Administrator Turnover and Quality of Care in Nursing Homes
Many studies indicate that a shortage in manpower in long-term care facilities may adversely affect the quality of care given to elderly persons. Whereas previous studies focused on direct care workers, the authors assessed whether issues with management staff can also impact care quality. They gathered data every month for a period of 2 years from 151 nursing homes in Iowa to determine whether there was a statistically significant relationship between administrative turnover and the number of failures reported at the facilities. Bivariate correlation analyses and a linear regression model were used to examine the relationships, and other facility characteristics, such as the number of beds, ownership type, and facility location (rural vs urban setting) were used as control variables. Through their assessments, the authors found a statistically significant relationship between administrative turnover and the number of deficiencies reported at a facility, with more deficiencies being identified at facilities with a higher rate of turnover.
Key words: Survey failure, administrative turnover, facility size, facility location, quality of life, quality of care.
________________________________________________________________________________________________________________________________________________
Several reports have indicated that a workforce shortage is threatening the long-term care (LTC) industry.1-6 Most studies have examined how shortages of direct care staff, such as nurses and certified nursing assistants, affect care quality, but little attention has been paid to the professionals who supervise this staff.1,2 Nursing home administrators oversee the daily operations of LTC facilities and play an integral part in managing direct care staff. Quality of life for residents in nursing homes is related to care practices, which are implemented by direct care employees under the direction of administrators.3 Turnover of LTC workers has been an issue for some time, including with regard to management.4-6 The impact of this turnover on the provision of care has yet to be fully understood. In this article, we address the issue by investigating the relationship between administrator turnover and quality of care at LTC facilities in Iowa. What follows is a brief discussion of the methods and findings of our study and its implications for LTC facilities nationwide to show how this study contributes to the growing body of evidence examining the association between administrative leadership and care quality. This article also acknowledges several study limitations and gaps in the research, which future studies should address.
Methods
We used publicly available data from the Iowa Department of Inspections and Appeals (DIA), pulling administrative turnover data from its Health Facilities Division Website.7 The data were abstracted monthly from records that spanned a 2-year period from December 2004 to December 2006. Changes in the administrator ID filed (ie, administrator name) were monitored and tagged to determine turnover rates. The data on deficiencies were abstracted from report cards that were posted over a 17-month period from May 2005 to December 2006.
At the beginning of each month during the data collection period, the names and addresses of the current administrator, the state-provided ID of the nursing home, and several other variables about the facility were recorded and stored in a database. The “administrative turnover” variable was then derived from these records by flagging the event of turnover (ie, the event change and the date of change). The number of administrative turnovers was then counted and stored in an analytic file format. The bed-count variable for each facility was also obtained from the same registry database. The occurrence of a deficiency and the date at which the deficiency was recorded were captured from the facility report card that was published by the DIA. The DIA-provided facility IDs, which were available on both the registry data and the report card tables, were used to link or “merge” the two research data tables. Univariate, bivariate, and multivariate techniques were used to answer the research question.
Results
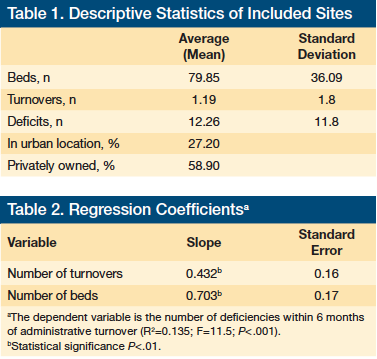
A total of 151 facilities were included in this study. The characteristics of these facilities, the average number of deficiencies, and the number of turnovers are outlined in Table 1. The Pearson’s correlation coefficients were calculated to evaluate the bivariate relationship between the research variables. Our analysis showed a weak but statistically significant correlation between the number of deficiencies (ie, dependent variable) and facility size, urban setting, and administrator turnover. It also showed a fairly moderate and statistically significant correlation between urban setting and facility size as measured by the number of beds.
A multivariate regression model was used to explore the statistical significance of the relationships between administrator turnover (the independent variable) and the number of deficiencies (the dependent variable), controlling for facility size. Originally, because in the bivariate analysis the relationship between the urban setting variable and the number of deficiencies was statistically significant, a dummy variable representing urban setting was included in the multivariate regression model; however, in this model, the relationship between urban setting and the number of deficiencies was not statistically significant. Hence this variable was removed from the multivariate model.
Table 2 shows the result of the regression analysis. The regression model was statistically significant, with an F-test of 11.5 (P<.001). Hence, there is a statistically significant relationship between the administrative turnover and the number of deficiencies when the effect of number of beds is held constant. The model accounted for about 13.5% of the variation in reported number of deficiencies. While this does not indicate a strong level of determination, the result of the F-test showed that this could not have been obtained by chance. Further, the slope parameters of the two predictor variables in the model (controlling for the other) were positive and statistically significant.
Study Limitations
Our study had several limitations. First, the administrative turnover data from the DIA spanned a 2-year period, whereas the data on deficiencies that were abstracted from report cards were from a 17-month period. Hence the data from the predictor variable used a wider observation window than the data from which the criterion variable was derived. Second, one of the facilities included in our study had more than 700 beds, whereas the rest had no more than 200 beds. This created the problem of departure from normality for the facility size variable. To address this, the outlier value was re-coded to 200, the next highest value in the dataset. Finally, the study was limited to nursing homes in Iowa.
Discussion
Administrators can have a significant impact on the quality of care at LTC facilities because these persons heavily influence overall facility operations. They manage the budget; implement and oversee staff training initiatives and secure the materials and resources for those initiatives; decide on care practices and oversee their implementation; address issues raised in meetings; communicate with staff; resolve facility and staff problems; and initiate quality assurance projects.3 In this section, we provide an overview of what the literature has shown with regard to administrator’s impact on care quality in LTC facilities and proceed to provide a recap of our study findings and observations.
Background
Several studies have linked care quality in nursing homes with administrator-related factors, including turnover, or have shown how facility factors can affect administrators both positively and negatively, thereby affecting turnover rates and care quality. Castle and colleagues3 noted that facility context (ie, facility size, ownership/chain membership, occupancy/Medicaid occupancy) and market context (competition and unemployment) impact consistency and coordination of care, with top management being influenced by these two contexts as they oversee care. Singh and associates6 hypothesized that administrator and facility characteristics could predict care quality. They found that demographics, qualifications, and professional status of the administrator in conjunction with the size, ownership, affiliation, location, and patient mix (ie, age, sex, race, and pay type) at the facility heavily influences care quality. Administrator stability and administrator effort also affected the quality of care. Understanding the context in which administrator turnover and caregiving takes place helps to further advance the knowledge of how to increase the tenure of nursing home administrators and ensure higher quality care for residents.
Deficiency citations from state surveyors are commonly used to measure the quality of care in LTC facilities. Federal and state regulations are enforced in an effort to maintain certain care standards. When these regulations are not met, the facility receives a deficiency citation. A 2006 study by Castle and Longest8 of approximately 17,000 LTC facilities showed an association between increased numbers of administrative deficiencies and increased numbers of care quality deficiencies. While a causal relationship could not be established due to the nature of these data, this association presents additional questions about the role administrator turnover may play in the number of deficiencies and quality of care. An earlier study by Castle9 reported a significant association between administrator turnover and various characteristics associated with care quality, including proportion of residents restrained, proportion of residents with pressure ulcers, and proportion of residents given psychoactive drugs.
One report found that increased length of employment significantly influenced quality in a positive way.10 This finding was supported by a study that found that facilities with three or more administrators during the study’s 42-month period had the highest number of health and safety deficiencies, whereas facilities with only one administrator during this time period had the lowest number of health and safety deficiencies.11
Studies indicate that administrator stability may relate directly to job satisfaction. In one study where administrators had an average tenure of only 31 months, administrator satisfaction was closely related to their interaction with coworkers.2 This indicates that increased satisfaction is an important strategy for lessening turnover. Another study suggested that reinventing the way administrators are trained, possibly by focusing on strengthening their competencies, may be another way to increase satisfaction.1 This finding was supported by a study that reported positive performance increased job satisfaction for administrators.6 It can be surmised that better training enables better performance, translating into increased job satisfaction. In contrast, a study by Myrtle and colleagues5 of healthcare managers found that no specific influence or group of influences could be used to determine commitment to career; however, when increased stability in the administrator position is achieved, it may lead to increased quality of care throughout the facility.
One conceptual model suggested that ownership of an LTC facility could influence administrator actions and the number of deficiencies.3 Ownership is frequently categorized as investor-owned, nonprofit, or public. One study of more than 13,600 LTC facilities found that even after multiple controls for location and reimbursement characteristics, investor-owned facilities averaged 0.679 more deficiencies than any other ownership type.12 This study suggests that ownership plays a significant role in the number of deficiencies and in the quality of care in LTC facilities.
Our Findings
Our study sought to further understand the relationship between administrator turnover and deficiencies reported to Iowa state surveyors. We found that a high rate of administrator turnover was associated with a high number of reported deficiencies in Iowa nursing homes. Other facility characteristics, such as size and location, also affected turnover, with larger facilities reporting an increased number of deficiencies as compared with smaller facilities. These larger nursing homes were located in more urban areas. This is most likely because more densely populated areas have a greater need for nursing home beds. Because larger facilities have a greater number of residents and workers, the finding that an increased number of beds is related to an increased number of deficiencies is fairly logical.
Urban areas also tend to have more facilities within close proximity to one another. We speculate this characteristic may promote administrator turnover in urban areas. When facilities are in close proximity to one another, administrators may be more inclined to leave a position when they become dissatisfied because they have a greater opportunity to find similar positions without having to relocate.
In our study, ownership of the facility was not found to be significant in determining the number of deficiencies. Due to the impact administrators have on managing direct care employees and on care practices, and the determination that reported deficiencies are an accepted way to monitor care quality, our findings support the hypothesis that administrator turnover does adversely affect care quality in LTC facilities.
These findings are in agreement with one previous research study in which administrator turnover was associated with an increased number of health and safety deficiencies.11 This correlation may be due to a multitude of factors, including the leadership role provided by the administrator. As with all occupations, a learning curve is present when new administrators start at a particular facility. Time is needed to understand the culture of the facility and the role that past leadership filled before any changes can be implemented. During this time of transition, direct care staff may become lax due to limited leadership and policy enforcement. Poor quality of care may itself lead to administrator turnover, which in turn leads to even poorer care quality, and the cycle continues, as was suggested by Castle and Lin,13 who reported a multicausal relationship between these two factors.
Nationwide implications and the need for future research. Given that our study is based on data from a single state, a legitimate question is how generalizable the results are to nursing homes in other states. Although the empirical model results pertain only to the conditions in Iowa, it is logical to extend the results to institutions in other parts of the country because US nursing homes share a number of common structural factors that shape their operations. For example, nursing homes in all states are subject to the standards set forth by the Nursing Home Reform Act, part of the
Omnibus Budget Reconciliation Act of 1987, which created a national set of standards of care for residents of certified nursing facilities.14 In addition, nursing homes nationwide face similar socioeconomic environments and market forces, and they have similar staffing characteristics, with direct care and indirect care staff having similar responsibilities. Based on these similarities, one can surmise that the relationship between administrative turnover and the quality of care may demonstrate parallel results in other states.
Future studies are needed to empirically examine the relationships between administrative turnover and nursing home care quality at a national level, and to understand the causes behind administrator turnover. Conceptual models may assist with determining more characteristics to consider.10,13 Implementing retention strategies could help secure administrators for longer tenure (eg, tenure-graded benefits packages). If the administrator is not performing effectively though, turnover may be beneficial.6 In any case, determining what personal and facility characteristics create the most job satisfaction for administrators is important to improving the quality of care at LTC facilities nationwide.
Conclusion
We found that the level of care quality at LTC facilities can be predicted by turnover, and that administrative turnover is also more predictive of care quality than structural characteristics, such as facility size and location. Based on our findings, it appears that prior studies that focused exclusively on direct care staffing characteristics have been missing an important piece of the puzzle: administrators. These individuals clearly have a tremendous impact on the quality of care at LTC facilities. We encourage future researchers to include administrative turnover when they model the structural determinants of nursing home quality. Obviously, our model does not tell the whole story, as it explains only a small proportion of the variations in quality. It does, however, make the important point that models that try to explain the variations in quality should include both direct and indirect care staffing characteristics of a facility. In addition, further research is needed to understand the causes behind administrator turnover.
References
1. Harahan MF. A critical look at the looming long-term-care workforce crisis. Generations. 2011;34(4):20-26.
2. Murphy B. Nursing home administrators’ level of job satisfaction. J Healthc Manag. 2004;49(5):336-345.
3. Castle NG, Ferguson JC, Hughes K. Humanism in nursing homes: the impact of top management. J Health Hum Serv Adm. 2009;31(4):483-516.
4. Kapp MB. Resident safety and medical errors in nursing homes: reporting and disclosure in a culture of mutual distrust. J Leg Med. 2003;24(1):51-76.
5. Myrtle RC, Chen DR, Lui C, Fahey D. Influences on the career commitment of health-care managers. Health Serv Manage Res. 2008;21(4):262-275.
6. Singh DA, Schwab RC. Predicting turnover and retention in nursing home administrators: management and policy implications. Gerontologist. 2000;40(3):310-319.
7. Iowa Department of Inspection and Appeals. Health Facilities Division. www.state.ia.us/government/dia/page11.html. Accessed January 7, 2013.
8. Castle NG, Longest BB. Administrative deficiency citations and quality of care in nursing homes. Health Serv Manage Res. 2006;19(3):144-152.
9. Castle NG. Administrative turnover and quality of care in nursing homes. Gerontologist. 2001;41(6):757-767.
10. Singh DA, Amidon RL, Shi L, Samuels ME. Predictors of quality care in nursing facilities. J Long Term Care Adm. 1996;24(3):22-26.
11. Christensen C, Beaver S. Correlation between administrator turnover and survey
results. J Long Term Care Adm. 1996;24(2):4-7.
12. Harrington C, Woolhandler S, Mullan J, Carrilo H, Himmelstein DU. Does investor ownership of nursing homes compromise the quality of care? Am J Public Health. 2001;91(9):1452-1455.
13. Castle NG, Lin M. Top management turnover and quality in nursing homes. Health Care Manage Rev. 2010;35(2):161-174.
14. Hawes C, Mor V, Phillips CD, et al. The OBRA-87 nursing home regulations and implementation of the Resident Assessment Instrument: effects on process quality. J Am Geriatr Soc. 1997;45(8):977-985.
Disclosures:
The authors report no relevant financial relationships.
Address correspondence to:
Simon Geletta, PhD
Department of Public Health
Des Moines University
3200 Grand Ave
Des Moines, IA 50312
sgeletta@dmu.edu










