Pharmacologic Treatment of Sexual Inappropriateness in Long-Term Care Residents with Dementia
Although behavioral symptoms associated with dementia in geriatric long-term care (LTC) residents living in nursing facilities are common, sexual inappropriateness (sexual disinhibition) remains one of the least understood and treatable aspects of this disease. Separating agitation and normal sexual expression from any sexual disinhibition that may be present can be clinically challenging to the health care practitioner and LTC nursing staff. Family concerns and staff attitudes toward normal sexual expression between older adults living in a LTC nursing facility may also cause an inconsistent approach to the evaluation of sexual disinhibition.
REVIEW OF THE LITERATURE
It has been estimated that up to 90% of individuals with dementia will develop behavioral issues that are significant at some point along the course of their illness.1 Merriam et al2 have declared Alzheimer’s disease to be “the most widely encountered cause of psychiatric pathology associated with a specific neuropathologic substrate.” ________________________________________________________________________________________________________________________________________________
Related Content
Inappropriate Sexual Behavior in Long-Term Care
Medroxyprogesterone Acetate Treatment for Sexually Inappropriate Behavior in a Patient With Frontotemporal Dementia
_______________________________________________________________________________________________________________________________________________
The prevalence of dementia rises from approximately 5% in individuals ages 65-69 to 20% in those older than age 85.3 However, there is a paucity of research about the effects and management of cognitive impairments on sexuality in the older adult with dementia.
Sexual disinhibition may be regarded as sexually inappropriate or “acting out” behavior. Impulsive behavior and poor judgment often occur in dementia, and inappropriate sexual impulses that were once controlled by intact judgment or moral values may emerge. Such behaviors have been reported more commonly in men.4 As many as 7-25% of seriously cognitively impaired older adults are reported to display sexually inappropriate behaviors.5-7 Some examples include genital exposure, public masturbation, propositions to others for sexual intercourse, and attempts at coitus or fondling another person’s genitals or breasts.8 Additionally, sexual talk or sexual acts (such as openly reading pornographic material or requesting unnecessary genital care from staff members) may also occur.7 These behaviors can be disruptive and problematic for caregivers either in the community or in the LTC setting.
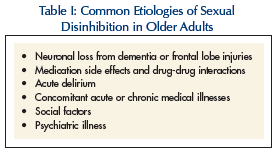 Causes of sexual disinhibition in the older individual are often multiple and include neurologic, psychiatric and social/environmental factors.9 Possible etiologic factors contributing to sexual disinhibition in the older adult are outlined in Table I. In individuals affected with Alzheimer’s disease, sexual disinhibition positively correlates with the clinical severity of dementia.5 However, this does not correlate with neuroimaging (CT scan) results. Frontal lobe injury is also known to be linked to sexual disinhibition, since inhibitory mechanisms that promote sexual self-control are impaired in these types of lesions.10 Subtypes of dementia that are frontal lobe-preponderant, including Pick’s disease and alcoholic dementia, may also be associated with sexually inappropriate behavior.
Causes of sexual disinhibition in the older individual are often multiple and include neurologic, psychiatric and social/environmental factors.9 Possible etiologic factors contributing to sexual disinhibition in the older adult are outlined in Table I. In individuals affected with Alzheimer’s disease, sexual disinhibition positively correlates with the clinical severity of dementia.5 However, this does not correlate with neuroimaging (CT scan) results. Frontal lobe injury is also known to be linked to sexual disinhibition, since inhibitory mechanisms that promote sexual self-control are impaired in these types of lesions.10 Subtypes of dementia that are frontal lobe-preponderant, including Pick’s disease and alcoholic dementia, may also be associated with sexually inappropriate behavior.
Reports have linked levodopa administration to hypersexuality when used in persons with Parkinson’s disease,11 and patients with brain damage have also been found to be more susceptible to the paradoxically disinhibiting effects of alcohol or benzodiazepines.12 Naguib and Levy13 examined the role of delirium in precipitating sexually inappropriate behaviors. In some cases, patients who have successfully controlled their heightened sexual impulsivity over a lifetime may regress after an episode of cognitive decline, such as that associated with an acute delirium. A stroke, cardiac event, vascular compromise, or surgery may also subsequently lead to sexual disinhibition.14 In such instances, sexual aggression is usually noted to be of an acute onset.
Social factors that bear mentioning include privacy constraints in nursing facilities that can lead to sexually inappropriate behavior in public areas of the facility and social cues, such as explicit television shows, which may also precipitate sexual disinhibition. Actions of caregivers can be misinterpreted—for example, an older male patient may misconstrue the hygiene care provided by female nursing staff as a sexual act or romantic advance.15 Additionally, manifestations of psychosis or mania occurring in dementia can lead to sexual inappropriateness.16 Although female residents may also develop sexual disinhibition, most of the literature reviews male interactions with other individuals.
Continued on next page
ASSESSMENT AND MEDICATION INTERVENTIONS FOR SEXUAL DISINHIBITION
Assessment
The cardinal step in assessing sexual inappropriateness in a LTC resident with dementia is obtaining a thorough history. Whenever possible, this should be from the resident as well as any of their caregivers.10 Psychosexual assessments and sexual history taking should ideally be included in the initial interview at the time of admission. “Aberrant” sexual behavior that is representative of a life-long pattern of very active sexual activity should be differentiated from disinhibition due to impaired judgment and impulse control from underlying medical conditions. Any evaluation of recent-onset cognitive impairment should also address the risk for sexually aggressive or inappropriate behavior in that individual. A mental status examination and physical examination, when pertinent, should be included in the assessment to rule out delirium or other acute or chronic medical illnesses as the cause of the sexual disinhibition. Formal mental status tests including the Folstein Mini-Mental State Examination17 and the Clock-Drawing Test18 may also be obtained. Yields from these tests may necessitate referral to a neuropsychologist for a more specific diagnosis, as well as recommendations for approaching other types of behavioral disturbances. Laboratory tests may further aid in evaluating the role of underlying medical conditions contributing to inappropriate sexual behavior.
Staff should avoid misinterpreting nonsexual behavior, such as confused wandering into another resident’s bedroom, as representing sexual disinhibition. Inappropriate sexual acts within a nursing facility tend to be remembered for a long time by staff and family members. There is often a tendency to label a resident as having “sexual inappropriateness” on the basis of a few instances.10 Therefore, accurate nursing notes and problem behavior checklists can aid in identifying any possible precipitants and decrease the risk of inaccurate identification of sexual impropriety.
It is critical to address ethical dilemmas and value judgments inherent with assessing and treating these issues. For example, before identifying and treating sexually inappropriate behavior, it should be ascertained whether the behavior in question is truly “inappropriate” or whether it is based on a judgment relative to a staff member’s own personal moral or ethical values.19 It is helpful to monitor the frequency and severity of any identified behaviors, and open communication in the interdisciplinary team meeting is recommended to explore these issues. In a study by Pease,20 this format enabled the treatment team to acknowledge the occurrence of sexual incidents and to offer support to the staff members directly involved.
Pharmacologic Interventions
 A review of the literature indicates that there have been few randomized controlled trials regarding the use of medications to address sexual disinhibition in the older adult with dementia.21 Pharmacologic management has included the use of hormonal agents or various psychotropic medications. Table II lists the medications that have been studied for treatment of sexual disinhibition.
A review of the literature indicates that there have been few randomized controlled trials regarding the use of medications to address sexual disinhibition in the older adult with dementia.21 Pharmacologic management has included the use of hormonal agents or various psychotropic medications. Table II lists the medications that have been studied for treatment of sexual disinhibition.
Antiandrogens. These agents exert their clinical effect by reducing serum testosterone levels leading to impaired sexual functioning, subsequently reducing inappropriate sexual behaviors. Medroxyprogesterone acetate (MPA) is a type of progesterone that decreases testosterone by inhibiting pituitary luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
The main side effects of MPA that have been reported include sedation, weight gain, fatigue, hot and cold flashes, mild diabetes, depression, and loss of body hair. In a case series by Cooper,22 four male nursing home residents with dementia and inappropriate sexual behaviors (masturbation, fondling, exposure, and attempting intercourse with other residents) were followed. The residents were between the ages of 75 and 84 and had failed behavioral management and treatment with chlorpromazine and thioridazine. The intramuscular administration of MPA at 300 mg weekly for 1 year was completed, and sexual inappropriateness was charted 6 months before the trial, during treatment, and for 1 year after the trial. Undesirable sexual behaviors were reduced within 10-14 days following the initiation of MPA treatment. Levels of testosterone and LH (which had fallen during the course of treatment) returned to pretreatment levels within 4 weeks after the trial ended. At the 1-year follow-up point, three out of the four residents were deemed to be free of sexually inappropriate behaviors. The fourth resident had a return of some behaviors, but to a lesser degree when compared to treatment.
Weiner et al23 reported two cases of sexual disinhibition (exposure, masturbation, fondling, and molestation) in men with dementia aged 72 and 84 years. Both of these residents had failed a trial of thioridazine. Intramuscular MPA at doses of 150 mg and 200 mg, respectively, led to a reduction of the inappropriate sexual behaviors within a 2-week period.
Cyproterone acetate (CPA) is another potent progesterone that suppresses end organ androgen influence, even when androgen levels are not elevated. Adverse effects of CPA include hepatic dysfunction, fatigue, gynecomastia, depression, and weight gain. There are no case reports documenting the use of antiandrogens in older women with dementia, but CPA has been used successfully in younger women. Nadal and Allgulander24 documented a report of successful treatment of hypersexuality in a 49-year-old female with suspected frontotemporal dementia of Pick’s type who presented with unrestrained masturbation. This patient had failed a trial of antidepressants and neuroleptics. Administration of CPA was started at 50 mg daily and increased to 100 mg daily as tolerated 3 weeks later. All sexual inappropriateness ceased after 1 month, and 5 months later the medication was able to be discontinued without any recurrence of hypersexuality.
It is important to stress that consenting sexual activity between residents with dementia should not be the basis for pharmacologic intervention,25 and adequate psychosocial review of any sexual expression by a resident in a nursing facility needs to be thoroughly examined before requesting interventions designed to stop such behaviors. The needs and desires of the residents in question must take precedence over those of their children who may, in fact, strongly oppose any sexual activity between their parent and another individual.
Estrogens. Few reports have documented the use of estrogen for treatment of sexually inappropriate behaviors in older men with dementia. This may be due partly to the increased occurrence of cardiovascular risk factors and previous strokes in this population, and also the causative link between estrogen use and deaths related to cardiovascular disease in men with prostate cancer who had been treated with diethylstilbestrol (DES).26
Estrogen acts similarly to MPA, in that testosterone production is decreased by estrogen’s effect in decreasing pituitary FSH and LH secretion. Common potential side effects are increased fluid retention, nausea, vomiting, and gynecomastia. In one study by Kyomen et al,27 DES was used in a 94-year-old male with dementia and repeated sexual aggression (forcible insertion of his penis into a female resident’s mouth and repeated thrashing against her). Therapy with DES was initiated at 1 mg daily, and the inappropriate behaviors ceased by 3 weeks. In another study by Kyomen et al,28 the use of conjugated equine estrogens was compared to placebo in decreasing aggressive behaviors in older residents with moderate-to-severe dementia. During this trial, residents entered a 4-week, double-blind, placebo-controlled trial phase. In the active group, estrogen dosing began at 0.625 mg, and increased by 0.625 mg increments each week, until the maximal dose of 2.5 mg at week 4 was reached. Nursing assistants rated the residents’ behavior each shift, using a modified version of the Overt Aggression Scale; weekly physical and psychiatric assessments were also obtained. While this study found that the frequency of physical aggression decreased (as did total aggression scores), estrogens were not found to be statistically significant from placebo in sexually aggressive scale ratings. However, Lothstein et al14 reported significant improvement in symptoms of sexual disinhibition in 38 out of 39 patients with dementia (males, ages 61-81) treated with oral estrogen (0.625 mg daily) or with transdermal estrogen patches (0.5 to 0.10 mg).
Gonadotrophin-Releasing Hormone Analogs. These medications stimulate LH and FSH secretion, which indirectly suppresses testosterone production by increasing systemic estrogen levels. Leuprolide acetate is a common gonadotrophin-releasing hormone (GnRH) analog used clinically, although continuous use is required to maintain clinical efficacy. Hot flashes, decreased libido, erectile dysfunction, and irritation at the site of injection have been reported as side effects. Although there are no case reports documenting the use of GnRH analogs in treating hypersexuality in older patients with dementia, there is one case report documenting the use of leuprolide acetate to successfully treat sexual aggression in a 43-year-old male with dementia and Kluver-Bucy syndrome.29
Serotonergic Agents. Selective serotonin reuptake inhibitors (SSRIs) are thought to decrease sexually inappropriate behaviors by reducing obsessive symptoms and overall libido.30 This class of agents has been found to be safe in overdose and has the added benefit of treating comorbid symptoms of depression and anxiety. Potential side effects include headache, gastrointestinal distress, insomnia, and sexual dysfunction.
A case report has documented the effectiveness of paroxetine at 20 mg in a 69-year-old male with dementia and sexual disinhibition.31 Positive effects were seen within 1 week, and the positive response was sustained at a 3-month follow-up. Another case report by Raji et al32 details the use of citalopram in a 90-year-old woman with a 2-year history of physical aggression, inappropriate disrobing, and grabbing at the pelvic area of male residents of the nursing facility. A previous trial of paroxetine was unsuccessful, and a trial of risperidone had resulted in only a partial response (decrease in physical aggression but not sexual aggression) but warranted discontinuation due to the development of extrapyramidal side effects. Trials of valproic acid and gabapentin were also deemed to have been ineffective. Citalopram at 20 mg orally decreased both physical aggression and sexually inappropriate behaviors within 1 week, with symptoms remaining in remission at a 9-month follow-up. The authors postulated that the effectiveness of citalopram (compared to paroxetine) was probably due to its higher selectivity on serotonin reuptake inhibition.
Two case reports have also documented successful treatment of paraphilias in older men with dementia with clomipramine.33 The first patient was repeatedly exposing himself (including one incident involving his granddaughter) and had failed trials of MPA and thioridazine. Clomipramine was initiated and titrated to 150 mg daily, resulting in a significant reduction in his sexual behaviors after 4 weeks. A second case involved an older male whose behaviors included public masturbation and frotteurism (becoming sexually aroused by touching and rubbing oneself against another nonconsenting person). This patient had failed trials of buspirone and thioridazine. Clomipramine was titrated up to 200 mg daily with subsequent cessation of behaviors. However, due to orthostatic hypotension that developed, clomipramine was discontinued and thioridazine was restarted. Sexual behaviors reappeared necessitating a switch back to clomipramine. Clomipramine was tolerated at a dose of 175 mg daily, with successful resolution of the offensive behaviors.
Simpson and Foster34 reported a case series of four patients between 62-72 years of age with dementia and sexual disinhibition who responded to trazodone after failing previous trials of antipsychotics (thioridazine, mesoridazine, thiothixene, and haloperidol) and benzodiazepines. Trazodone was dosed between 100 mg and 500 mg daily in divided doses. The positive response was thought to be due to trazodone’s calming effect and not its antidepressant action. Priapism is estimated to occur in 1 in 6000 patients taking trazodone, and is a potential side effect of the alpha-2 blocking action of trazodone. This side effect requires emergency intervention with intracavernal epinephrine injection.
Antipsychotics. While there are no known clinical trials on the use of antipsychotics to treat sexually inappropriate behaviors in the older adult, available evidence points to their possible efficacy.35 Their action on reducing sexual disinhibition is thought to be due to dopamine blockade. One case report involving the use of quetiapine in an 85-year-old man presenting with inappropriate sexual behaviors (masturbating to the point of genital trauma) and concurrent underlying parkinsonism and dementia has been published.36 After failing a trial of cyproterone acetate and developing diarrhea after 2 oral doses of paroxetine at 5 mg daily, quetiapine was started at 25 mg daily (orally). His sexual behavior stopped within 2 days and did not resume in the 2-month follow-up period. There was no exacerbation of parkinsonism, and blood pressure remained controlled during this 2-month period. The recent black-box warning of sudden death with the use of antipsychotics in older adults with dementia issued by the Food and Drug Administration is an important point to consider when using these agents.37
Mood stabilizers. While there are no case reports on the use of mood stabilizers specifically for the treatment of sexually inappropriate behaviors in the older adult with dementia, valproic acid and carbamazepine have been utilized to treat behavioral disturbances (including hypersexuality) associated with dementia.38,39 Potential side effects include tremors, sedation, falls, weight gain, and the potential for hepatotoxicity.
Cimetidine. Cimetidine is an H-2 receptor antagonist with antiandrogen effects. In a retrospective review conducted by Wiseman et al,40 out of 20 patients (17 men, 3 women) with sexually inappropriate behaviors and dementia were found to have responded positively to cimetidine use at doses ranging from 600 mg to 1600 mg daily. These 14 patients had also responded to either spironolactone 75 mg daily, ketoconazole 100 mg to 200 mg daily, or to all three medications. The average age of the patients reviewed was 73 years. Response time ranged from 1-8 weeks. Cimetidine-related side effects included headaches, nausea, and arthralgias. Recall bias and the subjective nature of the responses were the major potential limitations of this study.
Pindolol. Pindolol is thought to decrease sexually inappropriate behaviors by decreasing adrenergic drive, thereby reducing agitation, aggression, and hypersexuality. In one case report, a 75-year-old man with dementia and aggressive, hypersexual behaviors that included verbal comments, self-exposure, and attempted fondling was administered pindolol 40 mg daily, along with haloperidol 3 mg daily and hydroxyzine 100 mg daily41 (the latter 2 medications had not shown any benefit when used without pindolol). Time to a positive response was 2 weeks. Common potential side effects of pindolol include fatigue and hypotension.
Cholinesterase Inhibitors. While these agents have been found to be useful in treating the cognitive dysfunction and behavioral disturbances associated with dementia,42 there are no case reports on the use of cholinesterase inhibitors or the NMDA receptor antagonist (ie, memantine) in the treatment of sexual aggression associated with dementia.
Continued on next page
ETHICAL ISSUES
Hypersexual behaviors in a LTC resident can interfere with the therapeutic alliance and create a burden for staff, other residents, and family members. However, the use of medications also poses certain ethical concerns. The use of hormonal agents for the treatment of hypersexuality in the older adult is a sensitive ethical subject. Issues inherent in cases involving pharmacologic management of sexually inappropriate behaviors include the ability of the person to give informed consent, the side-effect profile of the medications, and the social stigma associated with their use. For example, hormonal agents are sometimes viewed as “chemical castration.” It is imperative to address the ethical conflicts by engaging in discussion with caregivers and family about the risks and benefits of using such medications.
Using medications to address sexual disinhibition issues in LTC residents with dementia should be an intervention of last resort, following the use of behavioral and other nonpharmacologic techniques. Adequate documentation of these initial interventions is critical. Careful Care Plan meetings, involving the legal next-of-kin (when the resident is deemed to be incompetent), the resident herself or himself (if possible), as well as the interdisciplinary team, should always be a critical first action completed prior to the initiation of any medication for sexual disinhibition.
PROPOSED EVALUATION AND TREATMENT
Based on the literature, we propose the following general approach to the evaluation, management, and possible pharmacologic treatment of LTC residents with sexually inappropriate behaviors due to sexual disinhibition associated with dementia. A treatment algorithm is proposed that recommends a systematic and organized approach based on a review of the available scientific literature (Figure).
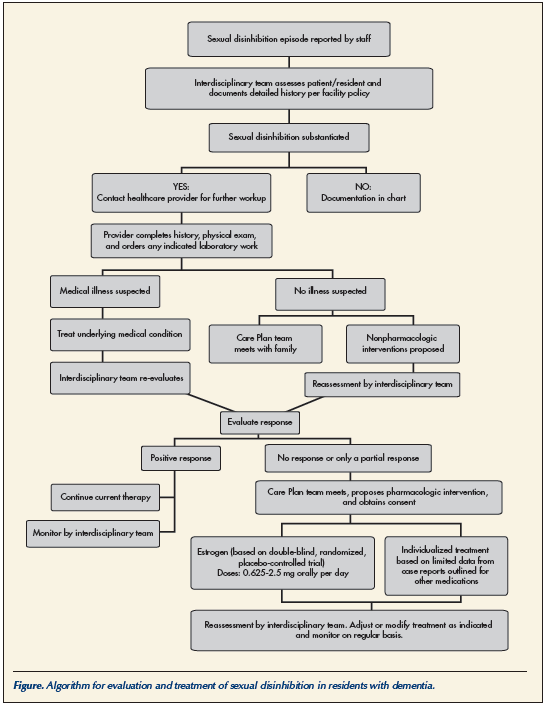
When sexual disinhibition incidents are initially reported by staff members, the interdisciplinary team should thoroughly investigate, interview all relevant personnel, including the resident himself or herself, and document the findings. If an episode of sexual disinhibition is substantiated, the health care provider should be contacted to complete an appropriate physical exam and order any indicated laboratory work to rule out an underlying medical illness or condition that could account for the sexual activity being observed.
If underlying medical conditions are found, then treatment for these conditions should be ordered and the effect on the reported sexual behavior observed after completion of the intervention. If no underlying condition is suspected of causing the behaviors, then the Care Plan team, including the attending physician, should meet with the family or legal next-of-kin, and nonpharmacologic interventions should be discussed and ordered. Reassessment by the interdisciplinary team should be conducted on a regular basis following these interventions.
If a positive response is obtained, the current therapy should be continued. If there is no response, or an unacceptable clinical response is noted, then the Care Plan team should again meet with the family or legal next-of-kin. At this time, pharmacologic interventions may be discussed. If the team feels that medication therapy would be useful, oral estrogen 0.625 to 2.5 mg every day can be initiated in male residents. If estrogen is contraindicated, the attending physician would also need to individualize therapy based on the limited data available from case reports. Pharmacologic interventions for female residents with dementia having sexual disinhibition would need to be individualized based on limited scientific evidence. Consent should be obtained from the next-of-kin and the Care Plan updated to reflect the proposed therapy and the specific target behaviors to be addressed by the therapy. Once initiated, observations for adverse side effects and response to the medications should be regularly reassessed by the interdisciplinary team. Adjustments to the dosage or changes in therapy should ideally be discussed by the Care Plan team as needed or indicated.
THE MEDICAL DIRECTOR’S ROLE
The LTC facility’s medical director can play a vital role in overseeing the approach to the evaluation and management of sexually inappropriate behaviors. He or she should also play a critical role in educating the staff on differentiating normal sexual expression in a resident with dementia from those disinhibited sexual behaviors that may be pathological or dangerous to other residents. The medical director is responsible for overseeing the implementation of all policies and procedures in the facility involving resident care,43 and should be involved in the development of all proposed facility-wide interventions, protocols, and policies for the residents described here.
Along with the resident’s attending physician, the medical director can greatly assist the nursing facility in dealing with the potential inflammatory reaction from family members, staff, and the public at large that can surround acts of sexual disinhibition that may rarely occur. The early involvement of the facility medical director regarding any alleged incidents can be instrumental in helping to oversee the proper evaluation of sexual disinhibition in the LTC setting, and he or she can act as a liaison between the administration, staff, and family members.
SUMMARY
Sexual inappropriateness remains one of the least understood and most difficult to treat behavioral issues seen in LTC residents with dementia. Separating agitation and normal sexual expression from true sexual disinhibition can be difficult, and requires a thorough evaluation on-site by the resident’s healthcare provider and the interdisciplinary team. Careful evaluation of the resident’s past medical and sexual history should also be included, and any potential medication or illness-induced causes of hypersexual or paraphilic behavior should be addressed.
When initial nonpharmacologic measures have failed, pharmacologic agents should be considered as part of the Care Planning process for that individual resident. Class I evidence indicates that estrogen therapy may be considered first, followed by the other agents discussed above. Given the paucity of comparative data, the choice of medication should be based on the individual’s medical condition and ability to tolerate medication side effects. Even though case reports suggest that antiandrogens, estrogens, GnRH analogs, and serotonergic agents may be beneficial in controlling sexually inappropriate behaviors, they do not provide a basis for comparison and lack long-term follow-up and efficacy studies. More controlled comparative trials with larger groups of patients/residents, including women, with longer follow-up periods would be required to better assess their appropriate role, if any, and the safety of any of these agents. Future research should also focus on early detection and prevention of sexually inappropriate behaviors to improve quality of life and reduce undue suffering of residents with dementia living in nursing facilities, while also reducing caregiver burden.
A systematic and organized approach to the evaluation and treatment of sexual disinhibition in LTC residents with dementia should be implemented within each facility, using a formal policy and procedure, including the input and oversight of the medical director. These policies should stress the importance of the interdisciplinary team in addressing this challenging issue.
Acknowledgments The authors wish to thank Jean K. Pals, RN,BC, and Julie S. Altman, PharmD, for their editorial comments on the manuscript.
The authors report no relevant financial relationships.










