SNF Success Under the New Hospital Readmission Payments
As promised, the federal government has moved to value-based reimbursement for skilled nursing facilities (SNFs) through financial adjustments based on hospital readmission rates that occur within 30 days of their discharge.1 Hospitalizations of nursing home (NH) residents, while decreasing in recent years, remain a problem, with nearly 11% of patients in 2016 being sent to hospitals for conditions that might have been averted with better medical oversight.2
Incentives to Drive Improved Outcomes
Congress created the Skilled Nursing Facility Value-Based Purchasing Program incentives in the 2014 Protecting Access to Medicare Act.1 In assigning bonuses and penalties, Medicare judged each facility’s performances in two ways: how its hospitalization rates in calendar year 2017 compared with other facilities and how much those rates changed from calendar year 2015.
SNFs received scores of 0 to 100 for their performances and 0 to 90 for their improvements, and the higher of the two scores was used to determine their overall score. Facilities were then ranked highest to lowest. Medicare is only measuring readmission rates of patients who are insured through traditional Medicare and not those enrolled in private Medicare Advantage (MA) plans, even though in some regions the majority of Medicare beneficiaries are members of MA plans. These MA plans are growing significantly in part because of their ability to offer benefits beyond traditional Medicare, making them especially attractive to younger Medicare beneficiaries who are typically coming from similar commercial plans.3
In early January 2018, the Centers for Medicare & Medicaid Services (CMS) announced that 10,976 NHs would have their Medicare reimbursement reduced for a year while 3983 facilities would receive bonus payments.2 These financial incentives, determined by each home’s readmission rates, significantly expand Medicare’s effort to pay medical providers based on the quality of care instead of just the number or condition of their patients.
Over this fiscal year, which began October 1, 2018, and goes through the end of September 2019, the best-performing homes will receive 1.6% more for each Medicare patient than they would have otherwise; the worst-performing homes will lose nearly 2% of each payment.4 The others will fall in between. A Kaiser Health News analysis of the data found that, in Arkansas, Louisiana, and Mississippi, 85% of homes will lose money.5 More than half in Alaska, Hawaii, and Washington will get bonuses. In general, for-profit NHs, which make up two-thirds of the nation’s facilities, face deeper cuts on average than do nonprofit and government-owned homes.5
Through the incentives, Medicare will redistribute $316 million from poorer-performing to better-performing NHs, while Medicare expects it will keep another $211 million that it would have otherwise paid to NHs if the program did not exist. As a result, Medicare will save money and drive behavior to improve clinical and financial outcomes as well.2
One NH group with 15 homes, for which Medicare is lowering payments to 12, anticipates losing almost $100,000, despite the fact that most of their hospital readmissions occurred after the patient left their SNF and was at home.2 Thus, the 30-day hospital readmission rate means that, for most patients, the SNF will be responsible for patients outside of their facility, as the average length of stay in SNFs is well below 30 days.
Enhanced Focus on Care Transitions
SNFs need to care for their patients not only in their SNF but also through the transition of care and into their homes in the community. For success during the SNF stay, this begins with working more closely with area hospitals to ensure that patients transferring to the SNF are clinically stable. But facilities should take care in these situations, as hospitals are increasingly looking to decrease their length of stay but do not want to suffer a readmission penalty. Once in the SNF, facilities will need to increase care access and level of their primary care provider (PCP) services through use of a dedicated SNFist, nurse practitioners, and virtual after-hours PCP services. Some facilities are going even further through use of paramedics or emergency services to provide rapid assessment and initial treatments so patients can be managed in the SNF, avoiding a hospital admission.
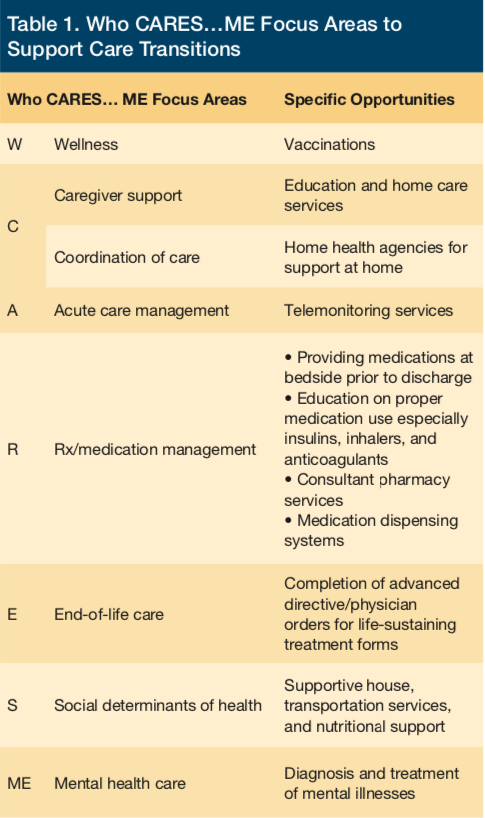
Prior to patient discharge and transition to the community, SNFs need to carefully consider whether patients are ready for discharge to the community; SNFs should focus on several areas best illustrated through the acronym “Who CARES…ME,” which targets several areas that help support successful transitions. These include: Wellness, Caregiver support, Coordination of care, Acute care management, Rx/medication management, End-of-life care, Social determinants of health, and Mental health care (Table 1).
These efforts are critical even beyond the context of CMS hospital readmission penalties as hospitals are defining their preferred SNF networks based on this data. As a result, not only will better performing SNFs receive additional funding directly from CMS, but these same facilities will likely received additional volume of patients from hospitals as well, as these hospitals look to improve their own readmission rates.
Conclusion
There are of course concerns with this program, for example, some consumer advocates fear that NHs will be reluctant to admit very infirm residents or to rehospitalize patients even when they need medical care. Also, since poor-performing facilities will see both direct CMS payment reductions and decreased volume from hospitals, there is a concern that this will cause a death spiral for these facilities as they will not have the funds needed to make improvements to improve their performance. For those involved in SNF care, assuring top performance will continue to be the best way to assure successful operation and what better way with answering the question, Who CARES? ME.
References
1. Centers for Medicare & Medicaid Services (CMS). The skilled nursing facility value-based purchasing program (SNF VBP). cms.gov website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Other-VBPs/SNF-VBP.html. Updated October 25, 2018. Accessed December 19, 2018.
2. Rau J. Medicare cuts payments to nursing homes whose patients keep ending up in hospital. Kaiser Health News. December 3, 2018. https://khn.org/news/medicare-cuts-payments-to-nursing-homes-whose-patients-keep-ending-up-in-hospital/. Accessed December 19, 2018.
3. Patel YM, Guterman S. The evolution of private plans in Medicare [issue brief]. Princeton, NJ: The Commonwealth Fund; 2017.
4. Look-up: Medicare’s bonuses and penalties for nursing homes near you. Kaiser Health News. November 30, 2018. https://khn.org/news/look-up-medicares-bonuses-and-penalties-for-nursing-homes-near-you/. Accessed December 19, 2018.
5. Centers for Medicare & Medicaid Services. SNF VBP facility-level dataset. data.medicare.gov website. https://data.medicare.gov/Nursing-Home-Compare/SNF-VBP-Facility-Level-Dataset/284v-j9fz. Accessed December 19, 2018.










