Examining Oral Health in Nursing Home Residents and Overcoming Mouth Care–Resistive Behaviors
Nursing home residents are a group with significant health disparities in the area of oral health. Poor oral health can place nursing home residents at risk for developing pneumonia, exhibiting poor glycemic control if already diabetic, and increasing cardiovascular disease. The majority of nursing home residents arrive with some or all of their dentition but without the resources to continue preventive dental care—Medicare does not reimburse for routine dental care and Medicaid either does not reimburse for this service or reimburses so poorly, few providers will accept it. The onus of mouth care falls on nursing assistants; many admit to failing to provide mouth care because of mouth care–resistive behaviors. Clinicians in nursing homes can model specific methods to reduce mouth care–resistive behaviors (for example, bridging, priming, and avoiding elderspeak) and share these techniques with the nursing assistants responsible for providing mouth care. (Annals of Long-Term Care: Clinical Care and Aging 2010;18[1]:21-26)
___________________________________________________________________________________________________________________________________
Introduction
In the United States, nearly 2 million older adults reside in 16,100 nursing homes (NHs).1,2 The majority of these elderly individuals require assistance with activities of daily living (ADL),3 and nursing assistants (NAs) are the predominant providers of this care.4 The National Institute of Dental and Craniofacial Research (NIDCR) recognizes these NH residents as a group with significant health disparities in the area of oral health.5 The existence of acute and chronic diseases may create a negative spiral in which the diseases are worsened by the presence of poor oral health, which deteriorates as their medical problems progress.6 The oral health status of NH residents has been described as “deplorable.”7 There are emerging connections between poor oral health and poor systemic health. The number of residents retaining their natural teeth exacerbates the problem of poor oral care in NH. In the early 1980s, 54% of persons age 65 years or older had some natural teeth; by 2002, the percentage had increased to 70%.5 The purpose of this review is to describe the oral health of elderly NH residents, the effect of mouth care–resistive behaviors on the oral health of these residents, and specific interventions to reduce mouth care–resistive behavior.
General Description of the NH Population
The current NH population is frail and functionally dependent. Ninety-one percent of NH residents are 65 years of age or older, and 46% are 85 years of age or older.3,8 Eighty-three percent require assistance with three or more ADL.9,10 The three most common ADL requiring assistance were bathing or showering (96%), dressing (87%), and eating (45%).3 Oral care was not specifically mentioned in any ADL category, but one could conservatively estimate that the 45% who required assistance with eating would most likely require assistance with mouth care. Self-care is further compromised by cognitive impairment; 70% of NH residents exhibit some form of cognitive impairment regardless of diagnoses.9
Oral Health Affects Systemic Health
Nearly one-third of all older adults experience xerostomia, or dry mouth, due to hyposalivation.11 Xerostomia causes mouth discomfort, interferes with chewing and swallowing, and supports plaque formation.11 Furthermore, saliva has antibacterial properties; diminished saliva production results in increased bacteria in the mouth. In a study of 225 residents of a geriatric facility, researchers found significant relationships between xerostomia and oral health.12 Persons with high levels of xerostomia were three times more likely to describe their oral health as fair to poor; five times more likely to express dissatisfaction with their oral health; and three times more likely to believe their oral health had worsened as a result of the xerostomia.12
Medications are the most common causes of xerostomia.12 The average NH resident takes eight medications daily.8 Anticholinergics, antihypertensives, antidepressants, diuretics, anxiolytics, and antihistamines diminish salivary production and alter the ability of the oral environment to fight the effects of pathogens.13,14 Many medications commonly prescribed for elderly patients, especially calcium channel blockers and anti-seizure medications, result in gingival overgrowth, which further predisposes the NH resident to caries and periodontal disease.13,14 The effect of medications taken by NH residents increases the importance of meticulous oral care.
Poor oral health interferes with the ability to chew food and can place residents at risk for malnutrition. In a study of 187 NH residents, researchers noted associations between persons with highly compromised dentition (edentate, edentate with 1 full-denture plate, or 6 or fewer teeth) and weight loss.15 In another study that examined relationships between oral health status and weight in persons newly admitted to a NH, researchers found an association between body mass indices below 22 and poor oral health.16
In addition to xerostomia and weight loss, poor oral health can cause other systemic problems. Emerging empirical evidence suggests links between poor oral health with plaque deposition and NH–acquired pneumonia (NHAP) or aspiration pneumonia.17-27 The accumulation of plaque in oral cavities potentially may serve as a source of colonizing respiratory pathogens; organisms responsible for pulmonary infections (eg, Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis) are hypothesized to reside in the plaque of persons with poor oral hygiene.28 Mature plaque also encourages the colonization of the oropharyngeal site with potential respiratory pathogens such as Klebsiella pneumoniae, Pseudomonas aeruginosa, and Staphylococcus aureus.23 These same organisms have been identified as causative agents of NHAP in several studies, although the etiology of NHAP was not identified in half of the confirmed cases. The larger the amounts of plaque, the greater the opportunity for the oral cavity to be colonized by potential respiratory pathogens.29 Thus, improved mouth care with subsequent bacterial removal and plaque reduction may reduce the incidence of pneumonia in NH residents.30
Links between diabetes and periodontal disease have been established in the literature, albeit not with elderly NH residents. Bakhshandeh et al31 found that none of their 299 dentate subjects with diabetes had healthy periodontia. Tsai and colleagues32 examined the association between type 2 diabetes mellitus (DM) and periodontal disease using data from the National Health and Nutrition Examination Survey III. They found that persons with glycosylated hemoglobin values greater than 9 were nearly three times as likely to have severe periodontal disease as those with glycosylated hemoglobins of 9 or lower. These findings were echoed in another study of 100 outpatients in Japan diagnosed with type 2 DM.33 Increasing age and greater amounts of plaque were inversely correlated with the number of remaining teeth.33 Promsudthi et al34 compared glycemic control between two groups of older adults with type 2 DM. The experimental group that received aggressive periodontal treatment showed improved plaque scores, periodontal disease, and fasting plasma glucose levels after 3 months over the control group.34
The presence of periodontal disease and the development of cardiovascular disease has been examined. In a study that examined the oral health of monozygotic twins in which one twin had coronary heart disease and the other did not, Tabrizi et al35 noted that the twin with heart disease had significantly more gingival bleeding and evidence of periodontal disease than the healthy twin. A series of findings from the Oral INfections and Vascular Disease Epidemiology Study (INVEST) have established relationships between poor oral health and cardiac disease. Researchers have noted positive associations between tooth loss, subclinical periodontal disease, and carotid artery plaque when controlling for age and other confounding variables.36 The same researchers also discovered a direct relationship between the amount of bacteria on dental plaque and the mean carotid artery intima-media thickness in 657 subjects with no history of cardiovascular events.37 Bacteria associated with periodontal disease was colonized in the great saphenous veins of women with varicose veins.38 Periodontal disease is thought to produce cytokines that play a part in coronary heart disease.39 Some researchers have reported associations between periodontal disease and C-reactive proteins.39,40 The INVEST team, however, found no association between C-reactive protein values and bacteria levels.37
Overall Oral Health of NH Residents
More older adults are entering NHs with some or all of their teeth. Using data from the 1995 National Nursing Home Survey, Dey41 calculated that 52.3% of NH residents were dentate. From 1988 to 2004, edentulism decreased from 34% of all adults over age 65 to 27%.42 For adults in the 65-74 years of age bracket, edentulism decreased from 28.6% to 23.9% during the same time; the reduction in edentulism for adults age 75 years and older was more impressive, decreasing from 40% in 1998 to 31% in 2004.42 The average number of teeth for all elderly persons age 65 years and older in 2004 was 18.9 teeth.42
The paradox of aging and oral health is that as more older adults keep their teeth, the resources for maintaining dental health diminish. According to the Agency for Healthcare Research and Quality, 70% of persons age 65 years and older lacked any dental insurance, as compared to 34% of persons age 45-64.43 When dental coverage for older adults was examined according to age strata, 64.6% of older adults age 65-74 lacked dental insurance and 75.7% of adults age 75 and older lacked dental insurance.43 Medicare does not cover routine dental care; Medicaid coverage varies between states but either does not cover dental care or compensates dentists so poorly that no one will accept it.44 The lack of resources for maintaining oral health results in situations where more dentate older adults who reside in NHs are at risk for tooth loss from dental caries and periodontal disease. Dentate older adults are especially vulnerable to caries around previous restorations, such as fillings and crowns.13 Caries can occur when the root surfaces are exposed as a result of periodontal disease in older adults.13 Older adults may form plaque more quickly than their younger counterparts when oral care is not routinely performed; this may be due to gingival recession, which exposes more tooth to the oral environment, and also due to reduced salivary flow.13 Tooth loss may cause shifting of remaining teeth to the point where occlusal surfaces no longer articulate, interfering with chewing and swallowing functions.
In spite of the tremendous importance of oral health to NH residents, there is evidence that oral care is suboptimal in the NH and is showing no improvement over time. In 1977, Bagramian and Heller45 conducted a dental health survey involving 112 patients. The average number of decayed, missing, and filled teeth (DMFT) was 26.7 for all residents; for the 44% who were dentate, the DMFT was 19.96.45 The need for better oral hygiene was noted in this study. Thirty years after the Bagramian study, Murray et al46 measured the oral health of 265 NH residents in South Florida and found that 79.6% of the 265 residents in their sample were dentate, and all had calcified plaque on their tooth surfaces. One-third of the residents had calculus that covered two-thirds or more of the tooth surface. Murray et al46 concluded that “a high proportion of elderly nursing home residents suffer from oral hygiene and oral health neglect.” In a smaller study conducted in New Jersey, researchers reported similar findings: of the 137 predominantly African-American NH residents examined, 61.9% had plaque and 55.4% had calculus; the mean DMFT was 23.8.47
While researchers have found that the lack of professional dental care may be an important factor for the poor oral health of elderly NH residents, poor daily oral care provided by caregivers may be the most significant singular factor for poor oral health.48-50 This observation was supported by findings that frail NH residents who required assistance with several ADL were highly likely to have poor oral health.45,51,52 The fact that mouth care and oral health in this highly vulnerable population is the responsibility of NAs who have received minimal training in providing adequate and effective mouth care further compounds this health dilemma.
One study in the literature reported the results of actual observation of NAs providing mouth care. Coleman and Watson53 observed 47 NAs from five NHs provide mouth care to 67 dentate residents. They compared the observed behavior to an oral care instrument validated by ten experts. The mean age of the NH residents was 83 years, and the majority (76.1%) were female. Nearly 90% were diagnosed with dementia; the mean Mini-Mental State Examination score was 6.8. All needed significant help with dressing and bathing, and 94% required assistance with personal hygiene, including mouth care. Only 28% received any type of mouth care; of that number, the average time for received mouth care was 1 minute and 12 seconds.
Older Adults and Mouth Care: Fighting and Biting
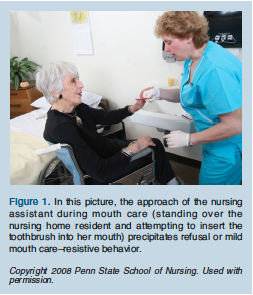 One theme reported throughout the oral care literature was mouth care–resistive behaviors, often described as biting and fighting. These mouth care–resistive behaviors included not opening mouths, refusing mouth care, biting the toothbrush, kicking or hitting, and biting the NA.54 Mouth care–resistive behaviors were most likely to occur when NAs provided physical assistance than with cueing or supervision. In fact, the way in which the NAs attempted to provide mouth care often elicited mouth care–resistive behavior. One NA tried to provide mouth care to a resident who was suspended in a mechanical lift in mid-air; the resident tried to bite the NA. Other precipitants to mouth care–resistive behavior included attempts to forcefully insert the toothbrush or swab into residents’ mouths without alerting them, lack of praise or encouragement, no smiling or positive facial cues, and no prompts or gestures.53 (Figure 1).
One theme reported throughout the oral care literature was mouth care–resistive behaviors, often described as biting and fighting. These mouth care–resistive behaviors included not opening mouths, refusing mouth care, biting the toothbrush, kicking or hitting, and biting the NA.54 Mouth care–resistive behaviors were most likely to occur when NAs provided physical assistance than with cueing or supervision. In fact, the way in which the NAs attempted to provide mouth care often elicited mouth care–resistive behavior. One NA tried to provide mouth care to a resident who was suspended in a mechanical lift in mid-air; the resident tried to bite the NA. Other precipitants to mouth care–resistive behavior included attempts to forcefully insert the toothbrush or swab into residents’ mouths without alerting them, lack of praise or encouragement, no smiling or positive facial cues, and no prompts or gestures.53 (Figure 1).
Strategies for Reducing Mouth Care–Resistive Behavior
Mouth care–resistive behaviors are actions “invoked by a caregiving encounter…defined as the repertoire of behaviors with which persons with dementia withstand or oppose the efforts of a caregiver.”55 In earlier research, behavior meeting this definition was usually labeled as “uncooperative behavior,”56-58 “disruptive behavior,”59-61 or even as “agitation.”62 Volicer et al62 and Mahoney et al55 distinguish agitation from mouth care–resistiveness using contextual cues: agitation usually occurs without a preceding event while mouth care–resistive behavior occurs as a response to a precipitating event. Agitation is evident in persons with mild dementia and increases with moderate dementia before waning as the dementia progresses to severe.62
Resistiveness to care, however, increases exponentially as the severity of dementia increases; one study found an eightfold increase of mouth care–resistive behavior when dementia progressed to severe.62 Agitation and mouth care–resistiveness can occur at the same time; one study noted that in a sample of nearly 24,000 residents of Veterans Administration NHs, agitation alone was found in 17%, mouth care–resistiveness alone was found in 9%, and both were found in 8% of the subjects.62 Mahoney et al55 have further conceptualized their model of mouth care–resistive behavior as having three major components: antecedents (characteristics of both the resident and caregiver, context of the interaction); resistiveness (dimensions of the behavior, such as turning away or saying no, and parameters of the behavior, such as frequency and duration of the behavior); and consequences (inadequate completion of caregiving activities, discomfort of the resident).
One of the best ways to avoid precipitating mouth care–resistive behavior, and to minimize its impact should it occur, lay in communication strategies. Both Williams et al63 and Cunningham and Williams64 have documented the increased probability that elderspeak will provoke mouth care–resistive behaviors. Elderspeak is a term used to describe “baby talk” speech patterns associated with infants and pets but inappropriately employed when engaged with older adults: high pitch, short sentences, sing-song cadence, patronizing tone, use of collective pronouns, and infantilizing terms (baby, honey, dearie). Williams et al63 analyzed 80 videotapes of 20 NH residents for relationships between elderspeak and mouth care–resistive behavior; they found that elderspeak resulted in the highest probability of care-resistant behavior (55%), followed by silence (36%).
Kayser-Jones et al65 analyzed qualitative data from two studies that involved mouth examinations of persons with dementia and found specific strategies that prevented or reduced mouth 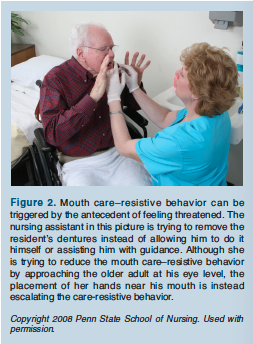 care–resistive behaviors. These strategies included: establishing rapport; positioning oneself at or below eye level; maintaining friendly, nonthreatening facial features; judicious use of touch; providing a quiet environment; speaking and moving slowly; using nouns instead of pronouns; and using multiple communication strategies, such as gestures and pantomime.65,66
care–resistive behaviors. These strategies included: establishing rapport; positioning oneself at or below eye level; maintaining friendly, nonthreatening facial features; judicious use of touch; providing a quiet environment; speaking and moving slowly; using nouns instead of pronouns; and using multiple communication strategies, such as gestures and pantomime.65,66
In Coleman and Watson’s53 study of mouth care provided by NAs, the NAs definitely precipitated care-resistant behavior by violating nearly every strategy listed here. When NAs performed mouth care on persons with dementia instead of allowing them to perform as much of it as possible, the NAs unwittingly precipitated mouth care–resistive behavior in some of their residents.53 (Figure 2).
An additional strategy to reduce this antecedent of mouth care–resistive behavior is the use of preserved implicit memory. Implicit memories, also described as procedural or unconscious memories, are those memories surrounding specific tasks learned early in childhood and repeated throughout adult life.67,68 A person with dementia, for example, may not be able to name a toothbrush if asked; however, if the nurse were to place the toothbrush in the person’s hand, he or she would start brushing his or her teeth. Priming is one method to elicit implicit memory.68 Wetting a toothbrush, placing toothpaste on it, and then handing the toothbrush to a person with dementia are strategies that could prime the release of implicit memories surrounding the task of mouth care.67 Some of Chalmers’66 strategies for dental professionals working with persons with dementia were congruent with the constructs of implicit memory, most specifically, priming. These strategies included bridging, in which the resident holds a toothbrush while the NA brushes the person’s teeth; hand-over-hand, in which the NA places his or her hand over the resident’s hand and guides the resident with an activity such as removing or replacing dentures; and chaining, in which the NA starts the mouth care activity and the person completes it.66 (Figures 3 and 4).

Conclusion
As more elderly persons enter NHs with their own teeth, the potential for oral health problems and systemic illnesses increase. Clinicians in NHs should be aware of the problems faced by direct care workers, such as NAs, who are entrusted with providing mouth care. Clinicians should assist direct care providers with behavioral interventions, as opposed to being quick to prescribe medications to address the care-resistive behavior.
The author reports no relevant financial relationships. Dr. Jablonski is Assistant Professor, The Pennsylvania State University School of Nursing, University Park, and a 2009-2011 Brookdale Leadership in Aging Fellow.










