The POLST Paradigm: Respecting the Wishes of Patients and Families
Introduction
Despite the hope that traditional advance directives would ensure that patients’ end-of-life treatment preferences are honored, numerous studies have found that only 20-30 percent of U.S. adults have an advance directive, and that these documents have limited effect on treatment decisions near the end of life.1 Some of the limitations associated with traditional advance directives are that they may not be available when needed, are not transferred with the patient, may not be specific enough, may be overridden by a treating physician, and do not immediately translate into a physician order.
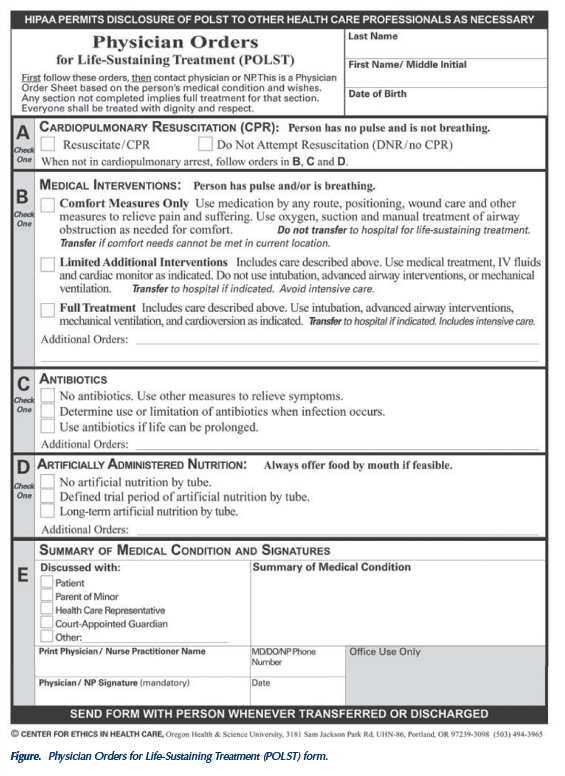
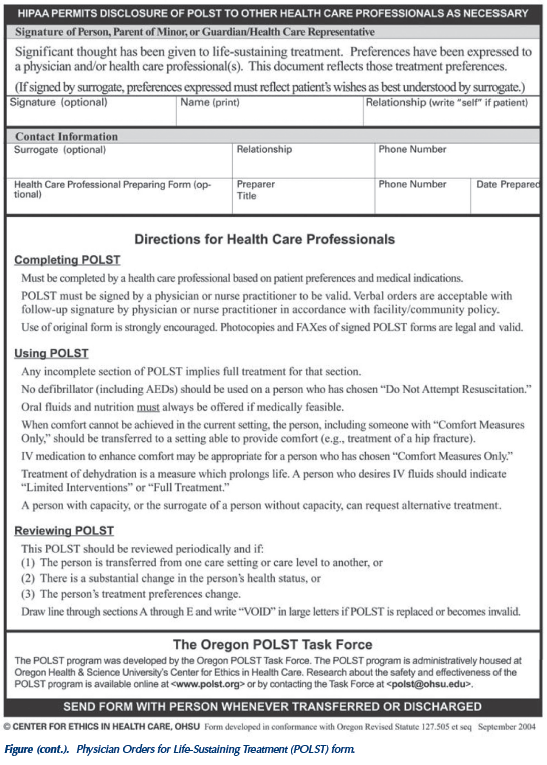
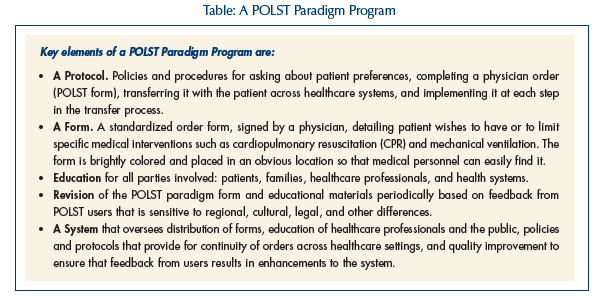
The Physician Orders for Life-Sustaining Treatment (POLST) form and program were originally developed in Oregon in 1991, complementing traditional advance directives, to help ensure that patient wishes to have or limit specific medical treatments are respected near the end of life.2-8 The POLST form is a standardized set of medical orders usually developed by a coalition of citizens, healthcare professionals, healthcare agencies and organizations representing hospice, hospitals, emergency medical services, primary care and long-term care (LTC) professionals, and aging services (Figure). These orders provide guidance to first responders at the time of need, and they transfer with patients throughout the healthcare system serving as portable medical orders.
Programs based on the POLST Paradigm are now implemented throughout or in parts of 15 states. Slight modifications have been made by some states. For example, in West Virginia, the program is called Physician Orders for Scope of Treatment (POST); in New York, it is called Medical Orders for Life Sustaining Treatment (MOLST). The overarching goals are the same. POLST/POST/MOLST orders are intended for persons with advanced chronic illness who wish to turn some aspects of their advance directives or advance care plans into action at the present time to ensure that their medical treatment preferences are respected.
The National Quality Forum recommended use of the POLST program as a preferred practice for quality palliative care, noting that, “Compared with other advance directive programs, POLST more accurately conveys end-of-life preferences and yields higher adherence by medical professionals.”9
This article outlines the elements of a POLST Paradigm Program, describes the current challenge to respect patient treatment preferences at the end of life, and offers a solution and recommendation.10
The Problem
Mrs. J is an elderly woman with advanced dementia who lives in a skilled nursing facility. She previously completed an advance directive requesting “do-not-resuscitate” (DNR) status and no intensive care. She has also completed paperwork appointing her daughter to make medical decisions. One Saturday night she is found unresponsive with an irregular weak pulse and very low blood pressure. Her facility is unable to reach her daughter, and emergency medical services (EMS) is called. The patient has a dysrhythmia, is resuscitated, intubated, and transferred to the nearest hospital. She is admitted to the intensive care unit and placed on a ventilator. The next morning, Mrs. J’s daughter learns what has happened and demands to know why the nursing home orders were not followed.
Why did this happen? Completing an advance directive or living will is often not sufficient to ensure that patients’ wishes to have or to limit medical treatment will be consistently respected. Advance directives are general statements of patients’ preferences but need to be carried out through specifications in medical orders when the need arises. Without special arrangements, medical orders have limited authority outside of the institutions in which they are written. For example, a physician’s orders at the nursing home usually have no authority in the ambulance or at the hospital.
(Continued on next page)
The Solution
Mrs. J needed a document with medical orders that were consistently followed at each step of her care, from the nursing home to the ambulance to the emergency department to the intensive care unit. This is what the POLST Paradigm Program accomplishes. Below, we describe the system components necessary to ensure that Mrs. J receives the care she wanted, and then we return to her case to show how the outcome could have been one that respected her values and preferences.
There is strong evidence that this approach really works.2-9 Patients in Oregon using the POLST form virtually always have their decisions honored, even during transfer to a hospital at the time of a serious complication.3 Patients living with serious chronic illness are advised to have their POLST form with them so that their wishes can be honored when the need arises.
Approach to Implementation of a POLST Paradigm Program in Your State
There is increasing awareness of the POLST Paradigm across the country, and many more states and communities are offering this document to summarize wishes for patients with advanced chronic illnesses and frailty in the form of physician orders. The POLST website at www.polst.org provides contact information and details about the status of POLST implementation in each state. The following steps outline the paths other states have followed to develop and implement a statewide POLST Paradigm Program:
1. Do a Needs Assessment. Is your system working well already to identify and respect patients’ preferences for end-of-life treatments? Are patients who wish to have orders to have or to limit life-sustaining treatments, such as CPR, clearly identified, and are those wishes being consistently respected? Are seriously ill patients who wish to remain at home or in a LTC facility usually able to receive comfort care in those settings, or are they often transported to the hospital? A statewide needs assessment would include surveying EMS, emergency physicians and nurses, and social workers in LTC facilities and hospitals.
2. Assemble a Core Working Group. If your data show problems in respecting patient wishes, you may wish to assemble a core group who believes that the POLST Paradigm is a good idea. By working together, members can enhance their knowledge, explain common goals to others, and enlist their participation. The video, “Your End-of-Life Prescription: Physician Orders for Life Sustaining Treatment (POLST),” describes how to build a coalition and is available on the POLST website.
3. Assemble a Task Force with Broad Representation. A statewide task force should include representatives from EMS, emergency physicians and nurses, LTC association and surveyors, medical association, senior services, department of health, hospital association, home health association, bar association, and hospice association. Other groups may also be considered for inclusion, such as organizations that represent healthcare for seniors, representatives from minority groups, the ethics committee network, and one or more legislative champions who can provide counsel and representation regarding possible legislation. Representatives of the disability community should be considered for membership or consulted as needed to further ensure that the wishes of vulnerable patients are honored.
4. Clarify Who Should Have a POLST. Use of the POLST form is most appropriate for seriously ill persons with a terminal illness. To determine whether a POLST form should be encouraged, clinicians should ask themselves, “Would I be surprised if this person died in the next year?” If the answer is “No, I would not be surprised,” then a POLST form is appropriate. Remember that a POLST form is designed to express the individual’s preferences for levels of treatment, and can indicate either full treatment including resuscitation attempts or can be used to limit those interventions that are not desired by the individual. Unless it is the patient’s preference, use of the POLST form to limit treatment is not appropriate for persons with stable medical or functionally disabling problems who have many years of life expectancy. In the absence of a POLST form or other state-specific DNR orders, patients will receive advanced cardiac life support, including CPR, endotracheal intubation, and defibrillation, by emergency medical personnel based on standard protocols.
5. Conduct a Pilot Project. Consider conducting a voluntary pilot project in one or more communities. Enlist all local LTC facilities, EMS, emergency department personnel, hospitals, home health, and hospice. Provide training for social workers and nurses so they are better able to talk to patients and families about the POLST Paradigm form. You may wish to create a regional task force composed of representatives from these entities and meet monthly to implement the pilot project, and then to review the results and share them with other members of the statewide task force. As your state or community develops a POLST Paradigm Program, the National POLST Paradigm Initiative Task Force is available for consultation. E-mail correspondence can be sent to polst@ohsu.edu. Once a local contact person has been identified, the task force can provide you with research and legal developments in other states, and connect you with others in your state by listing information about your state on the www.polst.org website.
6. Address Legal Issues. State laws vary and impact the process of implementation. Under your state law, can a POLST Paradigm Program be developed by state regulations, or will it require legislation? Some states have chosen the legislative route (West Virginia, Tennessee, and Hawaii) while others have followed the regulatory route (Oregon, Washington, and Utah). Consider whether you want to have the POLST Paradigm form signed by a physician only, with the patient/legal agent’s signature optional (as is the case in Oregon) or if you want the patient/legal agent’s signature mandatory (as is the case in West Virginia). Also, consider if the orders can be signed by a healthcare professional other than a physician. For example, primary care in some institutions and regions of a state may be primarily provided by nurse practitioners or physician assistants. Many programs have adopted regulations specifically authorizing nurse practitioners and physician assistants to be signers of a POLST Paradigm form. This can be a sensitive issue with some state medical associations not wanting other healthcare practitioners to have the authority to sign the form. Your coalition can address this potentially divisive issue, being both aware of and sensitive to your local political climate and existing regulations regarding scope of practice.
7. Train Healthcare Professionals. Intensive educational programs play a vital role in implementation. Train social workers, nurses, emergency medical personnel, chaplains, and others to be advance care planning facilitators to improve their skill and knowledge in discussing, completing, and following the orders on the POLST Paradigm form. A 10-minute video entitled “POLST at Work” is available at www.polst.org and can serve as a useful educational tool to educate frontline staff. Nursing homes with growing Latino populations may also wish to have their staff view a video, “Honoring the Wishes of the Spanish Speaking Patient and Family,” which is also available on the website in both English and Spanish.
8. Program Coordination. Each statewide task force faces unique challenges in considering the best method to coordinate their program long-term, operationally and financially. Some states have chosen academic ethics centers, medical associations, or the department of health, as sometimes mandated by legislation. The best option will vary based on state-specific factors. The necessary components of the system include: (1) standardized practices, policies, and form; (2) trained advance care planning facilitators; (3) timely discussions prompted by prognosis; (4) clear, specific language on an actionable form; (5) a bright form easily found among paperwork; (6) orders honored throughout the system; and (7) quality improvement activities for continual refinement of the form and the system.
9. Distribution Plan. Determine how you plan to distribute the form. In some states, the form is downloadable from a website, with the result that data is not readily available on the extent of the form’s use, and control over printing standards is reduced. In other states, the forms are numbered and distributed from a central office, so there is close monitoring of form usage, but delays may occur in form completion. Other states distribute the forms in bulk to participating LTC facilities, doctors, hospitals, and hospice programs. The method of distribution of the form has obvious financial implications.
10. Review Program Components. We have already reviewed the requirements of a POLST Paradigm Program (also described at: https://www.ohsu.edu/polst/coreform.shtml). If you are developing a program but do not yet meet all the criteria, you are invited to complete the online information and submit to the national coordinating center. Your program information will be included on the website, and the area covered by your program will be colored light pink on the website’s national map. If your program meets the core requirements, you are encouraged to apply on the website for endorsement as a POLST Paradigm Program. Your information is reviewed by the national task force that provides feedback to our program within six weeks. Completing this information is helpful to others in your state and beyond who have similar interests.
11. Relationship with Media. Consider the interface of your program to the media. What message do you want to consistently portray? Which message do you want to avoid? Having individuals on your task force who have good public communication skills can be helpful. Thinking through a media plan and messages in advance can avoid later challenges.
12. Available Resources (see www.polst.org). The National POLST Paradigm Initiative Task Force is available to help you. Pre-courses are being offered at some national meetings, and experienced colleagues in various states are willing to provide consultation. The national task force and website can help facilitate understanding, development, education, and evaluation regarding your program, regardless of your current level of development.
 Recommendation
Recommendation
State leaders in end-of-life care may wish to facilitate implementation of a POLST Paradigm Program at the state level and share these experiences on the www.polst.org website. The program is voluntary, and each state can make adaptations from established programs that respect legal, regional, and cultural differences.
In states lacking a statewide coalition for broad implementation, hospitals, hospices, LTC facilities, EMS, and administrative directors may consider using the POLST Paradigm Program at the regional level in their own facilities and communities. As mentioned, the ultimate goal of a POLST Paradigm Program is to ensure that the wishes of persons with advanced serious illness are honored and respected.
Implementing POLST in Your Facility
Assuming no prohibitions by state laws or regulations, facilities do not need to wait until POLST is implemented within their region or state to begin to use the POLST program. Institutional champions can serve as a catalyst to the introduction and use of POLST through a grass roots approach. Key to this approach is securing administrative, medical, nursing and social service support. Next steps can include developing policies and an education plan, and notifying key contacts such as EMS and nearby hospitals. Partial implementation is often successful, as your team develops skills relating to the use of tools and having discussions with your patients. Because of the progress made in various areas of the county, those who are interested in adopting the POLST Paradigm Program can know that tools and resources are available to facilitate implementation.
The Problem Revisited
 Let’s return to Mrs. J. Imagine instead that the patient’s physician had completed a POLST Paradigm form with orders indicating “Do Not Attempt Resuscitation (DNR/no CPR)” in Section A and “Comfort Measures Only. Do not transfer to hospital for life-sustaining treatment. Transfer if comfort needs cannot be met in current location” in Section B. Following the POLST form, the nursing home’s staff optimizes the patient’s comfort using medications, positioning, and oxygen. The covering physician and daughter are called, who agree with the previously completed POLST orders. The daughter understands that her mother would be transferred to the hospital if for some unexpected reason her mother’s comfort needs cannot be met at the nursing home. Mrs. J dies in comfort the next morning surrounded by her daughter, other family members, and staff who know her well at the nursing home.
Let’s return to Mrs. J. Imagine instead that the patient’s physician had completed a POLST Paradigm form with orders indicating “Do Not Attempt Resuscitation (DNR/no CPR)” in Section A and “Comfort Measures Only. Do not transfer to hospital for life-sustaining treatment. Transfer if comfort needs cannot be met in current location” in Section B. Following the POLST form, the nursing home’s staff optimizes the patient’s comfort using medications, positioning, and oxygen. The covering physician and daughter are called, who agree with the previously completed POLST orders. The daughter understands that her mother would be transferred to the hospital if for some unexpected reason her mother’s comfort needs cannot be met at the nursing home. Mrs. J dies in comfort the next morning surrounded by her daughter, other family members, and staff who know her well at the nursing home.
The challenges that patients, families, and their healthcare professionals face at the end of life can be daunting. Caring and sensitive communication can elicit patients’ wishes and be documented in an advance directive. To put these values into action requires an additional helpful tool, the POLST Paradigm form. Healthcare professionals and their organizations can overcome the myriad barriers to communication across systems of care by developing a POLST Paradigm Program, thereby creating a method that respects some of the most deeply held values of our patients.
The authors report no relevant financial relationships.
Acknowledgment
The authors thank Sarah Foreman and Marian Kemp for help in manuscript preparation.










