since there is no good way to assess the degrees of advanced dementia. His fall risk scores also trended downward (Table 2). However, his fall risk was transiently higher for 2 to 3 hours after his AT sessions, when the staff noticed that he would attempt to stand from his wheelchair and walk on his own, not remembering that he needed help. They also noticed that for 2 to 3 hours after his AT sessions he was smiling more and talking more clearly without his usual trouble finding words. He even joked with the staff.
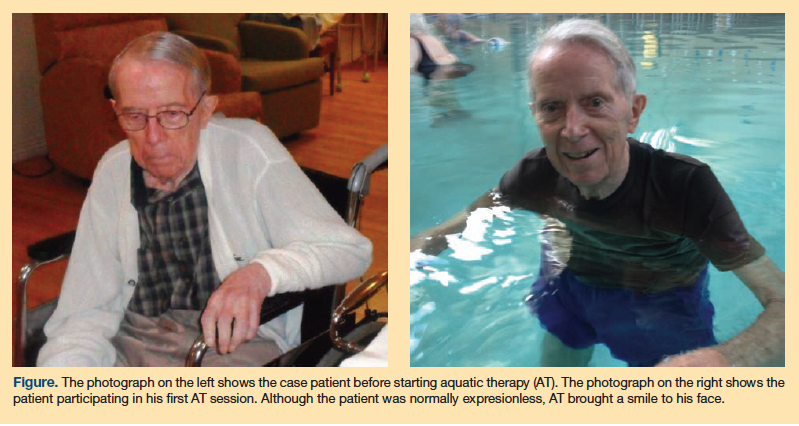
In addition, although the case patient was seated and submerged in warm water to his mid-abdomen twice weekly to be bathed, this had no noticeable effect on his cognition, expression, or communication skills; therefore, the mere act of being in the water did not improve his abilities. However, his very first AT session brought a broad smile to his normally expressionless face as he realized that he could ambulate in the water and perform AT rhythmic walking and positioning maneuvers (Figure).
The patient continued to perform AT exercises at increasingly advanced levels over the subsequent 3 months, and he eventually could obey a command to walk in the water to the edge of the pool, retrieve a pool toy, and bring it back to the aquatic therapist. His daughter visited him after 2 months of AT and she was also amazed when she got into the pool with him for a session. She stated, “In a way it was like having our dad back. It was amazing that he could communicate, speak in sentences, and follow directions. He really proved that he could understand.”
Discussion
Exercise has been shown to improve physical functioning in community-dwelling elders with AD12 and to slow the rate of decline in ADL performance in long-term care residents with dementia.13,14 What follows is a review of AT as an exercise program, including appropriate candidates for this therapy and a review of the benefits that have been observed.
Who is a Candidate for Aquatic Therapy?
Patients with decreased conditioning, cognitive impairments, reduced strength and endurance, head and spinal cord injuries, stroke, amputation, arthritis, osteoporosis, chronic back pain, and movement disorders may benefit from AT. Although this is a long list of candidates, there are also several patient groups in whom AT is contraindicated, including persons with aquaphobia and those with a fever or infection. Patients with cardiovascular diseases, particularly those with decompensated heart failure or a history of severe myocardial infarction, also are not candidates for AT.15 This is because immersion in the water may cause an abnormal cardiac response, especially when these patients are immersed up to their necks. In addition, persons with open wounds should not receive AT; however, patients with surgical wounds following total hip or knee replacement can become candidates for AT starting as early as postoperative day 4.16 Although incontinence has been considered a contraindication to AT, these patients may become candidates for this therapy if they are toileted before entering the pool and are provided with commercially available incontinence swim briefs.
Benefits of Aquatic Therapy
AT has been reported to have numerous benefits, but particularly in improving balance. What follows is a review of these benefits, including what several small studies have shown with regard to post-stroke rehabilitation, Parkinson’s disease, arthritis, and brain injuries.
Balance. Buoyancy in the water and the viscosity of water compared with air enable nonambulatory persons and those at high risk of falls to practice balancing skills while strengthening their lower extremity musculature without the risk of falling. In addition to the Halliwick concept, numerous other AT approaches have been used to improve balance, including water shiatsu (Watsu),4 water tai chi (Ai Chi),5 the Bad Ragaz ring method,6 and a task-type training approach7 (Table 1). Morris17 describes these approaches in detail in an article that outlines how AT improves balance dysfunction in older adults regardless of the physical problem causing the dysfunction, which can include musculoskeletal-related structural limitations, decreased sensory capabilities, motor coordination deficits, and loss of anticipatory control mechanisms.
In 1996, Simmons and Hansen18 conducted a study that included 52 healthy older adults assigned to one of four groups that met twice weekly for 45 minutes: water exercisers, who performed gait, balance, and lower body strengthening activities in the water; land exercisers, who performed comparable land-based exercises; water sitters, who sat in water while socializing; and land sitters, who sat on land while socializing. Each group had baseline functional reach test (FRT) scores of less than 10 inches, indicating a risk for falling. The groups were retested weekly during the 5-week study period. Only the water exercisers’ FRT scores improved weekly, with a final score of 13.4±1.6 inches. Land-based exercisers improved their scores only during the first week, with a final score of 11.3±1.5 inches. The nonexercising groups’ scores did not change. Based on their findings, the authors speculated that the freedom of moving freely in the water without the risk of falling enabled the water exercisers to improve their postural skills. They noted that elderly people might limit their movements because they fear falling, but that this can also contribute to falls by impeding their motor skills.18 This study implies that while gait, balance, and lower body strengthening activities reduce fall risk, aquatic exercises are more effective.
In 2008, Roller and colleauges19 found that an AT program consisting of active range of motion exercises, water walking, and using water weights for strengthening improved Berg Balance Scale (BBS) scores by 20% in 13 female assisted living residents (mean age, 77.5 years). The AT sessions were 45 minutes each and conducted twice weekly for a 6-week period. Although there was no comparison to a comparable land-based program, the AT participants had developed balance and stumble recovery skills in the water, which reduced their risk of falling and improved their BBS scores. The authors urged further research to assess whether a land-based exercise program could have the same effects.
In 2010, one such study was conducted by Brazilian researchers, who randomly assigned 36 elders to one of three groups: an aquatic exercise group, a nonaquatic exercise group, and a control group.20 All participants were evaluated at baseline and at 6 weeks using the BBS score and the Dynamic Gait Index, and their gait speed and tandem gait were also assessed. Both exercise groups underwent a program to improve lower-limb muscle endurance via 40-minute exercise sessions twice weekly for the study period. The researchers found that the muscle endurance programs provided a significant improvement in static and dynamic balance, regardless of environment (ie, aquatic versus nonaquatic); however, these participants had fewer limitations because they were cognitively intact community-dwelling elders. For long-term care residents with cognitive deficits, particularly those with severe dementia, land-based exercises may not be possible. Regardless, the study provides further evidence that water-based activities can improve balance.
A study by Gabilan and colleagues21 used AT based on the Halliwick concept and the Bad Ragaz ring method to provide vestibular rehabilitation to 21 patients with unilateral vestibular hypofunction due to multiple etiologies. AT was administered three times weekly for 45 minutes in 1.3 meters of water for 12 sessions. No other method of vestibular rehabilitation or therapeutic exercise was allowed and no association with the use of antivertigo medications and AT therapeutic effects was found. Compared with pretreatment results, all patients improved significantly when evaluated with the Brazilian Dizziness Handicap Inventory, dynamic computerized posturography, and the self-perception scale of dizziness intensity. The authors suggested that improvement resulted from recalibration of sensory inputs because the aquatic environment increases visual vestibular mismatch, decreases weight-bearing sensory information, and requires more controlled body translation. While this study was not limited to older adults, it suggests that AT might improve balance in people with vestibular disorders, the prevalence of which increases with age.
Post-Stroke. Several small-scale studies have shown water-based exercises to improve motor function in persons who have sustained a stroke. In 2004, Chu and colleagues22 randomly assigned 12 community-dwelling patients with mild to moderate residual motor defects following a stroke into an experimental group that exercised in chest-deep water and a control group that did arm and hand exercises while sitting on land. Both groups exercised for 1 hour three times a week for 8 weeks. Outcome measures included cardiovascular fitness (VO2 max), maximal workload, gait speed, BBS score, and overall muscular strength. The BBS improved slightly in both groups, with slightly more improvement in the control group, while the VO2 max improved by 22%, gait speed improved by 19%, and muscle strength on the more affected side improved by 9% in the experimental group. The improvement in muscle strength was deemed to be statistically significant, and the authors concluded “a water-based exercise program undertaken as a group program may be an effective way to promote fitness in people with stroke.”22
In 2007,a Brazilian study that evaluated a 12-week program of AT in 15 older adults who were recovering from a stroke found that these patients had a significant improvement in their ADLs compared with the control group of 13 patients.23 Based on their findings, the authors concluded that water-based exercises could improve the quality of life of stroke patients. In 2011, another small Brazilian studyevaluated 10 stroke patients between the ages of 7 and 83 years using a Timed Get Up and Go (TUG) test before and after each of the 12 water exercise sessions, which included stretching, muscle strengthening, balance training, and walking.24 The researchers found that participants’ TUG scores generally improved after each session, and all 10 participants improved their TUG scores at 12 weeks compared with their baseline scores.
In 2008, Korean researchers assessed whether AT could improve postural balance and muscle strength in stroke survivors.25 The study randomly assigned 25 ambulatory chronic stroke patients to an AT group (n=13) or to a conventional therapy group (n=12), both of which attended 1-hour sessions three times a week for 8 weeks. Persons receiving AT performed weight-bearing and balance exercises using the Ai Chi and Halliwick concepts, whereas the conventional therapy group performed gym exercises. Compared with the conventional therapy group, the AT group showed statistically significant improvements in BBS scores, forward and backward weight-bearing abilities of the affected limbs, and knee flexor strength.25
In 2011, Mehrholz and associates26 reviewed several databases to identify studies that examined whether AT could improve stroke outcomes. They included four randomized trials in their assessment, which collectively included 94 participants. Based on their review, the authors concluded that there is insufficient evidence to show water-based exercises after stroke to be effective in reducing disability, and they called for better and larger studies.26 Nevertheless, the authors found no reported adverse effects with AT in any of the studies, which indicates that AT may be safe to try in this population.
Other Potential Benefits of AT. In addition to helping with balance and stroke recovery, AT has been reported to help with numerous other conditions. One small Spanish study assessed whether AT could be beneficial for persons with Parkinson’s disease.27 The study randomly assigned 11 patients with Parkinson’s disease into land- and water-based physiotherapy groups. Both groups received comparable training to include warm-up exercises, trunk mobility exercises, postural stability training, and transfer training during individual 45-minute sessions twice weekly for 4 weeks. Baseline and post-intervention evaluations were performed 12 hours after Parkinson’s medications were withheld and included an FRT, BBS score, gait evaluation, TUG test, and Unified Parkinson’s Disease Rating Scale (UPDRS) score. Both groups improved with regard to the FRT. There was no significant difference in either group with respect to gait evaluation and the TUG test, and only the AT group improved with regard to their BBS and UPDRS scores.
In 2000, a small study showed AT to increase postural stability in women with lower extremity arthritis.28 In the study, 24 women with lower extremity arthritis were randomly assigned to an AT group (n=14) or to a control group (n=10). The researchers found that the AT participants had reduced their lateral sway and total sway scores by 18% and 30%, respectively. A more recent study from 2012 that compared aquatic treadmill exercise to land-based treadmill exercise noted a significant improvement in gait kinematics and 100% improvement in perceived pain in knee joint arthritis patients performing these exercises in water.29
AT has also demonstrated greater improvement than land-based physiotherapy following total hip or knee replacement starting as early as postoperative day 4,16 and a systematic review and meta-analysis in 2013 concluded that early AT following orthopedic surgery does not increase the risk of wound-related adverse events.30 In addition, spinal cord injury patients with spasticity improved significantly and required less medication (baclofen) after 10 weeks of AT and passive range of motion exercises compared with a control group treated only with medication and passive range of motion exercises.31 Another study documented reduced spasticity and a significantly decreased quantitative knee-jerk reflex, especially in an affected limb, following a 2-week course of AT in patients with spastic paresis resulting from hemiparesis, paraparesis, tetraparesis, or multiple sclerosis.32
Several small reports have shown AT to be beneficial for patients who have experienced a brain injury. In 2004, a randomized controlled trial that included 16 patients with brain injury and unilateral spasticity noted improvement in cardiovascular endurance, muscular strength and endurance, and flexibility after an 8-week course of AT three times weekly.33 More recently, a case report noted AT to be a useful adjunct to land-based physiotherapy to improve balance, gait, coordination, and ataxia in a patient with a traumatic brain injury.34
Conclusion
AT appears to be effective for a number of neurological and musculoskeletal disorders, and it may be more effective than land-based physiotherapy in some cases. The improvement in our case patient’s cognitive skills during AT sessions was especially impressive to his family members and to his caregivers, although the carryover effect on land after AT was limited. It is still unclear why AT is so beneficial, but there is speculation that the aquatic environment might recalibrate sensory inputs in cognitively impaired patients because water immersion decreases weight-bearing sensory information and requires less effort to balance, enabling enhanced focus on cognitive skills. Our case report illustrates a need to further study the potential for AT to improve the quality of life of patients with dementia.
References
1. Alzheimer’s Association. Alzheimer’s facts and figures. www.alz.org/alzheimers_disease_facts_and_figures.asp. Accessed April 15, 2013.
2. Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094-1105.
3. Lambeck J, Gamper U. The Halliwick Concept. In: Becker BA, Cole AJ, eds. Comprehensive Aquatic Therapy. 3rd ed. Pullman, WA: Washington State University Publishing; 2011.
4. Dull H. Watsu: Freeing the Body in Water. Middletown, CA: Harbin Springs Publishing; 1993.
5. Sova R, Konno J. Ai Chi: Balancing Harmony and Healing. Port Washington, WI: DSL Ltd; 1999.
6. Boyle AM. The Bad Ragaz ring method. Physiotherapy. 1981;67(9):265-268.
7. Morris DM. Aquatic rehabilitation for the treatment of neuromuscular disorders.
J Back Musculoskelet Rehabil. 1994;4(4):297-308.
8. Centers for Medicare & Medicaid Services. Long-Term Care Facility Resident
Assessment Instrument User’s Manual: MDS 3.0. V1.08. April 2012.
9. Katz S, Down TD, Cash HR, Grotz RC. Progress in the development of the index of ADL. Gerontologist. 1970;10(1):20-30.
10. HC – Fall Risk Assessment v1.4. Royal Oaks Health Care Center, November 2007.
11. Vanbellingen T, Kersten B, Van de Winckel A, et al. A new bedside test of gestures in stroke: the apraxia screen of TULIA (AST). J Neurol Neurosurg Psychiatry. 2011;82(4):389-392.
12. Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA. 2003;290(15):2015-2022.
13. Rolland Y, Pillard F, Klapouszczak A, et al. Exercise program for nursing home residents with Alzheimer’s disease: a 1-year randomized, controlled trial. J Am Geriatr Soc. 2007;55(2):158-165.
14. Roach KE, Tappn RM, Kirk-Sanchez N, Williams CL, Loewenstein D. A randomized controlled trial of an activity specific exercise program for individuals with Alzheimer disease in long-term care settings. J Geriatr Phys Ther. 2011;34(2):50-56.
15. Meyer K. Left ventricular dysfunction and chronic heart failure: should aqua therapy and swimming be allowed? Br J Sports Med. 2006;40(10):817-818.
16. Rahmann AE, Brauer SG, Nitz JC. A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: a randomized
controlled trial. Arch Phys Med Rehabil. 2009;90(5):745-755.
17. Morris D. Aquatic therapy to improve balance dysfunction in older adults. Top Geriatr Rehabil. 2010;26(2):104-119.
18. Simmons V, Hansen PD. Effectiveness of water exercise on postural mobility in the well elderly: an experimental study on balance enhancement. J Gerontol A Biol Sci Med Sci. 1996;51(5):M233-M238.
19. Roller J, Johnson M, Jones E, Hunt H, Kirkwood NW. Effectiveness of a water-based exercise program on Berg Balance Test scores in community-living older women.
J Aquat Phys Ther. 2008;16(1):1-5.
20. Avelar NC, Bastone AC, Alcântara MA, Gomes WF. Effectiveness of aquatic and non-aquatic lower limb muscle endurance training in the static and dynamic balance of elderly people. Rev Bras Fisioter. 2010;14(3):229-236.
21. Gabilan Y, Perracini M, Munhoz MS, Gananc FF. Aquatic physiotherapy for vestibular rehabilitation in patients with unilateral vestibular hypofunction: exploratory prospective study. J Vestib Res. 2008;18(2-3):139-146.
22. Chu K, Eng J, Dawson AS, Harris JE, Ozkaplan A, Gylfadottir S. Water-based exercise for cardiovascular fitness in people with chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2004;85(6):870-874.
23. Aidar F, Silva A, Reis VM, Carneiro A, Carnerio-Cotta S. A study on the quality of life in ischaemic vascular accidents and its relation to physical activity. Rev Neurol. 2007;45(9):518-522.
24. Goncalves dos Santos D, Pegoraro ASN, Vilela Abrantes C, Jakaitis F, Gusmen S, Bifulco SC. Evaluation of functional mobility of patients with stroke sequela after treatment in hydrotherapy pool using the Timed Up and Go Test. Einstein. 2011;9(3):302-306.
25. Noh DK, Lim JY, Shin HI, Paik NJ. The effect of aquatic therapy on postural balance and muscle strength in stroke survivors—a randomized controlled pilot trial. Clin Rehabil. 2008;22(10-11):966-976.
26. Mehrholz J, Kugler J, Pohl M. Water-based exercises for improving activities of daily living after stroke. Cochrane Database Syst Rev. 2011;(1):CD008186.
27. Vivas J, Arias P, Cudeiro J. Aquatic therapy versus conventional land-based therapy for Parkinson’s disease: an open label pilot study. Arch Phys Med Rehabil. 2011;92(8):1202-1210.
28. Suomi R, Koceja D. Postural sway characteristics in women with lower extremity arthritis before and after an aquatic exercise intervention. Arch Phys Med Rehabil. 2000;81(6):780-785.
29. Roper JA, Bressel E, Tillman MD. Acute aquatic treadmill exercise improves gait and pain in people with knee arthritis. Arch Phys Med Rehabil. 2012. Published online ahead of print November 3, 2012.
30. Villalta EM, Peiris CL. Early aquatic physical therapy improves function and does not increase risk of wound-related adverse events for adults after orthopedic surgery: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2013;94(1):138-148.
31. Kesiktas N, Paker N, Erdogan N, Gulsen G, Bicki D, Yilmaz H. The use of hydrotherapy for the management of spasticity. Neurorehabil Neural Repair. 2004;18(4):268-273.
32. Pagliaro P, Zamparo P. Quantitative evaluation of the stretch reflex before and after hydro kinesy therapy in patients affected by spastic paresis. J Electromyogr Kinesiol. 1999;9(2):141-148.
33. Driver S, O’connor J, Lox C, Rees K. Evaluation of an aquatics programme on fitness parameters of individuals with a brain injury. Brain Inj. 2004;18(9):847-859.
34. Degano AC, Geigle PR. Use of aquatic physical therapy in the treatment of balance and gait impairment following traumatic brain injury: a case report. J Aquat Phys Ther. 2009;17(1):16-21.
Disclosures:
The authors report no relevant financial relationships.
Address correspondence to:
Kent Myers, MD
Midwestern University
19555 N 59th Avenue
Glendale, AZ 85308
kmyers@midwestern.edu










