Discrepancies in Diagnosis of Deep Venous Thrombosis Using Portable Technology in a Skilled Nursing Facility and an Acute Hospital-Based System
We report three cases of Doppler ultrasound discrepancies between portable diagnostic unit and hospital-based units among skilled nursing facility residents.
Case 1
Mrs. HK is an 81-year-old female resident of a skilled nursing facility (SNF). Her medical history includes coronary artery disease (CAD), hypertension, and a right humeral neck fracture and left radial fracture 6 weeks earlier. She complained of pain and swelling of her right upper extremity (RUE). An order for an upper extremity portable Doppler ultrasound (US) was placed. This study, as well as all studies in the SNF, were done with portable equipment at the bedside. The study was read by a radiologist as compatible with a RUE deep vein thrombosis (DVT). The patient was transferred the same day to the closest acute care hospital, and a repeat US of RUE was read with no evidence for a DVT.
Case 2
Mrs. MJ, an 81-year-old female SNF resident with a history of hypertension, anemia, and congestive heart failure (CHF), was noted to have new onset of lower-extremity (LE) edema. A portable US was reported positive for a DVT in the right common femoral vein. The patient was transported to the hospital, where a Doppler US on the same found no evidence for a DVT in either extremity.
Case 3
Mrs. AM, a 91-year-old female SNF resident with a history of atrial fibrillation, CHF, right hip fracture (status post open reduction internal fixation) 1 month previously, taking enoxaparin, complained of pain and swelling of her right leg. A portable US was reported as consistent with a thrombus in the common femoral vein. When a repeat US was done the next day at the acute care hospital, there was no evidence for a DVT. At this point, the medical director was notified and an investigation started.
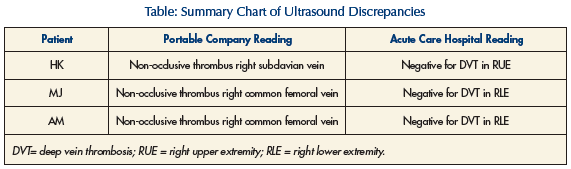
In each of the three cases, either the patient did not receive new anticoagulation or no change in present anticoagulation therapy was made (Table). No further clinical adverse reactions were noted.
Deep vein thromboses are very common in both acute care hospitals and SNFs, with prevalence from 5-20%.1 Risk factors include malignancy, advanced age, history of thromboembolism, and post-surgical conditions that are common in a SNF population. For all these reasons, the medical staff must have a high index of suspicion for this common and potentially life-threatening disease.2,3
The SNF in this vignette is a not-for-profit, religiously affiliated facility that is part of a Continuing Care Retirement Community in suburban Philadelphia. All of the patients were short-stay residents admitted to the facility for acute rehabilitation after a hospitalization for an acute illness. The mobile ultrasound company is a division of a larger mobile x-ray company that had been serving the SNF and multiple other nursing facilities in Philadelphia and the surrounding area for many years. The mobile studies were read and reported in writing by board-certified radiologists. It should be noted that the studies were performed by different technicians and were read by different radiologists in the portable ultrasound company and the acute care hospital.
The acute care hospital is an academic university-affiliated, 570-bed, not-for-profit hospital in suburban Philadelphia less than one mile from the nursing facility. The second ultrasound was ordered while the patients were in the emergency room and was read by board-certified radiologists.
Discussion
These cases present a potentially serious problem for patients and staff at long-term care facilities. With insurance changes and stricter regulations for acute rehabilitation hospitals, the trend for patients to be admitted to a SNF for rehabilitation after hip and knee surgeries, cerebrovascular accidents, gait dysfunction, falls, and brain injuries is increasing.4,5
Patients in SNFs are at a high risk for a LE DVT which, if dislodged, might result in pulmonary embolism.6 An upper-extremity DVT also carries significant morbidity. None of our patients had pulmonary embolism by clinical data and are doing well at present with no change in treatment. It is well documented that physical exam is not very sensitive or specific for the presence of a DVT.7,8 In addition, unlike an acute care facility, physician staff is not always present at a SNF. Doppler ultrasound is considered a usable standard for the diagnosis of DVT. Some studies have reported a sensitivity of 70-80% and specificity of 95-100% for diagnosing DVT by US.9,10 No prospective studies could be found in medical literature comparing the rates of DVT diagnosis by portable ultrasound and ultrasound machines used in the hospital setting. Retrospective studies have reported a negative predictive value of 98% with portable ultrasound11,12 for DVT diagnosis. With the development of low-weight products, intravenous heparin therapy is not always indicated. There is a trend towards not hospitalizing patients with a newly diagnosed DVT and treating patients in the SNF with weight-adjusted, intramuscular, low-molecular-weight heparin (eg, enoxaparin) until they are therapeutic on warfarin.13,14 The physicians caring for these patients all decided to hospitalize the patients for a variety of reasons rather than having the patients remain at the SNF. The patients were all new to the facility, were not primary patients of the physician prior to their admission, and had all had recent acute illnesses or surgeries. The physicians felt that for these cases, further evaluation in an emergency room with possible subsequent admission was a better treatment plan. Had the physicians and staff not chosen hospitalization, it is most likely that these patients would have been treated for months with anticoagulation, putting them at risk for all the possible complications of this, such as bleeding, bruising, drug interactions, warfarin necrosis, and possibly death.
These cases represent a warning for possible inaccuracies in portable ultrasound techniques and reading that should serve as a warning to long-term care facility medical and nursing staff and medical directors. Unfortunately, it remains unclear why these discrepancies occurred, despite a thorough investigation by the ultrasound company and a medical staff meeting at the nursing home to review the films and technique. It is possible that the clot could have been dislodged in the short time interval between the initial and repeat ultrasounds. However, this seems unlikely as none of the patients had any signs or symptoms consistent with pulmonary embolism.
Nursing facilities should consider a Quality Assessment program, including an audit of charts to compare portable and non-portable x-rays and ultrasounds if both are done. Communication between the medical director and the ultrasound company should be initiated with periodic follow-up. Any history of discrepancies between portable and non-portable studies should be examined and, if present, prompt an evaluation of the qualifications and skills of the technicians and radiologists. An ideal solution would be to digitize and make available all portable x-rays and ultrasounds at a secure site on the Internet, where qualified personnel, including attending physicians, could have access to the actual films.
With more acutely ill patients being transferred to a SNF, and the increasing use of low-molecular-weight heparin products in facilities for treatments of acute DVT, the reliability and accuracy of portable Doppler ultrasound studies becomes more critical in preventing medical errors and unnecessary morbidities and mortality. Since attending physicians in SNFs seldom have a choice of provider for in-house radiological studies, and have little information with which to gauge their reliability, a patient’s plan of care may be dependant on the accuracy of a service over which they have little control. Interdisciplinary team members must carefully evaluate the results of tests ordered and carefully consider risk-benefit before beginning therapy. In cases where the diagnosis is in doubt or the risk of anticoagulation is very high, it may be appropriate to order a confirmatory evaluation with a non-mobile unit.
Medical directors should consider implementation of a Quality Assessment program or audit of studies performed by mobile providers.
The authors report no relevant financial relationships.










