The Physician’s Role in Screening Long-Term Care Facility Admissions
INTRODUCTION
With the advent of multiple payor sources, transition of patients to long-term care (LTC) settings from hospitals, subacute care units, emergency departments, or other sites is often based on reimbursement issues or contract-derived agreements. As a result, the attending physician’s role in screening these potential admissions to nursing facilities has become very attenuated. Nursing facilities are increasingly faced with referrals of more medically complex patients due to the diagnosis-related group payment system for acute care hospital stays, and the associated economic incentives for these entities to reduce total length of stay.
The type of subacute services being offered in LTC facilities has been well described by Levenson.1,2 Although screening by facility medical directors of high-acuity patients for possible admission to subacute units (Medicare Part A-covered stays) has been discussed previously,3 the current role of the attending physician with regard to screening of potential LTC admissions has been the subject of fewer published reviews.
The medical director’s role is primarily for the implementation of resident care policies and the overall coordination of medical care in the facility; it does not include the direct resident care responsibilities of the attending physician for any particular resident. The medical director also has direct input into the development of all facility admission policies and procedures.
Common reasons for admission of an individual to a LTC facility include postsurgical recovery, chronic dementia or other neurodegenerative processes with a significant requirement for assistance with activities of daily living (ADLs) or behavior-related issues, continued treatment for stroke-related injuries, significant pressure ulcers, or other chronic medical conditions requiring 24-hour-a-day nursing supervision (eg, hypertension, chronic obstructive pulmonary disease, cardiovascular disease, diabetes mellitus, Parkinson’s disease, or osteoporosis). Many residents in nursing facilities may have more than one active medical condition and, as such, experience multiple issues and concurrent psychosocial concerns. Thus, it is imperative that the interdisciplinary team approach to the delivery of quality care be utilized at all times. Such a team will typically consist of the attending physician, nursing staff, speech therapist, physical therapist, occupational therapist, social worker, dietitian, pharmacist, and other allied health professionals. Critically, the LTC resident (or his or her next of kin if the resident cannot participate) should also be involved in the development of the care plan and overall goals.
In addition, nurse practitioners (NPs) and physician assistants (PAs) are playing an increasingly valuable role in providing direct resident care in the LTC setting. The NPs and PAs have varying independent authority, as determined by state regulations and laws. However, they play an important role in the day-to-day evaluation of acute changes in a LTC resident’s condition. Although the literature is sparse on this issue, NPs and PAs may also assume some screening responsibilities for new LTC admissions on behalf of the attending physician. Attending physicians, NPs, and PAs cannot currently bill for services in connection with the assessment and screening of potential nursing facility admissions.
A revision of F-Tag 501, a component of the Centers for Medicare & Medicaid Services (CMS) regulations for nursing facilities, became effective on November 25, 2005.4 This Tag describes the responsibilities for a nursing facility medical director, and the implications of this revision have been excellently summarized by Elon.5 One of these responsibilities includes the oversight for admission policies and care practices that address the types of residents that may be admitted, based on the facility’s ability to provide all required care needs for the potential admission. These admission policies should be individualized for each specific nursing facility based on staffing levels, appropriate training, and the availability of any required ancillary services (eg, rehabilitation, wound care units).
A different F-Tag, 285, discusses preadmission screening for individuals who are either mentally ill or mentally retarded, and F-Tag 385 states that a physician must personally approve in writing that an individual be admitted to a nursing facility.6 There exists, therefore, significant federal guidance directing that the attending physician have input in deciding if a potential resident is suitable for admission.
CLINICAL ASPECTS OF SCREENING LTC ADMISSIONS
The attending physician should assist the LTC admissions coordinator in the clinical aspects of screening potential admissions. As a critical component of this procedure, an effective method of information transfer directly from the referring facility should be established. The request for admission can come from a variety of sources including acute care hospitals, group homes, assisted living facilities, psychiatric facilities, or from a resident’s home. Information that should be obtained from these referral sources for purposes of screening a potential resident to ensure all needs can be met are: (1) the resident’s past and recent medical history, including any surgical procedures; (2) a current list of medications and laboratory data; (3) any history of falls, wandering, or elopement episodes; and (4) any abusive, violent, or sexually inappropriate behaviors. Comorbid illnesses can affect postoperative complication rates or survival,7,8 and should be taken into account at the time of screening.
Additionally, the potential resident’s level of cognitive and physical ability, the need for further rehabilitation for disabilities, required modes of transfer, and mobility needs must also be taken into consideration prior to acceptance to ensure that appropriate therapies can be provided. Any nutritional and hydration issues should be identified, as well as the presence of any skin disorders, including pressure ulcers. Pressure ulcers should be staged, described in detail, and reviewed by the facility’s wound care nurse to ensure that proper care can be given following admission. Current advance directives (including Do-Not-Resuscitate [DNR] status) should also be noted if available. A contact telephone number for the hospital attending physician, as well as a family contact name and number, should be listed to allow for ease in clarification of any information.
Much of this useful information typically can be found on a hospital or other facility discharge summary. However, this summary may not be available at the time of screening or even at the time of transfer to the LTC facility. The development of a medical transfer form may be needed to collect the required information in order for the LTC facility to properly screen the individual as a potential admission. A sample form is shown in the Figure. This form could be used for the transfer of a patient between any two facilities. Such resident transfer forms have been proposed before,3,9,10 although most have focused on the transfer of residents from LTC nursing facilities to emergency departments of hospitals. The physician who cared for the resident in the community would also be a good source of information, and, ideally, a copy of past medical records should be requested for review prior to admission.

The LTC facility may assign a nurse to visit the individual for potential admission in his or her present setting to assess the number of nursing care hours that will be required to provide proper care, as well as to collect pertinent medical data for use by the attending physician and admissions coordinator in order to expedite the review process. In general, any high-acuity individuals should not be granted final admission approval to the LTC facility until the medical director or attending physician has carefully reviewed all available data and discussed the case with the admissions coordinator and director of nursing.
Prior to admission to the facility, all arrangements should be made for any specialized equipment needs to be available upon arrival of the resident (eg, specialty bed, oxygen, respiratory or rehabilitative equipment that may not be routinely stocked). To improve efficiency for the accepting facility and to enhance continuity of care, it is necessary to thoroughly review special requirements for all potential admissions prior to acceptance from the referring facility or other entity. As with the procedure for subacute unit admissions, acceptance of persons for admission to LTC floors should follow established facility criteria and staffing availability in all cases, and routine exceptions to these policies should be avoided.3
THE ROLE OF THE ATTENDING PHYSICIAN IN THE LTC FACILITY
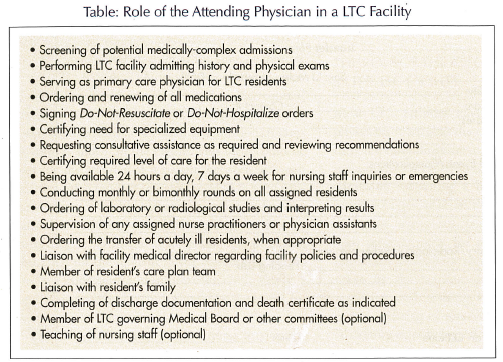
Most LTC facilities have a number of attending physicians managing the care of their residents, and their responsibilities are many (Table). Top priorities include the initial screening of the resident prior to admission, obtaining a history and performing a physical examination of the resident (usually within 3 days of admission), performing monthly rounds with progress notes for the first 90 days (may be bimonthly thereafter), returning telephone inquiries made by the nursing staff in a timely manner, reviewing and revising of pharmacological treatments, ordering of consults, ordering of appropriate laboratory or radiological tests along with the evaluation of results, obtaining adequate cross-coverage, and assisting and facilitating the interdisciplinary team approach to the care of the LTC resident. Educational inservice training should be conducted on a regular basis, and the attending physician should actively support and participate in these educational programs, if at all possible. The attending physician must also be available 24 hours a day, 7 days a week for nursing inquiries or to respond to resident emergencies, or have a designated covering physician identified. The medical director of a facility serves as the emergency alternate physician when the primary attending physician cannot be reached.11,12
Current advance directive and DNR instructions should be obtained from the referring hospital when possible, but should be verified with the patient/resident (or legal next of kin as appropriate) in case any changes are desired. For example, many times preferences regarding further acute care hospitalization may be given by the resident or their representative at the time of admission to the LTC facility. Any such discussions should be well documented in the LTC facility medical record by the attending physician. A detailed review of DNR and Do-Not-Hospitalize directives pertaining to patients admitted to skilled nursing facilities has been published.13
QUALITY ASSURANCE AND RISK MANAGEMENT ISSUES
The medical staff of a LTC facility should preferably include physicians and other health care professionals who have the appropriate training and experience in the areas of service to be offered to residents of that facility; this may include physical rehabilitation medicine, orthopedics, and occupational, speech, or wound therapies. Although challenging in today’s environment, LTC facilities should make diligent efforts to encourage and recruit local Family Practice and Internal Medicine physicians to provide primary care coverage to their admitted residents. Facilities receiving Medicare and Medicaid monies are required to follow those regulations specified in the Omnibus Budget and Reconciliation Act of 1987.14 Violations of these regulations serve as the basis for regulatory deficiencies during the survey process, but also may be cited in any subsequent legal action against the facility and/or the health care providers.
Attending physicians, in conjunction with the facility’s medical director, must ensure that all admissions policies and procedures regarding new admissions address the specific ability of the facility to provide all required care to the resident. This care may need to include special ancillary services such as physical, occupational, or speech therapy, pressure ulcer care, intravenous or central line administration of fluids and antibiotics, or other medical needs that may not routinely be provided by that particular facility. Procedures should be developed to ensure that referred individuals requiring subacute care, rather than regular long-term care, be properly identified at the time of screening and prior to admission.3 The facility medical director should be utilized in cases where the appropriate placement within a facility of a potential new admission is not clear.
With regard to new orders issued by covering physicians on behalf of the LTC facility attending physician, it is important that a timely report and follow-up be obtained with the attending physician to ensure that he/she is in agreement with all new orders that may have been given during his/her absence. The attending physician should also conduct a regular review of available ancillary and consultative service that can be obtained by the facility such as specialty physicians, laboratory, radiology, pharmacological, and physical, occupational, and speech therapies, as well as any specialty support services (eg, dialysis, central line, wound care). The attending physician should be aware of facility policies that are directly related to the care that is expected to be rendered by him/herself or any NPs or PAs under his/her supervision. It is also imperative that the physician be advised of any untoward events occurring to residents assigned to his or her care, and that appropriate policies and procedures are in place within the facility to investigate cause and outcomes of such incidents.15
As previously stated, during the past several years, NPs and PAs have assumed an important and active role in the clinical management of LTC residents. Although many states allow NPs and PAs to operate with minimal supervision, oversight and responsibility for their clinical actions ultimately remains with the attending physician, as does any legal liability for orders or treatments given or omitted in the care of their assigned facility residents.
An effective working relationship should be maintained with the facility’s medical director and the attending physician, and he or she should be actively involved in the development of the policies dealing with care issues.12,15 As legal and civil actions alleging poor care and neglect are becoming more and more prevalent in the LTC industry, the attending physician should be aware of the importance of merging quality care with risk management issues.16
SUMMARY
An informed and actively involved attending physician is critical in maintaining quality, cost-effective care in today’s LTC facilities. Screening by the attending physician prior to a resident’s admission into the nursing facility enables the interdisciplinary team to be reassured that all the needs of the potential resident can be met by the facility and its staff.
It is important that both the facility medical director and the attending physician be aware of all current CMS regulations concerning the requirement for appropriate admissions policies and procedures to be developed in every nursing facility. Attending physicians, in conjunction with the facility’s medical director, must ensure that all admissions policies and procedures regarding new admissions address the specific ability of the facility to provide all required care to the resident.
Additionally, the attending physician should determine if any referred individual is suitable for admission to a particular nursing facility. The attending physician plays a complementary role to that of the facility medical director in the screening of potential new admissions. Only by incorporating a team approach to the screening, admission, and care processes can we achieve optimal benefit to both the resident and the facility, allowing for more specialized care to be available to this unique segment of our society.
The authors report no relevant financial relationships.










