Bacterial Pneumonia Acquired in Nursing Homes
INTRODUCTION
Bacterial pneumonia acquired in the nursing home or long-term care setting provides unique management challenges. In this review, “nursing home” and “long-term care facility” will be used interchangeably. Currently, many nursing homes serve also as “subacute” care facilities, and patients move to and from acute care facilities; this can result in changes in oropharyngeal flora for nursing home care residents, similar to what is observed in acute care facilities. Severe comorbidities and impairment of functional status both increase risk of pneumonia and pneumonia-related morbidity and mortality. In order to reduce the impact of pneumonia on this vulnerable population, clinicians must be familiar with current strategies for the prevention, early diagnosis, and treatment of pneumonia in this setting. In this review, discussion will be limited to pneumonia of bacterial etiology because of its dominance as the primary cause of this infection in the long-term care setting.
EPIDEMIOLOGY
It is estimated that approximately 915,000 cases of community-acquired pneumonia (CAP) occur each year in the United States in patients age 65 and older who are living outside of long-term care facilities.1 From this study it was also estimated that the annual number of cases of CAP per 1000 elderly non–nursing home residents was 28 cases; however, for those persons age 85 and older, it was more than 50 cases. Of these non–nursing home patients with CAP, approximately 40% were hospitalized for this disease.1 The data are not available to give precise numbers for the incidence of pneumonia in the long-term care setting. However, it is estimated that approximately 33-114 cases per 1000 nursing home residents will require hospitalization for pneumonia each year, and represent 4.3% of those age 65 and older who are hospitalized annually for pneumonia.2,3 Since 31% of 155 episodes of pneumonia cases occurring in several long-term care facilities ended up being transferred to an acute care hospital,4 it can then be inferred that the true incidence of pneumonia in long-term care institutions is approximately threefold higher than the figure for actual transfer of long-term care pneumonia cases for hospital care. Thus, the true incidence of pneumonia in the long-term care setting may be as high as 100-300 cases per 1000 nursing home residents per year. Pneumonia remains the leading cause of infection in nursing home facilities resulting in transfer to acute care hospitals.5
Kaplan et al3 looked at over 600,000 hospital admissions for CAP in seniors and found that hospitalized nursing home residents were more likely to be older (mean age, 80, vs 76.8), and were more likely to be women (58.1% vs 53.4%) and have more comorbidities than hospitalized non–nursing home residents. Hospital mortality rates were higher for nursing home residents (17.6 %) versus non–nursing home residents (10.6%). These rates are substantially higher than the 5.5 % mortality rate observed for a control population consisting of elderly patients matched by age, sex, and race who were hospitalized for diseases other than pneumonia.6 It was estimated from this study that the 1-year mortality rate after being discharged alive following hospitalization for CAP is about 41% versus 29% for the control group.6 However, the 1-year cumulative mortality rate (in-hospital plus postdischarge) for elderly patients hospitalized for community- or nursing home–acquired pneumonia (NHAP) is approximately 50%, and can be presumed to be highest for those with significant comorbidities. This compares with the 1-year mortality rate of 74% observed for a study of long-term care residents of a Veterans Affairs (VA) nursing home who developed pneumonia, versus 40% for matched controls who did not develop pneumonia.7
DETERMINANTS OF NURSING HOME-ACQUIRED PNEUMONIA
Extreme old age, male sex, inability to take oral medications or difficulty swallowing, immobility, and failure to receive influenza vaccine were found to be risk factors for pneumonia in a prospective study of residents of five long-term care facilities.4 A carefully designed case-control study where pneumonia patients were matched for admission date, level of nursing care, and dependence identified large-volume aspiration and sedating medication as modifiable risk factors for NHAP.7
Pneumonia results from aspiration of oropharyngeal bacteria, and the risk of developing pneumonia is directly proportional to volume of aspirate and the virulence of the bacterial pathogens aspirated, and inversely proportional to the integrity of host defenses. Aging and the presence of comorbidities are associated with changes in pulmonary function and host defenses that in turn increase the risk of pneumonia. These changes have been reviewed extensively elsewhere and include reduction in lung elasticity, increase in airway resistance, decrease in respiratory muscle strength, and diminished force of cough.2,8 Furthermore, alterations in T-cell function play a role in the diminished response to vaccines in elderly persons. Finally, colonization of the pharynx by gram-negative bacilli (GNB) and Staphylococcus aureus (pathogenic colonization) is strongly correlated with increasing age and debility. Xerostomia, changes in immunoglobulin content of saliva, and defective swallowing are also thought to play a role in this important precursor phenomenon.
It is now confirmed that elderly patients with pathogenic colonization have reduced clearance of a radiolabel from the oropharynx.9 Interestingly, this same study noted reduced clearance of the radiolabel for patients taking antidepressants. Additionally, the number of salivary lymphocytes and the number of buccal cells per milliliter of saliva were increased in colonized patients versus non-colonized controls. Finally, elastase activity was elevated in patients who were colonized by GNB compared with non-colonized controls.9 Recent experiments also shed some light on the reduced clearance of pathogenic bacteria observed for debilitated elderly persons. Using subjects of various ages, Ho et al10 measured mucociliary clearance time (time between placement of intranasal saccharine and the subject sensing a sweet taste), and used their nasal respiratory cells to measure ciliary beat frequency and to study microtubular structural changes with age. Adults over age 40 years had prolonged nasal mucociliary clearance, slower ciliary beat frequency, and increased ultrastructural defects in nasal respiratory cell cilia. These experiments appear to confirm that aging and debilitation result in impaired oropharyngeal bacterial clearance, and abnormalities in respiratory cell cilia function contribute to diminished host defenses in both lower and upper airways.
CAUSATIVE PATHOGENS
There is a paucity of studies that clearly define the microbial etiology of NHAP. However, reviews of the older literature reflect that approximately 20% of cases are due to Streptococcus pneumoniae, 10% each are due to Haemophilus influenzae and S. aureus, and 30% are caused by aerobic GNB, while normal flora are isolated 15% of the time.5,8,11 Two recent studies more clearly defined the microbial etiology of severe pneumonia in this setting by studying nursing home residents transferred to an acute care hospital intensive care unit (ICU).12,13
In the first study, the investigators classified CAP patients as both NHAP and non-NHAP.12 Forty-seven nursing home residents admitted to the ICU and intubated also underwent protected catheter brush bronchoalveolar lavage, with quantitative culture or postmortem transthoracic needle aspiration biopsy culture. If pleural fluid was present, it was sent for culture. Blood cultures as well as urine antigen testing for Legionella pneumophila and S. pneumoniae and various serologic tests were performed. In a second study, 95 nursing home residents admitted to the ICU underwent similar testing to the first study.13 A microbial etiology could be determined in about 55% of residents. Combining the two study results, for the residents in whom a pathogen(s) was identified, S. pneumoniae occurred in 9%, S. aureus occurred in 22% (about 60% were methicillin-sensitive), and aerobic GNB (not including Haemophilus species, which occurred in 3%) occurred in 44% of residents. Mixed infection occurred in about 20% of residents with anaerobes being isolated in 20% of NHAP cases described in the later study. This differed from non–nursing home CAP cases where S. pneumoniae and Legionella species were the dominant single bacterial pathogens. The incidence of GNB was comparable for both NHAP and non-NHAP cases.
The risk of drug-resistant bacterial pneumonia in nursing home residents admitted to an ICU was correlated with a high activity of daily living score (most dependent) and previous antibiotic usage.14
CLINICAL PRESENTATION AND DIAGNOSIS
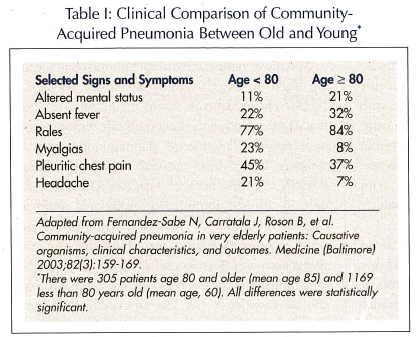
Fever, the cardinal manifestation of infection, is often absent or blunted in infected elderly patients.15 It is well established that the presentation of pneumonia in the elderly differs significantly from that of the younger adults. The classical symptoms and signs of high fever, chills, productive cough, and chest pain are often absent or minimal. Changes in mental status, falls, lethargy, and tachypnea may be the sole presentation of this disease, particularly in frail nursing home residents. Recent studies have quantified these differences in presentation.16,17 Investigators examined prospectively a cohort of patients of different ages admitted for CAP, which included residents transferred from nursing homes to acute care hospitals for treatment of pneumonia. Baseline symptoms were obtained from direct interview of patients or by interviews of close relatives or caregivers. The data led to the conclusion that the median duration of symptoms for several symptoms, including cough and sputum production, increased with advanced age, and older patients had “a significantly lower number of respiratory and nonrespiratory symptoms compared with younger patients.” Pneumonia-related fever, chest pain, headache, and myalgia were substantially reduced in prevalence with advanced age.16 Another study, which did not include nursing home residents but included substantial numbers of patients over the age of 80, found significant differences between the presentation for those age 80 and older (mean age, 85) versus those below age 80 (mean age, 60) (Table I). Altered mental status occurred nearly twice as often in the older group; pleuritic chest pain occurred less often in the old, as did myalgias and headache. Finally, fever was more likely to be absent in the older patients.17 In conclusion, symptoms and signs of pneumonia are often absent or blunted in the elderly, particularly in patients over age 80. The clinician should thus be aware that serious illness may be present despite a paucity of symptoms and signs.
The diagnosis of pneumonia in the long-term care setting is usually based on clinical data alone, given the variability in resources available for laboratory testing in this setting. Generally, fever, tachypnea, new-onset or increasing cough with purulent respiratory secretions, pleuritic chest pain, worsening hypoxemia, the new presence of rales or rhonchi, or rapidly declining functional status—especially altered mental status—should alert the clinician to the possibility that the resident has pneumonia.5,8,11,18-20
MANAGEMENT AND PREVENTION
The preliminary evaluation in the nursing home should consist of a physical examination and measuring vital signs, including temperature, respiratory rate, pulse, and blood pressure. Tachypnea (greater than 25 breaths per min) has a high predictive value for the diagnosis of pneumonia in the long-term care setting.18 Pulse oximetry should also be performed. For patients managed in the nursing home, laboratory testing, if available, should include a chest radiograph, a white blood cell count with differential, and a serum creatinine. Sputum, if available, should be sent for culture and sensitivity. Although the utility of obtaining blood cultures in the nursing home setting has not been established, if positive, they are useful in establishing the causative pathogen. There is little disagreement about the utility of blood cultures for nursing home and non–nursing home patients admitted to an acute care facility.
A recent study of about 13,000 patients hospitalized for CAP, 23% of whom were nursing home–acquired, determined that the overall risk of bacteremia from pneumonia was 7%.21 However, bacteremia was least likely to be present in cases with previous antibiotic treatment and most likely to be positive in the presence of liver disease or vital sign abnormalities (systolic blood pressure less than 90 mm Hg, temperature less than 35 degrees Celsius or greater than or equal to 40 degrees Celsius, or pulse greater than 125 per min). Also, bacteremia was most likely to occur with certain laboratory abnormalities (blood urea nitrogen greater than or equal to 30 mg/dL, sodium less than 130 mmol/L, or white blood cell count less than 5,000 or greater then 20,000/mm3). A validation cohort of patients demonstrated the utility of these findings.21
Decision on Hospitalization
The decision to hospitalize a nursing home resident with pneumonia depends on the instructions of advance directives, severity of illness, and the availability of clinical and laboratory resources to the facility. The presence of respiratory distress, hypothermia, hypotension, or renal failure requires transfer to an acute care hospital, unless prohibited by an advance directive. Investigators performing a large retrospective study demonstrated that the 30-day mortality rate for pneumonia acquired in a nursing home (21%) did not appear to be greater for the 280 episodes of pneumonia treated in 11 nursing homes, versus 98 nursing home–acquired episodes subsequently treated in an acute care hospital.However, the hospitalized group was more likely to be severely ill as compared with the group that received treatment within the nursing home.22 A multistate study looking at facility characteristics that play a role in the decision to hospitalize nursing home residents found that nursing homes with more intense medical resources are more likely to manage acute illnesses, such as respiratory infection, within the long-term care facility than to hospitalize the resident. This was especially true for facilities with increased numbers of physicians or physician extenders available to the home.23
The most recent consensus guidelines as to decisions regarding possible transfer of a long-term care facility resident with pneumonia to an acute care hospital emphasize the importance of completing an advance directive early after the patient is admitted to a nursing home. The guidelines indicate that clinical instability, in the face of resident/family decision to aggressively treat the resident, justifies transfer. Similarly, the unavailability of clinical diagnostic testing, necessary treatment modalities, needed frequent monitoring, or infection-control measures in the nursing home are also indications for transfer to an acute care facility.18
Antimicrobial Therapy
The prompt initiation of appropriate antimicrobial therapy is essential to reduce mortality and morbidity risk from NHAP. Although not confirmed for early assessment of oxygenation, the initiation of antibiotics minimally within 8 hours and optimally within 4 hours of presentation to the hospital, and blood cultures obtained prior to initiating antibiotics, have been conclusively shown to reduce 30-day mortality for a large population of Medicare patients admitted to a hospital for CAP. Twenty-three percent of these patients acquired pneumonia in a nursing home.24 Close attention to treating underlying diseases, improving nutrition, correcting any fluid and electrolyte imbalance, providing respiratory support, and avoiding narcotics and sedative medications is a cornerstone of treatment. Geriatricians have known for years that mobility should be encouraged. Early and progressive mobilization was shown recently to reduce hospital stay for CAP in moderately ill geriatric patients. Length of stay was reduced by 1.1 days in 458 patients participating in this randomized clinical trial.25
Specific recommendations for antimicrobial therapy are based on what we know about the etiology of NHAP. For residents in whom the decision has been made to treat within the long-term care setting, an oral or intravenous “respiratory” fluoroquinolone may be utilized. These drugs include levofloxacin, moxifloxacin, and gemifloxacin. Gemifloxacin is available only in an oral formulation. Additional antibiotic choices could include oral amoxicillin-clavulanate, which is an excellent drug for NHAP unless atypical agents such as Legionella or Chlamydia are suspected. Oral cephalosporins (eg, cefpodoxime, cefprozil) could also be considered, but like amoxicillin-clavulanate, have little activity against atypical agents. A parenteral third-generation cephalosporin, such as ceftriaxone or cefotaxime, is also an appropriate drug class to treat NHAP. Ceftriaxone has the advantage of single-daily dosing. Macrolides (azithromycin, erythromycin) may also be considered. Clindamycin and metronidazole may be added to any of the above regimens to improve coverage of anaerobes, and vancomyin or linezolid should be added if methicillin-resistant S. aureus (MRSA) is the causative agent. Table II summarizes these recommendations.
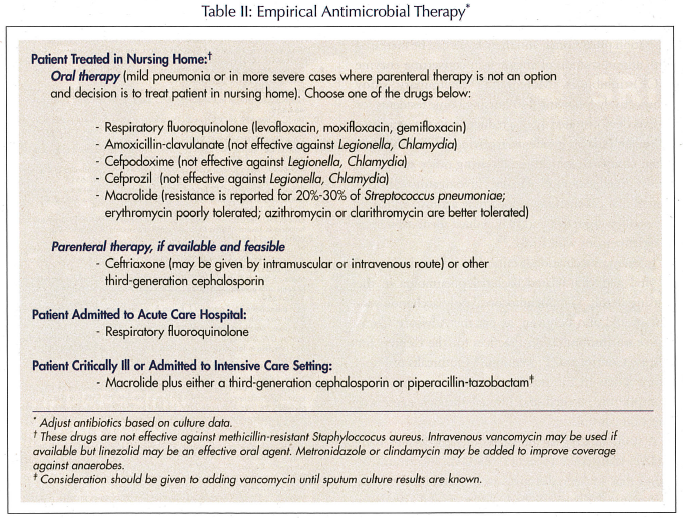
Patients who are transferred to the acute care setting should be treated with a respiratory quinolone. Expanded coverage should be given for critically ill residents, and such residents could be treated with a macrolide plus a third-generation cephalosporin or macrolide plus piperacillin-tazobactam. Additionally, vancomycin should be added until cultures eliminate the possibility of MRSA.
Antimicrobial therapy should always be adjusted when culture data become available. While the duration of antibiotic therapy should be 10-14 days, some patients may require more prolonged antibiotic coverage.
Prevention Strategies
Strategies to prevent pneumonia in the nursing home population include preventing malnutrition, avoiding tube feeding whenever possible, feeding in the upright position, treating underlying diseases, and avoiding the use of sedating medications.26 Selected residents with swallowing disorders should be evaluated with videofluorography, and residents with feeding tubes should be fed in the upright position. A recent study looking at a subpopulation of elderly persons at high risk for aspiration pneumonia demonstrated that a bolus of water given at a high or low temperature accelerated triggering of the swallowing reflex, when compared with water given at room temperature; this suggests that serving meals as soon as they are cooked may be beneficial.27
Another nursing home study, following an earlier study which showed that oral care reduced the risk of pneumonia, demonstrated that after 1 month, cough reflex sensitivity to citric acid significantly increased when compared with controls. The experimental group received gingival and teeth cleaning after every meal by their caregivers.28,29 The earlier study demonstrated that the relative risk for pneumonia in the non-oral care control group was 2.5 times greater when compared with the group of nursing home residents who received oral care. Moreover, the residents receiving oral care had one-half the number of febrile days when compared with controls.29 Unfortunately, a review of interventions to prevent aspiration pneumonia in older adults found insufficient data from randomized, controlled trials to make definitive conclusions on the effectiveness of certain prevention modalities (eg, dietary interventions, positioning, types of feeding tubes).30
While more studies are clearly needed, in recent years there has been progress by investigators in establishing the role of substance P in aspiration.31 Substance P serum levels are depressed in persons with aspiration pneumonia, and these levels can be increased with administration of angiotensin-converting enzyme (ACE) inhibitors. Moreover, a preliminary study prospectively following 440 nursing home residents for 2 years demonstrated a 50% reduction in the incidence of pneumonia in residents receiving ACE inhibitors when compared with those receiving other antihypertensive medications.32 Finally, investigators demonstrated that cabergoline, a dopamine agonist, enhances the swallowing reflex and may reduce silent aspiration in older persons with stroke.33
Influenza vaccination is critical to reduce the impact of viral and viral-related bacterial pneumonia in the nursing home. The pneumococcal polysaccharide vaccine should also be given, as per the Advisory Committee on Immunization Practices for the Centers for Disease Control and Prevention.34 Outbreaks of respiratory illness in the nursing home setting should be promptly investigated and limited through aggressive infection control.
A study looking at the charts of 528 persons with NHAP transferred to acute hospitals for treatment found that advance directives were present only 6.4% of the time.35 Given the high 1-year mortality rate for NHAP, clinicians caring for nursing home residents should make it a priority to ensure that advance directives are in place. These should be readily available to help with the decision on whether or not the resident should be transferred to a hospital, and must also accompany the patient to the acute care facility.









