Medicare Medication Management: Updating Issues with Parts A, B, C, and D
Presidential election aside, medication management under Medicare promises to see some major changes that will affect access to medications in the coming year. This at a time—or perhaps because we are in a time—of increasing demand for access to innovative medications by an ever-expanding group of Medicare beneficiaries.
In a question-and-answer format, this article will highlight the major areas of change that are occurring to medication management within all parts of the Medicare program:
• Medicare Part A, which covers hospitalization, subacute services, and hospice
• Medicare Part B, which covers provider services and a few vaccinations
• Medicare Part C, or the Medicare Advantage managed care program • Medicare Part D, the outpatient medication benefit
All aspects of the Medicare program affect medication management, especially for injectible medications.
Medicare Part A: Hospital Insurance
Q: How will changes in hospital reimbursement affect prescribing?
A: After more than 40 years of paying for preventable mistakes, Medicare is ceasing the practice. As a result, hospitals will no longer be paid for mistakes that occur during a hospitalization. This is but the first step; Medicare is closely looking at penalizing hospitals for readmissions that occur within 30 days of a hospitalization for the same diagnosis or a complication of the original diagnosis. This change in reimbursement of holding hospitals accountable is already having an effect on some providers and will likely have far-reaching effects in the near future.
Cardinal Health, Inc., one of the nation’s top drug wholesalers, expects its newer hospital supply and equipment businesses to grow faster as a result of Medicare tightening rules for no longer paying for “preventable” conditions, mistakes, and infections resulting from a hospital stay.1 The majority of that growth will come from technologies for hospital automation systems for medicine and supplies. Even more important from a long-term care perspective is the expectation that hospitals will be forced to take a closer look at transitions of care. Medicare is deeply concerned, as pointed out in reports from MedPAC, about the readmissions that are common among Medicare beneficiaries within a 30-day timeframe. As mentioned above, hospitals may be penalized for readmissions that occur for the same diagnosis or complication of the original admitting diagnosis. This is likely to result in hospitals playing a more critical role in assuring that patients have access and understand their discharge medications. Compliance with the discharge plan, or rather lack of compliance, is often a cause for readmissions. This increased attention is likely to result in improvement in medication management at the time of discharge.
Q: What medication carve-outs exist within Medicare Part A?
A: While many believe that during a Medicare Part A stay all medications are included in the payment for that stay, there are exceptions. As in the case of hospice, Medicare Part A stays only include responsibility for medications that are related to that stay. The most significant outlier during a Medicare Part A stay are vaccinations. Vaccines that are rendered during a Medicare Part A stay are covered under the Medicare Part D or Part B program. Medicare Part B will continue to cover pneumococcal, influenza, and hepatitis B, while Medicare Part D will cover all other vaccines, including not only the medication but also the administration cost. Given the public health promotion of vaccines, it makes sense that the financial disincentive to provide vaccines during a Medicare Part A stay should not exist.
Medicare Part B: Medical Insurance
Q: What incentives exist for the over- and underutilization of traditional Part B medications?
A: Within the area of medications available under Medicare Part B, the majority of which are oncology medications, several studies have demonstrated higher utilization associated with incentives for profitability from their use. This was demonstrated most recently in a study examining the use of erythropoiesis-stimulating agents (ESAs) in for-profit versus not-for-profit dialysis centers. With this in mind, Medicare is examining several tools to limit this incentive, thus resulting in a projected decrease in the use of these medications. These levers include further decreases in physician reimbursement for medications, further encouragement of physicians into the Competitive Acquisition Program (a program where physicians receive medications with a prescription from a specialty pharmacy rather than purchasing it themselves), and further movement of Medicare Part B medications to Medicare Part D, as was just done with all the vaccines except for pneumococcal, influenza, and hepatitis B. In addition, not only are the ingredient costs for the vaccines covered under Medicare Part D as of January 1, 2008, but the administration fee as well. (See “Medicare Part B’s BIG Changes” in the June 2007 issue of Annals of Long-Term Care.)
Q: Where are we headed regarding access to medications through Medicare? What tools are the CMS and the FDA utilizing to assure appropriate medication use?
A: Most of Medicare’s focus on controlling costs for medications is on the Medicare Part B program. That is because Medicare Part D is provided through private plans that reserve a defined amount of money from Medicare for covering prescription drugs—overutilization in the Medicare Part D program becomes the liability of the Part D plans. Not so in Medicare Part B, where Medicare is responsible for all overutilization of these increasingly costly and utilized medications. To control these costs, Medicare is increasing regulation through such devices as globally capitating providers for services that include medications such as dialysis, forcing the use of RiskMaps and Coverage with Evidence Determination to control utilization, and requiring specific genetic testing to assure that patients who would not benefit from medication protocols are not placed unnecessarily on that course of therapy.
Medicare Part C: Medicare Advantage
Q: What type of plans have expanded most within Medicare Part C and why?
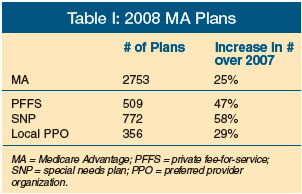 A: For 2008, Medicare has seen a significant increase in the number of managed care plans (Table I), especially in the area of special needs plans (SNPs), where the growth of new plans is estimated at 58%. Some unique plans have been developed in 2008 under these programs; most unusual is the development by Evercare of an Alzheimer’s dementia SNP set to begin enrollment in Arizona. The increase in the number of Medicare Advantage plans (MA-PD) for 2008 will likely continue to extend the growth of enrollment in these programs, which have already seen a significant increase from enrollment levels of 5.8 million in 2005, 6.04 million in 2006, and 6.7 million in 2007. It is worthwhile to note that Medicare Advantage plans act differently from stand-alone prescription drug plans in their offering of lower premiums, which are approximately $11 per month, as well as medication coverage during the donut hole, which is 20% more than those offered by prescription drug plans.
A: For 2008, Medicare has seen a significant increase in the number of managed care plans (Table I), especially in the area of special needs plans (SNPs), where the growth of new plans is estimated at 58%. Some unique plans have been developed in 2008 under these programs; most unusual is the development by Evercare of an Alzheimer’s dementia SNP set to begin enrollment in Arizona. The increase in the number of Medicare Advantage plans (MA-PD) for 2008 will likely continue to extend the growth of enrollment in these programs, which have already seen a significant increase from enrollment levels of 5.8 million in 2005, 6.04 million in 2006, and 6.7 million in 2007. It is worthwhile to note that Medicare Advantage plans act differently from stand-alone prescription drug plans in their offering of lower premiums, which are approximately $11 per month, as well as medication coverage during the donut hole, which is 20% more than those offered by prescription drug plans.
Medicare Part D: Prescription Drug Coverage
Q: What regulatory changes are impacting medication access through Medicare Part D for 2008?
A: The major change for 2008 Medicare Part D formularies is the elimination of the requirement for one drug in a formulary key drug type (FKDT). In the first two years of the program, plans that followed the United States Pharmacopeia Model Guidelines were required to cover two medications in classes and categories and one in a FKDT. The classes most affected by this restriction in access to medications are the antibacterial agents, cardiovascular agents, and medications for the treatment of diabetes and Parkinson’s disease.
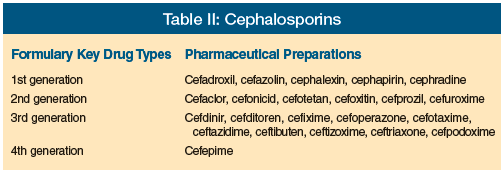
If one examines the antibacterial category, it is noted that a move eliminating the requirement of coverage in each FKDT means that plans could move from covering a drug in each of the generations to only providing coverage for two 1st-generation cephalosporins. This would mean that a 2nd-, 3rd-, or 4th-generation cephalosporin would require an appeal to gain access (Table II).
Q: What is the most likely impact of the PQRI on prescribing habits? Where is Medicare pushing prescribing through its quality initiatives?
A: Medicare through pay-for-performance initiatives has established several programs that rely heavily on medication management. For the Physician Quality Reporting Initiatives (PQRI), many of the 74 measures currently available to physicians require medication management. For example, the three measures for diabetes look to achieve low-density lipoprotein of less than 100, HbA1c of less than 9.0, and blood pressure of less than 140/90 mm Hg. It becomes clear that these measures are achievable only if physicians, with pharmacists and other practitioners, are able to communicate the importance of adherence, as well as assure access to the medications necessary to achieve these outcomes.
Q: Where is medication therapy management going?
A: Under Medicare Part D, these services are provided through plans under their medication therapy management (MTM) programs, as such a plan must provide the service internally or contract with qualified providers for the services. MTM programs are services targeting those seniors taking multiple medications with costs of over $4000 annually to treat multiple chronic illnesses. The $4000 financial threshold for medications used annually remains the same for 2008. CMS believes strongly that MTM will evolve, becoming a cornerstone of the Medicare Prescription Drug Benefit.
The stated objective of CMS in developing MTM is to assure that prescribed Medicare Part D medications are appropriately used to optimize therapeutic outcomes through improved medication use, as well as reduce the risk of adverse events, including adverse drug interactions for targeted beneficiaries. CMS believes that MTM should include enhanced enrollee understanding through beneficiary education counseling and other means that promote the appropriate use of medications, and reduce the risk of potentially adverse events associated with the use of medications. Another component could be increased enrollee adherence to prescription medication regimens (eg, through medication refill reminders, special packaging, compliance programs, and other appropriate means). MTM could also include detection of adverse drug events and patterns of overuse and underuse of prescription drugs to assure that the appropriate medications are prescribed.
Q: What effect will ePrescribing have on outcomes?
A: ePrescribing (the process of writing and transmitting prescriptions electronically) is likely to have a major effect on which medications are prescribed to patients, as decision making at the point of prescribing can be better informed. Legislative efforts are likely within the next year to promote electronic health records and national health data standards. ePrescribing has been promoted to reduce preventable medication errors, which have been estimated by the Institute of Medicine to affect 1.5 million Americans per year. Currently, fewer than one in five MDs uses ePrescribing.
A communication and knowledge gap exists between seniors and their physicians regarding prescription medications.2 When initiating new medications, it has been demonstrated that physicians often fail to communicate critical information,3 and ePrescribing may benefit this process. Having ePrescribing resources with embedded evidence-based guidelines, such as the Beers Criteria, available at the time of prescribing have the potential to reduce this gap.
What’s Next for Medicare Medication Management?
The exact answer to “What’s Next?” will have to await the result of the 2008 elections, but one thing is certain: CMS, despite recent advances into areas of quality concerns, is likely to slide back to its old focus as the Health Care Financing Administration, where the concentration was on paying bills. In that capacity, Medicare is likely to increasingly shift costs to seniors in an effort to reduce utilization as well as their share of the cost for covered services. How extensive this shift will be remains to be seen; but clearly, in order for Medicare to continue to provide comprehensive coverage for a growing number of seniors, cuts in both medication utilization and Medicare’s share of the costs must occur to decrease total expenses to the level that Medicare can afford. Stay tuned, for while the questions may stay the same, the answers may be very different as politicians, providers, and patients demand changes.
Please send any questions or experiences about Medicare you would like to share with readers to: bspivack@lifecare.com









