American Academy of Neurology (AAN) 2012 Annual Meeting
New Orleans, LA; April 21-28, 2012
______________________________________
Vitamin B12 Replacement Therapy Shows No Improvement for Patients With Dementia
Vitamin B12 replacement demonstrated no evidence of reversibility, stabilization, or retardation of dementia progression compared with Alzheimer’s disease, according to study results presented in an AAN poster session.
Routine practice to identify a reversible cause of dementia is done by determining vitamin B12 levels in patients with dementia. Conflicting evidence, however, exists regarding the effects of vitamin B12 replacement on dementia. The aim of this study was to assess the reversibility of dementia associated with vitamin B12 deficiency. Pavan Bhargava, MD, Southern Illinois University School of Medicine, and colleagues, reviewed the clinical course of patients who had presented to their dementia clinic and were found to have a vitamin B12 deficiency, defined as a low B12 level (<250 pg/mL) and elevated methylmalonic acid (>0.40 umol/L) or homocysteine (>15 umol/L) levels. The researchers also identified a comparison group of patients with probable Alzheimer’s disease, matched for age, sex, and baseline Mini-Mental State Examination (MMSE) score. Chi-square and the Mann-Whitney U tests were used for comparison of variables.
The investigators identified 33 patients with a vitamin B12 deficiency from a cohort of 1548 consecutive patients. Patients were treated parenterally with vitamin B12 and followed for a mean duration of 26.6 months. There was no considerable difference in baseline characteristics between the vitamin B12 deficiency group and the Alzheimer’s group except for initial vitamin B12 levels (153.3 ± 33.2 vs 518 ± 223.6, respectively). The findings indicated no difference in the rate of decline of the MMSE score between the vitamin B12 deficiency group and Alzheimer’s disease group (−0.19 ± 0.37 vs −0.12 ± 0.16, respectively; P=.45) and absolute change in MMSE score (−4.3 ± 4.8 vs −6 ± 7.8, respectively; P=.86). The results also showed no difference between the vitamin B12 group and Alzheimer’s group in the number whose MMSE scores were stable or improved at 12 months (−0.94 ± 3.78 vs −0.36 ± 3.40, respectively; P=.76) and 24 months (−1.46 ± 4.30 vs −0.27 ± 2.50, respectively; P=.53). None of the participants experienced a dramatic clinical reversal of their dementia with vitamin B12 replacement (30% for the vitamin B12 deficiency group and 27% for the Alzheimer’s group).
A study limitation acknowledged by the investigators was that the patients with vitamin B12 deficiency may also have had Alzheimer’s disease. The researchers concluded that considering the patient population, the dementia associated with vitamin B12 deficiency appears unlikely to reverse. They recommended additional studies to investigate the issue on a larger scale.
—Eileen Koutnik-Fotopoulos
(Continued on next page)
Patients With Dementia Benefit From Health Educator or Social Worker Counseling
Medication use is not the only treatment option for quality dementia care. A multidisciplinary approach is recommended to address the needs of patients and their caregivers. The contribution of health educators and social workers, who provide counseling services to patients and their families regarding dementia care, are underrecognized. Therefore, researchers sought to determine whether counseling by a health educator and/or social worker at the time of dementia diagnosis improves compliance with physician advice related to dementia care. Results of the study were presented in an AAN poster session.
For the study, 1577 patients with a cognitive symptom were seen in the Cognitive Disorders Clinic at the University of Utah between January 2006 and December 2010. All patients were referred to a health educator and to a social worker for education and planning upon receiving a dementia diagnosis. Edward Zamrini, MD, professor of neurology, University of Utah, and colleagues retrospectively determined how often a durable power of attorney (DPOA) for healthcare was present in the medical record and the enrollment level in the university’s Gift of Life (GTL) autopsy program.
The researchers noted that patients reflected the typical demographics of a dementia speciality clinic—682 (43.24%) were men, mean age was 72.8 years (range, 29-98 years), and Mini-Mental Health Status Exam (MMSE) or equivalent was 0-30 (mean, 22.08). Of the study participants, 1167 (74%) met with the health educator at least once, and 353 (22%) met with the social worker. The investigators performed four separate logistic regression models with DPOA or GTL enrollment as outcomes and health educator visit or social worker visit (yes/no) as predictors, and controlled for sex and dichotomized for age, years of education, symptom years, and MMSE, using cutoff point 70, 12, 2, and 24, respectively.
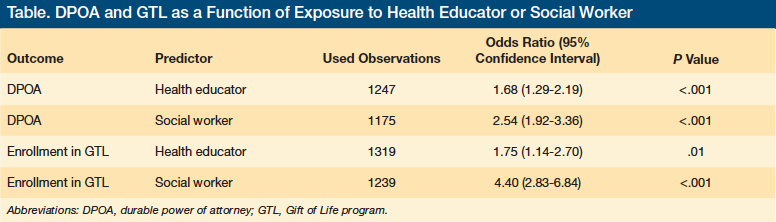
The findings showed that exposure to either a health educator or social worker correlated with DPOA documentation and enrollment in GTL (Table). The researchers concluded that health educator and/or social worker counseling “increases compliance with physician advice to complete a DPOA and to enroll in GTL.” They noted that additional studies are need to show that a health educator or social worker can improve quality of life and lower costs.—Eileen Koutnik-Fotopoulos
The study was funded by the University of Utah Center for Alzheimer’s Care, Imaging and Research, and the Center for Health Improvement.









