What Do Our Seniors Need?Outcomes Of At-Home Comprehensive Geriatric Assessments
INTRODUCTION
Nevada continues to lead nationwide with the fastest growing age 65-and-over population. The number of seniors residing in Nevada increased by 72% between 1990 and 2000, and this population is estimated to grow another 20% between 2000 and 2004.1 Between the aging population and migration of older seniors, the rates of disability are increasing significantly. Disability, though not caused directly by age alone, increases in frequency with age. In 2003, 39% of the age 65-and-over population in Nevada reported a chronic condition that limited function. 8% of these seniors stated that their disability limited the performance of daily activities in a major way.2 The age 85-and-over age group, the fasting growing segment in Nevada, experiences an even higher prevalence of disability, with 64% reporting the presence of a disability.1 If one includes multiple morbidities, which occur in over three-quarters of the age 70-and-over population, the numbers of vulnerable elders in Nevada reaches into the tens of thousands, and continues to grow at an alarming rate.
From a financial perspective, Hoffman and Rice3 have estimated the costs associated with chronic illness and disability to our healthcare system. For every $1.00 spent on acute care services, a person with one chronic condition spends an additional $2.00, and a person with two or more chronic conditions spends an additional $6.00 for every acute dollar expended. These costs are significant, and generally not covered by the current healthcare system.
The early identification and care management of disabled, frail elderly persons is being addressed by Nevada’s Sanford Center for Aging and Office of Geriatric Medicine, Chronic Illness and Disability Management through a statewide Geriatric Resource Team (GRT). The GRT provides screening, assessment, service procurement, and monitoring to a targeted population of disabled elderly persons within their home setting. The objective is to maintain the individual’s independence and reduce institutionalization within acute and long-term care facilities. The GRT works closely with clients and families/caregivers to help with their short- and long-term goals. This plan of care, known as the Medical Action Plan (MAP), provides an added resource to the primary care physician and other healthcare providers involved in the clients’ care.
The GRT targets those disabled elderly persons, and directs them and their caregivers to the most appropriate and cost-effective care in the community. Within the state of Nevada, a connection between acute/chronic medical care and community services for an at-risk elder population has not existed prior to implementation of the statewide GRT.
To the authors’ knowledge, this program is one of a kind, given that it has been totally funded through a portion of the state of Nevada’s share of the national Master Settlement Agreement with the tobacco industry. The Fund for a Healthy Nevada was created in 1999 under NRS 439.605, and holds statutory authority to allocate these funds and to develop policies and procedures for the administration and distribution of grants targeting tobacco control, children’s health, and disability services. The statewide Geriatric Resource Team has received funding through a competitive application process since 1999.
METHODOLOGY
Referrals to the GRT are received from family members, provider offices, home health agencies, community programs, and individual clients themselves. This is accomplished by the completion of the Vulnerable Elders Survey (VES-13).4 The VES-13 is an easy-to-complete function-based tool for the screening of a community-dwelling population at risk for health deterioration. Clients can complete the VES-13 themselves, or health professionals may complete the VES-13 with the client. Often, a client will complete the VES-13 with a home health nurse during a routine home visit. A score of 3 or higher is used for determination of eligibility to the GRT program. Once a client is determined to be eligible by the GRT staff, a local area provider is assigned to the client. A nurse then visits the client’s home and completes a clinical assessment using a format previously developed under the Second Generation Social HMO Demonstration Program.5
The 20-page assessment has more than 300 questions and includes medical, psychological, functional, social, home safety, and medication reviews. Completion of the assessment in the client’s home takes 2-3 hours. A MAP is developed with input from the client, family members, and/or caregiver, when appropriate. After development of the MAP, the nurse care manager provides direction on how to access community services and implement the plan of care that has been agreed to by all parties. A copy of the MAP is provided to the primary care physician, with a follow-up conversation as needed. In order to assist in implementation, an additional 1-3 telephone contacts by the nurse care manager are provided to the client.
A follow-up telephone call at 6 months after development of the MAP is completed with the use of a detailed evaluation tool. A member of the GRT program uses a script to interview clients and caregivers. If a client does not answer the phone or respond to three messages, the questions are sent to the home of the client with a self-addressed, stamped envelope for return. This is performed in order to determine current living status, satisfaction with the GRT program, and client follow-through on the specific recommendations within the MAP.
RESULTS
The demographics of 233 clients served by the statewide GRT program are not different from the general population, as represented by the Nevada age 65-and-over data. Statewide in the Nevada age 65-and-over age group there are 47% males and 53% females in comparison to 34% males and 66% females in the GRT population served. The percentages of GRT clients according to where they live are: rural, 5%; Reno/Sparks/Carson City, 11%; and Las Vegas metropolitan area, 84%, which is proportional to the state demographics.
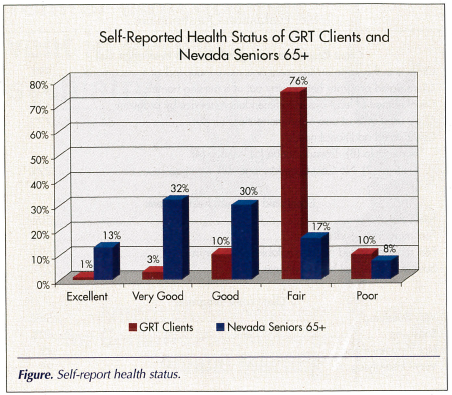
Within the area of self-reported health, more GRT clients expressed “Fair” or “Poor” health compared to the statewide statistics for the age 65-and-over population (Figure).The role of self-reported health status has been previously recognized as a valid indicator of current and future healthcare outcomes.6,7 This suggests that the screening for eligibility, provision of assessments, and a plan of care was being directed at the intended treatment population.
The recommendations by the GRT were incorporated into three main categories. This included Social Services (52%; eg, Senior/Health and Wellness Centers, Homemaker Programs, Lifeline/Safe Return, Meals on Wheels); Medical (20%; eg, See Doctor, Medication Review, Home Health Care, Medical Equipment/Products); and Lifestyle/Education (28%; eg, Smoking/Alcohol/Drug Cessation, Fall Prevention, Modify Diet, Exercise).
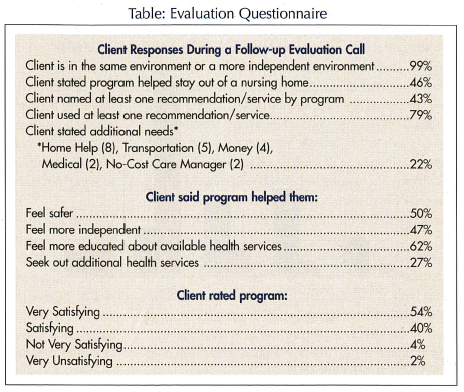
At the 6-month follow-up period, 137 clients were contacted and asked a standard series of “yes/no” questions regarding current living environment, implementation of GRT recommendations, how the program assisted them, and their overall level of satisfaction. The responses were favorable in the areas of continued independence, implementation of recommendations, safety, knowledge, and overall satisfaction (Table). The authors were unable to follow up with 96 clients as they did not return calls (55), were cognitively unable (6), refused to participate in the follow-up survey (10), or were not contacted due to completion of the program (25). Clients who returned calls were on average slightly older (78) and more likely to live in the Reno/Sparks/Carson City area (22%) or in rural regions (15%) as compared to the overall GRT population. In addition, respondents were more likely to report poor health (16% vs 10%) but less likely to report fair health (52% vs 75%).
DISCUSSION
The statewide GRT has provided a service to a segment of the elderly population within the state of Nevada that were identified with the use of a validated and reliable screening tool, the VES-13. Through the use of a standardized assessment tool, a plan of care was developed with overall client satisfaction and ability to remain within their same or more independent living environment. The authors are unaware of the VES-13 being used previously at a statewide level. In addition, the assessment tool was adapted from that used within the Medicare managed care arena for use in a non-managed care environment. The authors believe that this is noteworthy, given the limitation of resources available to the GRT as compared with a Medicare managed care program.
Limitations to this clinical investigation include the lack of a control group, the short duration of follow-up at 6 months, and limited ability to follow up with clients who have impaired memory and functioning. The VES-13 is intended to identify a group that at 2 years will require a higher level of care and or will have died. The authors believe that over time, their initial assessments and ongoing care management will address the impact of the GRT on this population. The authors are requesting additional support from the state of Nevada to expand the GRT operation, and enhance the role of nurse care management and the use of nurse practitioners and geriatricians in the assessment and management of this population. The long-term goal is to develop a program that will be able to sustain itself without state funding, based upon a successful model currently utilized in Nevada for the care of at-risk Senior Dimension Medicare Advantage members.8
CONCLUSION
More than 90 % of the clients who responded were satisfied or very satisfied with assessment and recommendations. Nearly 80% of clients enacted at least one of the recommendations provided by the Medical Action Plan, including medical care, social services, and increased health and wellness.
The Geriatric Resource Team increased a sense of safety, independence, and education in close to one-half of the clients. Nearly one-third of the clients sought out additional healthcare services after completion of the home assessment and development of the plan of care.
It appears that the statewide GRT is a valuable resource for this at-risk elderly population. Further evaluation and incorporation of greater care management with the involvement of advanced practitioners of nursing and geriatricians is warranted.
Acknowledgments
The authors would like to thank Linsay Oakden, BA, for her assistance with data collection and manuscript preparation, and Rickard Nilsson, BS, for his data analysis.
The statewide Geriatric Resource Team is funded by the Task Force for the Fund for a Healthy Nevada. The funding agency had no role in the program development, data collection, or preparation of the manuscript for publication.
Ms. Rogerson claims no conflict of interest; she participated in data collection, analysis, and manuscript preparation. Dr. Weiss claims no conflict of interest; he participated in program design, data analysis, and manuscript preparation. Dr. Phillips claims no conflict of interest; he participated in program design and implementation, data analysis, and manuscript preparation.









