Patient Safety Culture: A Review of the Nursing Home Literature and Recommendations for Practice
Introduction
The Institute of Medicine (IOM) report, “Crossing the Quality Chasm: A New Health System for the 21st Century,”1 suggested that the biggest challenge to moving toward a safer healthcare system is changing the patient safety culture from one in which individuals are blamed for errors to one in which errors are treated as opportunities to improve the system and prevent harm. Patient safety culture (PSC) has been defined as how the perceptions, behaviors, and competencies of individuals and groups determine an organization’s commitment, style, and proficiency in safety management.2 A variety of instruments have been developed to assess PSC in various clinical care settings.3-5 Acute and ambulatory care centers have also begun to compile PSC benchmarking data.3,4 However, nursing homes lag behind in developing and implementing PSC measures and establishing benchmarking data.6-8
In nursing homes, the collective attitudes, beliefs, values, and behaviors of the nursing home staff and related individuals (visitors, ombudsmen, regulators, and others) may influence patient safety and, hence, PSC. Failure to identify weaknesses in communication, error reporting, teamwork, staffing, and other care processes may lead to safety system defects. These defects may cause failures resulting in accidents or injuries if unchecked. It has been suggested that measurement of PSC could guide nursing home medical directors and administrators in identifying potential systems gaps and in directing a plan for improving safety throughout the nursing home.9 Understanding how PSC impacts clinical and workforce outcomes will be valuable to anyone practicing in nursing homes. This article reviews the literature on nursing home PSC, the measurement of PSC, and offers recommendations to medical directors and providers for evaluating this important aspect of nursing home care delivery.
The Need for PSC Measurement in Nursing Homes
The distinct study of PSC in nursing homes is important for several reasons. Frail elders represent a vulnerable population at high risk for medical errors due to cognitive and sensory impairments. Individuals over age 85 years are the fastest growing segment of the U.S. senior population,10 and most will spend at least some time in a nursing home. Studies have shown that adverse drug events (ADEs) are common in nursing homes,11-13 with rates as frequent as 9.8 ADEs per 100 resident-months, and 4.1 preventable ADEs per 100 resident-months.13 Multiple medications, multiple disease processes, and nonspecific presentation of illness all increase the risk of medical error in the nursing home population.
In addition to unique aspects of this population, the structure of the nursing model of care is considerably different from that in acute care or outpatient institutions. Most direct care in nursing homes is provided by certified nursing assistants (CNAs),14 guided by licensed practical nurses (LPNs) and/or registered nurses (RNs). Physicians often are not on site,15,16 so communication regarding change of condition or changes in medications is often accomplished via telephone. This suggests significant differences in the systems of care in nursing homes, different potential underlying causative factors and solutions to patient safety issues, and possibly a different underlying safety culture.
Nursing homes are driven in part by a punitive regulatory environment, governed by regulations from the Centers for Medicare & Medicaid Services (CMS), and each state’s Department of Public Health.17 By comparison, hospitals are primarily driven by an accreditation process through the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO). Certain principles of PSC that apply to other industries or to hospitals, such as a fair and just culture versus a culture of blame, may not resonate with nursing homes as they are currently structured. The need to develop nursing home–specific instruments to measure PSC—particularly to address the views of CNAs—has been raised by a number of researchers.4,7,18
Finally, studies in hospitals suggest that PSC may be related to outcomes such as reduced length of stay, nursing turnover, and medication errors.19 Research also suggests that there is an association between PSC attitudes, staff behaviors, and resident outcomes such as falls, medication errors, and pressure ulcers.20-22
Instruments Used to Assess PSC in Nursing Homes
To date, a standard methodology for studying PSC in all healthcare settings has not been identified. There is considerable overlap in the dimensions of PSC measured in various instruments; however, there are also important differences.23 Several recent reviews of PSC instruments have concluded that there is a need to develop standard dimensions of PSC23-25 since it is possible that, to date, important dimensions could have been omitted and relatively less important dimensions included.26 The Hospital Survey of Patient Safety Culture (HSOPSC) is the only instrument that has been used in more than one nursing home study; therefore, we review it in some detail below.
The Hospital Survey of Patient Safety Culture
 The HSOPSC, funded by the Agency for Healthcare Research and Quality (AHRQ), was developed and piloted in 2003.4,27 The original instrument included 12 specific dimensions and two outcome measures (Table I). Each dimension has 3-5 items. A 5-point Likert scale (1-5) measures “strongly disagree” to “strongly agree,” or “never” to “always.” The outcome measures are single-item responses about the number of “events” reported in the past 12 months (defined as errors of any type, regardless of whether they result in patient harm) and the overall patient safety grade (“excellent” to “failing”). Higher scores indicate more positive attitudes toward patient safety culture. A report detailing the development of the instrument and initial psychometric testing is available online.4 Initial testing was done in 21 hospitals across six states. A total of 1437 hospital employees out of 4983 potential respondents completed the survey for a response rate of 29%. Current benchmark data consist of 108,621 hospital employees from 382 hospitals across the United States as of 2006.28
The HSOPSC, funded by the Agency for Healthcare Research and Quality (AHRQ), was developed and piloted in 2003.4,27 The original instrument included 12 specific dimensions and two outcome measures (Table I). Each dimension has 3-5 items. A 5-point Likert scale (1-5) measures “strongly disagree” to “strongly agree,” or “never” to “always.” The outcome measures are single-item responses about the number of “events” reported in the past 12 months (defined as errors of any type, regardless of whether they result in patient harm) and the overall patient safety grade (“excellent” to “failing”). Higher scores indicate more positive attitudes toward patient safety culture. A report detailing the development of the instrument and initial psychometric testing is available online.4 Initial testing was done in 21 hospitals across six states. A total of 1437 hospital employees out of 4983 potential respondents completed the survey for a response rate of 29%. Current benchmark data consist of 108,621 hospital employees from 382 hospitals across the United States as of 2006.28
Potential issues exist with the validity of PSC instruments in new populations and settings. Researchers adapting the HSOPSC for other settings or populations, such as nursing homes, have tried to optimize comparability and the potential for benchmarking by keeping the revised instruments as close to the original as possible.9 To ensure validity in the nursing home setting, AHRQ is currently assessing PSC in 40 nursing homes across the United States to develop nursing home–specific benchmarks.
Nursing Home PSC Studies
A search was conducted in MEDLINE, Ovid, Cumulative Index of Nursing and Allied Health Literature (CINAHL), PsychINFO, and Health and Psychosocial Instrument for articles published in the English language between January 1, 2003, and November 1, 2007. Search terms used were climate of safety, culture of safety, patient safety culture, nursing home, long-term care, organizational culture. Variables of interest included medical error reporting, transitions across healthcare settings, quality improvement programs, and staff retention.
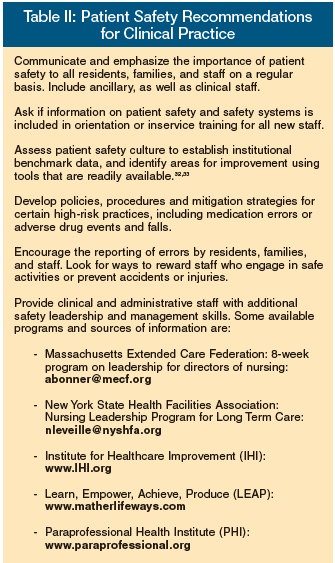
A total of six studies were identified that examined PSC in nursing homes.7-9,18,29,30 These six studies focused on nurses and CNAs, CNAs exclusively, administrators, providers (physicians, nurses, nurse practitioners, pharmacists), and nurses and nursing leadership. These studies are briefly reviewed below, with some key points featured in Table II.
Nurse Aides’ Ratings of the Resident Safety Culture in Nursing Homes
 Castle7 conducted a PSC survey in five randomly selected states: New York, Oregon, Michigan, Colorado, and Florida. The purpose was to: (1) compare CNA PSC survey scores with hospital benchmark PSC scores; and (2) to see how nursing home PSC varied by certain facility-level and market characteristics such as bed size, profit or chain status, or average occupancy. Out of 240 randomly selected participating homes, 72 agreed to participate, for an overall nursing home response rate of 30%. In those 72 homes, 1579 CNAs out of 2872 completed the survey, for a 55% response rate.
Castle7 conducted a PSC survey in five randomly selected states: New York, Oregon, Michigan, Colorado, and Florida. The purpose was to: (1) compare CNA PSC survey scores with hospital benchmark PSC scores; and (2) to see how nursing home PSC varied by certain facility-level and market characteristics such as bed size, profit or chain status, or average occupancy. Out of 240 randomly selected participating homes, 72 agreed to participate, for an overall nursing home response rate of 30%. In those 72 homes, 1579 CNAs out of 2872 completed the survey, for a 55% response rate.
Results suggested that certain facility characteristics were associated with higher CNA PSC scores. In almost all dimensions, PSC ratings for nursing homes were lower than for hospitals. The author concludes that significant issues related to nursing home PSC exist, and that further research is warranted.
The role of the CNA in nursing homes is critical, because CNAs provide the vast majority of direct resident care. Accurately measuring CNA PSC is likely to be important in assessing differences in safety and quality outcomes across nursing homes. A current study is being conducted by the authors to examine the relationship between CNA PSC and clinical and workforce outcomes.
Nurses’ and Nursing Assistants’ Perceptions of Patient Safety Culture in Nursing Homes
Hughes and Lapane18 report on PSC in a sample of nurses and nurse’s aides in 26 Ohio nursing homes. Fifty percent of staff reported discussions with management to prevent mistakes, suggesting a positive safety culture. However, two out of five study participants report that error reporting is seen as a “personal attack,” and 20% report feeling “punished” for making errors.
Results of this study suggest that an open environment around error reporting does not exist in nursing homes. Given the punitive nature of the state survey process, this is not surprising. Efforts to reconcile enforcement of regulation with encouragement of open communication and error reporting in nursing homes is warranted.
Patient Safety Culture Assessment in the Nursing Home
Handler et al9 conducted a study assessing the PSC of pharmacists, physicians, nurse practitioners, and nurses in four nursing homes in southwestern Pennsylvania. In this study, healthcare professionals agreed on 11 of 12 dimensions and differed significantly (P < 0.05) only in ratings for one PSC dimension (attitudes about staffing issues), where nurses and pharmacists believed that they had enough employees to handle the workload. Nursing homes scored significantly lower (ie, worse) than hospitals (P < 0.05) in five PSC dimensions (nonpunitive response to error, teamwork within units, communication openness, feedback and communication about error, and organizational learning). Nursing homes differed from hospitals, especially in perceived response to error, which was reported as more punitive in the nursing home. These findings were not unexpected, because error-reporting policies and processes are thought to perpetuate a punitive environment in nursing homes.31
Assessment of Safety Attitudes in a Skilled Nursing Facility
Wisniewski et al30 studied job categories that included nurses and CNAs, as well as some non-nursing staff (social workers, therapists, unit clerks) in an exploratory study using the Safety Attitudes Questionnaire (SAQ) in one nursing home in New York State. The response rate was 18%; since it was only 13% for CNAs, generalizability is limited. Physicians and nurse practitioners were not included. The construct “perceptions of management” had the lowest mean score. Analyses revealed that increased staffing might have an impact on this staff perception. Consistent with other studies,18,29 uneasiness with discussion and reporting of errors were identified. The SAQ has several elements related to job satisfaction as well as PSC, and may be useful in assessing both concepts in one survey. Further work in larger studies is indicated by the preliminary results.
Moving from a Culture of Blame to a Culture of Safety in the Nursing Home Setting
Scott-Cawiezell et al29 studied PSC in a single nursing home using a mixed methods approach, including the Shortell organization and management survey. They also used a case study approach to the quality improvement (QI) process around medication safety. The job class of specific team members included in the design was not reported. Despite on-site research staff support, and the presence of a supportive administrator, a culture of blame with respect to medication errors persisted. The researchers identified limited resources, overwhelmed leadership, and an educationally diverse workforce as barriers to improved PSC. This study highlighted the importance of leadership, communication, and relationships among coworkers and managers in optimizing patient safety processes and outcomes.
A Culture of Patient Safety in Nursing Homes
Castle and Sonon8 asked administrators to complete the HSOPSC. 2840 nursing homes out of 4000 responded to a mailed survey, for a response rate of 71%.8 Scores were lower than hospital benchmarks in almost all categories. Large differences existed between the organizational learning climate in hospitals and nursing homes. Responses to statements such as “we are actively working to improve resident safety, we see positive changes as a result of a mistake, we evaluate effectiveness after implementing change” were considerably lower when answered by nursing home administrators. These results support previous studies showing administrative staff have higher overall perceptions of safety culture than direct-care staff,26 and should be of concern to individuals working in nursing homes.
Summary and Implications for Future Research
Nursing home PSC studies have examined the attitudes of nurse’s aides, nurses, providers, pharmacists, and administrators. But no single study has included all job categories, as well as ancillary staff. Facility PSC measurement should include not only clinical staff but housekeepers, dietary staff, maintenance workers, social services, and others. To date, studies have not included families, ombudsmen, other visitors, and most of all, residents. Determining whether there are differences in the views of state surveyors or other regulators versus nursing home staff would provide an opportunity to identify areas of conflict. The punitive approach of Departments of Public Health may be limiting nursing homes’ ability to develop or enhance PSC.
Studies from nursing homes reviewed in this article suggest that PSC can be measured, although researchers still disagree about the most accurate way to do this. Surveys that measure PSC may include different sub-domains, and opportunities to improve conceptual clarity around safety climate and culture exist. More work needs to be done to determine whether adapting existing surveys will be reliable and valid in new settings, such as nursing home or ambulatory care settings. There is also a need to determine whether an association between patient safety culture and clinical outcomes exists.
Research currently being conducted by the authors has begun to show that a relationship exists between nursing home staff PSC scores and clinical or workforce outcomes. Consequently, measurement of PSC in nursing homes may provide a feasible method for assessing important safety constructs such as communication, staffing, supervision, error reporting, learning environment, and handoffs. Providing nursing home leaders with the skills and tools to impact those areas may lead to improved patient safety outcomes and lower staff turnover. Future work will address the gap that exists in our understanding of PSC among nursing home CNAs, nurses, administrators, providers, and other staff. Understanding and measuring the PSC of frontline workers and leadership are critical, both for U.S. policy and for best practices to address patient safety in America’s nursing homes.
Dr. Perera has received research grants from Eli Lilly and Company and Ortho Biotech. The other authors report no relevant financial relationships.
Acknowledgments
This study was supported in part by an American Medical Directors Association Foundation/Pfizer Quality Improvement Award, NIH grants 1 KL2 RR024154-01 (NIH Roadmap Multidisciplinary Clinical Research Career Development Award Grant), and a Merck/AFAR Junior Investigator Award in Geriatric Clinical Pharmacology.










